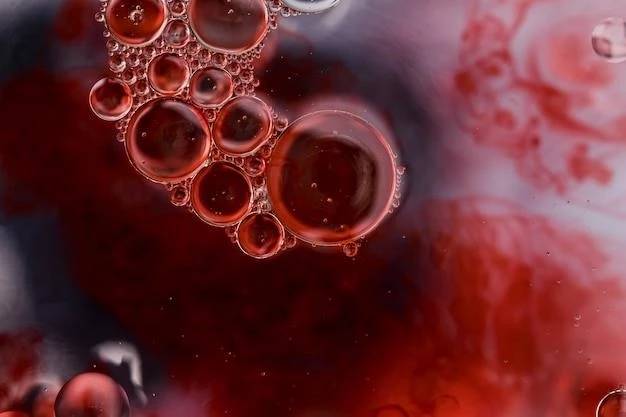
Disease, Hemorrhagic Thrombocythemia
Hemorrhagic thrombocythemia is a rare blood disorder involving excessive production of platelets, leading to blood clotting in blood vessels. Understanding this condition requires insight into hematology and the role of platelets in the body, as well as the causes, symptoms, diagnosis, prognosis, complications, and treatment options available, including medication management and procedures guided by a hematologist.
I. Introduction to Hemorrhagic Thrombocythemia
Hemorrhagic thrombocythemia, also known as essential thrombocythemia, is a rare chronic blood disorder characterized by the overproduction of platelets in the bone marrow. Platelets, also called thrombocytes, are blood cells responsible for blood clotting to prevent excessive bleeding. In individuals with hemorrhagic thrombocythemia, there is an abnormal increase in platelet production, leading to a higher risk of blood clot formation in blood vessels. This condition can affect people of any age, but it is more commonly diagnosed in adults over the age of 50.
The exact cause of hemorrhagic thrombocythemia is often unknown, although genetic mutations may play a role in its development. The disorder is considered a myeloproliferative neoplasm, a group of conditions where the bone marrow produces too many blood cells. As platelets are crucial for normal blood clotting, an excessive number of these cells can lead to abnormal clotting within blood vessels. This abnormal clotting, known as thrombosis, can block blood flow and cause serious complications.
Individuals with hemorrhagic thrombocythemia may experience a range of symptoms, including weakness, fatigue, headaches, dizziness, and numbness or tingling in the hands or feet. Some individuals may also develop bleeding problems due to abnormal platelet function. Diagnosis of hemorrhagic thrombocythemia involves blood tests to measure platelet levels and assess the overall functioning of the blood cells. Additional tests, such as bone marrow biopsy, may be required to confirm the diagnosis and rule out other conditions.
Managing hemorrhagic thrombocythemia involves controlling blood clotting to prevent complications such as strokes, heart attacks, or deep vein thrombosis. Treatment options may include medications to reduce platelet counts and lower the risk of clot formation. In some cases, procedures like platelet apheresis may be recommended to decrease platelet levels rapidly. Regular monitoring by a hematologist is essential to track the progression of the disease and adjust treatment as needed.
Overall, hemorrhagic thrombocythemia is a complex blood disorder that requires careful management and monitoring to prevent serious complications. With proper treatment and ongoing care from a hematologist, individuals with this condition can lead healthy lives and minimize the impact of abnormal blood clotting on their overall health.
II. Understanding Hematology and Blood Disorders
Hematology is the branch of medicine focused on the study of blood and blood disorders. Blood plays a vital role in the body, carrying oxygen, nutrients, and waste products to and from cells. It consists of various components, including red blood cells, white blood cells, platelets, and plasma. Platelets, also known as thrombocytes, are small cell fragments produced in the bone marrow that are essential for blood clotting.
Blood disorders encompass a wide range of conditions that affect the production, function, or composition of blood cells. These disorders can involve abnormalities in red blood cells (anemia), white blood cells (leukemia), platelets (thrombocytopenia), or plasma (clotting disorders). Understanding the different blood components and their roles is crucial for diagnosing and treating blood disorders effectively.
Thrombosis is a common complication seen in various blood disorders, including hemorrhagic thrombocythemia. It refers to the formation of blood clots within blood vessels, which can restrict or block blood flow. When a blood clot forms, it can lead to serious health issues such as heart attacks, strokes, or pulmonary embolisms. Managing blood clotting disorders requires a comprehensive approach that addresses the underlying cause and reduces the risk of clot formation.
