Disease ─ Herpes Zoster Oticus
Herpes Zoster Oticus, commonly known as Ramsay Hunt Syndrome, is a viral infection caused by the varicella-zoster virus․ It affects the ear canal, leading to symptoms such as severe ear pain, facial paralysis, blisters, and hearing loss․ Prompt diagnosis and treatment are crucial to prevent complications․

Overview of Herpes Zoster Oticus
Herpes Zoster Oticus, also known as Ramsay Hunt Syndrome, is a rare but serious viral infection that affects the ear․ It is caused by the varicella-zoster virus, the same virus that causes chickenpox and shingles․ The condition primarily targets the facial nerve, leading to symptoms such as severe ear pain, facial paralysis, blisters in the ear canal, and potential hearing loss․
The varicella-zoster virus remains dormant in the body after a chickenpox infection and can reactivate years later as shingles, including in the ear area, causing Herpes Zoster Oticus․ The condition requires prompt medical attention due to the risk of complications involving the cranial nerves, which can result in long-term consequences such as permanent facial paralysis or hearing impairment․
Diagnosis of Herpes Zoster Oticus typically involves a physical examination, medical history review, and possibly imaging tests to assess the extent of nerve involvement․ Early recognition is essential for appropriate management to prevent severe outcomes․ Treatment often includes antiviral medications to combat the viral infection and reduce the risk of nerve damage․
Understanding the signs and symptoms of Herpes Zoster Oticus is critical for timely intervention and optimal recovery․ It is crucial to seek medical advice if you experience ear pain, facial weakness, or other concerning symptoms, as early treatment can help alleviate discomfort and minimize the risk of long-term complications associated with the condition․
Symptoms and Diagnosis
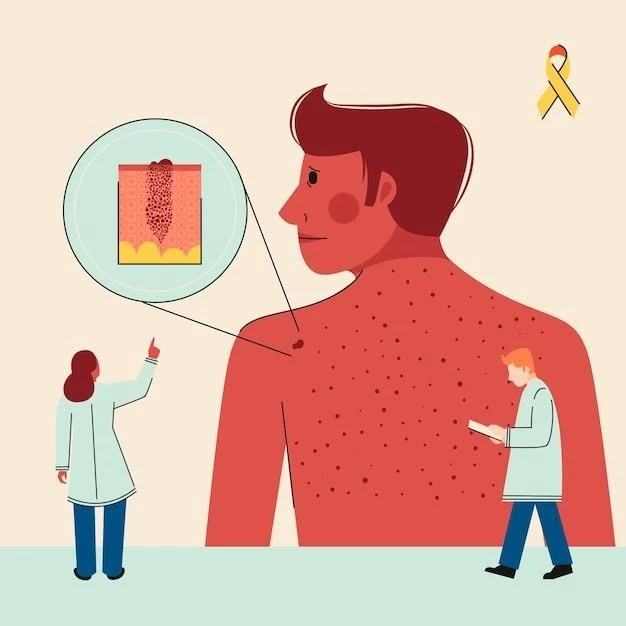
The symptoms of Herpes Zoster Oticus typically manifest as severe ear pain, which can be accompanied by facial paralysis on the same side as the affected ear․ Patients may experience a rash consisting of blisters in or around the ear canal along with hearing loss․ Other common signs include dizziness, vertigo, and an altered sense of taste․
Diagnosing Herpes Zoster Oticus involves a detailed examination of the patient’s medical history and a physical assessment to identify characteristic symptoms such as facial weakness and rash in the ear region․ Healthcare providers may also perform a comprehensive neurological examination to assess cranial nerve function․ In some cases, imaging studies like MRI or CT scans may be recommended to evaluate nerve involvement․
Early recognition of Herpes Zoster Oticus is crucial for prompt initiation of appropriate treatment and reducing the risk of complications․ If you experience sudden onset of severe ear pain, facial paralysis, or other concerning symptoms related to the ear and facial area, it is essential to consult a healthcare professional for a comprehensive evaluation and accurate diagnosis․
Effective management of Herpes Zoster Oticus requires a multidisciplinary approach involving healthcare providers specializing in infectious diseases, otolaryngology, and neurology․ Timely diagnosis enables the implementation of targeted interventions, including antiviral medications, to alleviate symptoms, prevent the spread of the virus, and minimize the potential for long-term sequelae associated with the condition․
Complications of Herpes Zoster Oticus
Herpes Zoster Oticus can lead to various complications, especially if not promptly treated․ One significant complication is persistent nerve pain (neuralgia) in the affected ear, which can be debilitating and impact the quality of life․ Additionally, severe cases of Herpes Zoster Oticus may result in long-term facial paralysis if the facial nerve is extensively damaged during the infection․
Individuals with Herpes Zoster Oticus are also at risk of developing hearing loss, either temporary or permanent, due to damage to the auditory nerves․ The condition can cause significant discomfort and functional impairment, requiring close monitoring and appropriate management to preserve hearing function․ In some instances, patients may experience ongoing dizziness or balance issues post-infection․
Furthermore, untreated Herpes Zoster Oticus can lead to the spread of the viral infection to other cranial nerves, potentially causing complications such as vision problems, taste disturbances, or difficulties with facial movements․ These complications underscore the importance of early intervention and comprehensive treatment to minimize the risk of long-term neurological sequelae․
Complications of Herpes Zoster Oticus highlight the necessity of timely recognition and management of the condition to prevent adverse outcomes․ Healthcare professionals must closely monitor patients with Herpes Zoster Oticus for any signs of worsening symptoms or the development of complications, ensuring that appropriate interventions are implemented promptly to optimize outcomes and reduce the impact of potential long-term sequelae․
Treatment Options
The primary treatment for Herpes Zoster Oticus involves antiviral medications to combat the varicella-zoster virus causing the infection; These medications aim to reduce viral replication, alleviate symptoms, and prevent complications․ Early initiation of antiviral therapy is crucial for optimal outcomes and may include drugs such as acyclovir, valacyclovir, or famciclovir․