Hematologists are medical specialists who diagnose and treat blood disorders. They have extensive training in hematology and are skilled in evaluating blood test results, conducting bone marrow biopsies, and developing treatment plans for patients with blood-related conditions. In the case of hemorrhagic thrombocythemia, hematologists play a crucial role in monitoring platelet levels, managing blood clotting, and preventing complications associated with excessive platelet production.
By studying hematology and understanding blood disorders, healthcare providers can effectively identify and manage conditions like hemorrhagic thrombocythemia. Advances in research and treatment options continue to improve outcomes for individuals with blood disorders, offering hope for better management and quality of life. Collaborating with a hematologist is essential for individuals diagnosed with complex blood disorders, ensuring comprehensive care and tailored treatment plans to address their specific needs.
A. Role of Platelets in the Body
Platelets, also known as thrombocytes, are small cell fragments that play a crucial role in blood clotting, or hemostasis. When a blood vessel is damaged, platelets rush to the site to form a plug and prevent excessive bleeding. This process involves a series of steps that lead to the formation of a stable blood clot, sealing the damaged vessel.
Initially, when blood vessel injury occurs, platelets adhere to the site by sticking to the exposed collagen fibers in the vessel wall. This adhesion triggers the activation of platelets, causing them to change shape and release chemical signals that attract more platelets to the area. As more platelets accumulate, they form a temporary plug that helps stop bleeding.
In addition to adhesion and aggregation, platelets release various substances, such as clotting factors and growth factors, that contribute to the formation of a stable blood clot. Clotting factors help strengthen the clot by forming fibrin strands that weave through the platelet plug, creating a mesh-like structure that traps more platelets and red blood cells.
Once the blood clot is securely in place, it helps seal the wound and allows the damaged blood vessel to heal. Over time, the clot dissolves as the vessel repairs itself, restoring normal blood flow. However, in conditions like hemorrhagic thrombocythemia, where there is an overproduction of platelets, the risk of abnormal blood clot formation increases, leading to potential complications such as thrombosis.
Understanding the role of platelets in maintaining hemostasis is essential for appreciating their significance in preventing excessive bleeding. Balanced platelet function is critical for normal blood clotting and overall cardiovascular health. In cases of blood disorders like hemorrhagic thrombocythemia, where platelet production is dysregulated, careful management is needed to avoid abnormal clotting and related complications.
B. Overview of Thrombosis and Thrombocytes
Thrombosis is the condition characterized by the formation of blood clots within blood vessels, disrupting normal blood flow. These clots can develop in arteries or veins and pose a significant risk to an individual’s health. Thrombocytes, more commonly known as platelets, play a central role in the process of thrombosis and hemostasis to prevent excessive bleeding.
When a blood vessel is injured, platelets are activated and adhere to the site of damage to form a plug, initiating clot formation. This initial platelet plug is essential for temporarily stopping bleeding and initiating the clotting cascade, a series of biochemical reactions that lead to the formation of a stable blood clot.
Platelets release various substances, including clotting factors and growth factors, that promote the progression of clot formation. Clotting factors work together to strengthen the platelet plug by forming fibrin strands that reinforce the clot structure; Additionally, growth factors stimulate cell proliferation and tissue repair at the site of injury.
In conditions like hemorrhagic thrombocythemia, where there is an excess of platelets in the bloodstream, the risk of abnormal clotting events, such as thrombosis, is heightened. The overproduction of platelets can lead to the formation of blood clots that block blood vessels, potentially causing serious complications such as heart attacks, strokes, or pulmonary embolisms.
Treating thrombosis often involves the use of anticoagulant medications that help prevent the formation of new clots or reduce the size of existing clots. Individuals with thrombotic disorders may also need antiplatelet medications to inhibit platelet function and minimize clotting. In severe cases, procedures like thrombectomy or angioplasty may be necessary to remove or bypass blood clots.
Understanding the mechanisms of thrombosis and the role of thrombocytes in blood clotting is essential for managing conditions like hemorrhagic thrombocythemia effectively. By targeting the underlying causes of abnormal clotting and regulating platelet function, healthcare providers can reduce the risk of thrombotic events and improve outcomes for individuals with blood disorders characterized by excessive platelet production.
III. Causes and Risk Factors of Hemorrhagic Thrombocythemia
The exact cause of hemorrhagic thrombocythemia is often unknown, but certain factors may contribute to its development. This condition is classified as a myeloproliferative neoplasm, a group of disorders where the bone marrow produces too many blood cells, including platelets. Genetic mutations, particularly in genes like JAK2٫ CALR٫ and MPL٫ are commonly associated with myeloproliferative neoplasms.
While the specific triggers for these mutations remain unclear, they can lead to the abnormal proliferation of blood cells, including platelets. This overproduction of platelets results in higher-than-normal levels circulating in the bloodstream, increasing the risk of abnormal blood clotting. Age is a significant risk factor for hemorrhagic thrombocythemia, with most cases diagnosed in adults over the age of 50.
Other potential risk factors for developing hemorrhagic thrombocythemia include a family history of myeloproliferative neoplasms, exposure to certain toxins or chemicals, or prior radiation therapy. Individuals who have undergone chemotherapy for other conditions may also have an increased risk of developing blood disorders like hemorrhagic thrombocythemia.
Hemorrhagic thrombocythemia is a rare disorder, and while the causes may vary among individuals, the abnormal increase in platelet production and dysregulation of blood cell growth are central features of the condition. Understanding the genetic and environmental factors that contribute to the development of hemorrhagic thrombocythemia is crucial for early detection, diagnosis, and targeted treatment approaches.
IV. Symptoms of Hemorrhagic Thrombocythemia
Hemorrhagic thrombocythemia, or essential thrombocythemia, can manifest with a variety of symptoms related to abnormal platelet levels and blood clotting. Some individuals with this condition may remain asymptomatic and are diagnosed incidentally through routine blood tests. However, when symptoms do occur, they can vary in severity and may include⁚
- Headaches⁚ Persistent or severe headaches can be a common symptom of hemorrhagic thrombocythemia, often associated with changes in blood flow and platelet levels.
- Fatigue⁚ Excessive tiredness and lack of energy may result from the body’s increased demand for circulating platelets and disruptions in normal blood clotting.
- Dizziness⁚ Feeling lightheaded or dizzy may occur due to changes in blood flow and circulation, potentially affecting oxygen delivery to the brain.
- Numbness or Tingling⁚ Sensations of numbness or tingling, particularly in the hands or feet, can be attributed to altered blood flow and nerve function.
- Bruising or Bleeding⁚ Easy bruising, prolonged bleeding from minor injuries, or nosebleeds are common signs of abnormal platelet function and blood clotting issues.
- Vision Changes⁚ Visual disturbances, such as blurred vision or visual field changes, may occur in some individuals with hemorrhagic thrombocythemia due to altered blood flow to the eyes.
It is essential to note that the symptoms of hemorrhagic thrombocythemia can vary among individuals, and some may experience additional issues like chest pain, abdominal discomfort, or enlarged spleen. Since these symptoms can overlap with other conditions, a comprehensive evaluation by a healthcare provider is necessary for an accurate diagnosis. Monitoring platelet levels through regular blood tests is crucial in managing hemorrhagic thrombocythemia and preventing potential complications associated with abnormal blood clotting.
V. Diagnosis of Hemorrhagic Thrombocythemia
Diagnosing hemorrhagic thrombocythemia involves a series of assessments to evaluate platelet levels, blood cell counts, and overall blood functioning. Healthcare providers may consider the following diagnostic approaches⁚
- Complete Blood Count (CBC)⁚ A CBC test measures the number of platelets, red blood cells, and white blood cells in the blood. Elevated platelet counts may indicate thrombocythemia.
- Peripheral Blood Smear⁚ A blood smear allows for the examination of blood cells under a microscope, providing insights into their size, shape, and distribution.
- Bone Marrow Biopsy⁚ In some cases, a bone marrow biopsy may be performed to assess the production and function of blood cells in the bone marrow.
- JAK2 Mutation Testing⁚ Genetic testing for mutations in the JAK2 gene can help confirm the diagnosis of myeloproliferative neoplasms, including essential thrombocythemia.
- Bone Marrow Aspiration⁚ This procedure involves extracting a sample of bone marrow for analysis, aiding in the diagnosis and classification of blood disorders.
In addition to these tests, healthcare providers may evaluate a patient’s medical history, symptoms, and any family history of blood disorders. It is essential to differentiate hemorrhagic thrombocythemia from other myeloproliferative neoplasms and conditions that can cause similar symptoms, such as polycythemia vera or primary myelofibrosis.