In addition to antiviral drugs, healthcare providers may recommend pain management strategies to relieve nerve pain associated with Herpes Zoster Oticus․ Analgesic medications, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate discomfort․ In severe cases of nerve pain, physicians may consider prescribing medications specifically targeting neuropathic pain․
Patients with Herpes Zoster Oticus experiencing significant ear pain or discomfort may benefit from topical treatments or ear drops to alleviate symptoms and promote healing of any blisters in the ear canal․ Proper wound care and infection prevention are essential components of managing the skin lesions associated with the condition․
Individuals with severe cases of Herpes Zoster Oticus or those at risk of complications, such as facial paralysis or hearing loss, may require specialized care from multiple healthcare professionals, including otolaryngologists and neurologists․ Close monitoring and follow-up evaluations are essential to track treatment effectiveness and address any emerging issues promptly․
Overall, the treatment approach for Herpes Zoster Oticus focuses on controlling the viral infection, managing symptoms, and preventing long-term sequelae․ Collaboration between healthcare providers and patients is key to developing a comprehensive treatment plan tailored to individual needs and ensuring the best possible outcomes in managing this viral ear condition․
Management of Symptoms
Managing the symptoms of Herpes Zoster Oticus requires a comprehensive approach to address the various manifestations of the condition․ Patients experiencing severe ear pain can benefit from applying warm compresses to the affected ear to help alleviate discomfort․ It is essential to avoid inserting anything into the ear canal to prevent further irritation․
Facial paralysis associated with Herpes Zoster Oticus may require specialized interventions, including physical therapy and facial exercises to improve muscle strength and function․ Healthcare providers may offer guidance on facial massage techniques to promote recovery and enhance facial nerve regeneration․ Protective eye care measures are essential to prevent complications due to facial muscle weakness affecting eyelid closure․
If blisters or rashes develop in or around the ear canal, proper wound care is essential to prevent infection and facilitate healing․ Keeping the affected area clean and dry can help minimize the risk of secondary complications and promote skin recovery․ Avoiding exposure to irritants or allergens is crucial to prevent further skin irritation and discomfort․
Patients experiencing hearing loss as a result of Herpes Zoster Oticus may benefit from assistive devices or interventions to improve auditory function․ Audiological assessments can help determine the extent of hearing impairment and guide the implementation of appropriate management strategies, such as hearing aids or cochlear implants, if necessary․
Emotional support and counseling may also play a crucial role in the management of symptoms associated with Herpes Zoster Oticus․ Coping strategies, stress management techniques, and support from healthcare professionals or mental health specialists can help individuals navigate the challenges posed by the condition and optimize their overall well-being throughout the recovery process․
Prevention and Outlook
Preventing Herpes Zoster Oticus primarily involves reducing the risk of varicella-zoster virus reactivation through vaccination․ The herpes zoster vaccine, which is recommended for individuals over a certain age, can help lower the likelihood of developing shingles and subsequent complications like Herpes Zoster Oticus․ Maintaining overall health and a robust immune system through regular exercise, a balanced diet, and adequate rest can also contribute to reducing the risk of viral infections․
The outlook for individuals with Herpes Zoster Oticus varies depending on factors such as the timeliness of diagnosis, the severity of symptoms, and the effectiveness of treatment․ Early recognition of the condition and prompt initiation of antiviral therapy can improve outcomes and reduce the risk of long-term complications․ Close monitoring and follow-up care are essential for tracking progress and addressing any lingering symptoms or potential complications․
While some individuals may experience full recovery from Herpes Zoster Oticus with appropriate treatment and symptom management, others may have residual issues such as mild facial weakness or hearing deficits․ The recovery process may be gradual, requiring patience and ongoing support from healthcare providers to optimize outcomes and enhance quality of life․ Long-term sequelae, such as persistent neuralgia or facial nerve damage, are possible but can often be mitigated with timely intervention and comprehensive care․
By prioritizing prevention strategies, seeking timely medical attention, and actively participating in treatment and symptom management, individuals can positively influence their outlook when facing Herpes Zoster Oticus․ Collaborating with healthcare professionals to develop a personalized care plan and adhering to recommended interventions can help minimize the impact of the condition and promote recovery and well-being in those affected by this viral ear disorder․