Early diagnosis of hemorrhagic thrombocythemia is crucial for initiating appropriate treatment and minimizing the risk of complications associated with abnormal blood clotting. Regular monitoring of platelet levels and blood tests is essential to track disease progression and treatment response. A collaborative approach involving hematologists and other specialists is often necessary to provide comprehensive care for individuals with hemorrhagic thrombocythemia.
VI. Prognosis and Complications Associated with Hemorrhagic Thrombocythemia
The prognosis for individuals with hemorrhagic thrombocythemia varies depending on various factors, including age at diagnosis, overall health, and response to treatment. While hemorrhagic thrombocythemia is considered a chronic condition, most people with this disorder have a relatively good prognosis with proper management and monitoring.
However, complications can arise due to the abnormal increase in platelet levels and the risk of blood clot formation. Some of the potential complications associated with hemorrhagic thrombocythemia include⁚
- Thrombosis⁚ The formation of blood clots in blood vessels can lead to serious complications such as strokes, heart attacks, or pulmonary embolisms.
- Bleeding Disorders⁚ Abnormal platelet function can result in bleeding problems, including easy bruising, nosebleeds, or prolonged bleeding from minor cuts.
- Enlarged Spleen⁚ The spleen may become enlarged due to the increased number of blood cells, leading to discomfort or pain in the abdomen.
- Secondary Leukemia⁚ In rare cases, individuals with myeloproliferative neoplasms, including hemorrhagic thrombocythemia, may develop secondary leukemias.
Regular monitoring by a hematologist is essential to detect and manage potential complications early. Treatment strategies aimed at controlling platelet levels and preventing abnormal blood clotting can help reduce the risk of complications and improve long-term outcomes for individuals with hemorrhagic thrombocythemia.
With advancements in diagnostic tools and treatment options, individuals with hemorrhagic thrombocythemia can lead productive lives and effectively manage the challenges associated with this rare blood disorder. Collaboration between healthcare providers, including hematologists and other specialists, is key to optimizing care and addressing both the primary condition and any complications that may arise.
VII. Treatment Options for Hemorrhagic Thrombocythemia
Treatment for hemorrhagic thrombocythemia aims to manage platelet levels, reduce the risk of blood clot formation, and alleviate symptoms associated with the condition. The choice of treatment depends on various factors, including the individual’s overall health, age, and the presence of symptoms or complications.
A. Medications for Managing Blood Clotting⁚ Medications are often prescribed to lower platelet counts and prevent abnormal blood clotting. Common medications used in the treatment of hemorrhagic thrombocythemia include⁚
- Aspirin⁚ Low doses of aspirin may be recommended to reduce the risk of blood clots by inhibiting platelet function.
- Hydroxyurea⁚ This medication can help lower platelet counts and decrease the risk of clotting.
- Interferon⁚ Interferon therapy may be used in some cases to regulate blood cell production and manage symptoms.
- Anagrelide⁚ Anagrelide is a medication that can reduce platelet counts by affecting their production in the bone marrow.
B. Procedures to Address Hemorrhagic Thrombocythemia⁚ In certain situations, procedures may be considered to manage hemorrhagic thrombocythemia. These procedures aim to reduce platelet levels quickly and address potential complications. Some common procedures include⁚
- Platelet Apheresis⁚ Apheresis is a procedure that removes platelets from the blood to lower platelet counts rapidly.
- Thrombectomy⁚ Surgical removal of blood clots may be necessary in cases where thrombosis poses a significant risk.
- Radioactive Phosphorus Therapy⁚ This treatment option may be used in select cases to decrease platelet production.
Individuals with hemorrhagic thrombocythemia require ongoing monitoring and treatment adjustments to ensure optimal platelet levels and minimize the risk of complications. Collaborating with a hematologist and other healthcare providers is essential in developing a comprehensive treatment plan tailored to individual needs and ensuring long-term management of this rare blood disorder.
A. Medications for Managing Blood Clotting
Medications play a crucial role in managing hemorrhagic thrombocythemia by controlling platelet levels and reducing the risk of abnormal blood clot formation. Several medications are commonly used to address the underlying mechanisms of the condition and alleviate associated symptoms⁚
- Aspirin⁚ Aspirin is often prescribed in low doses to inhibit platelet aggregation and decrease the likelihood of blood clot formation. By blocking platelet function, aspirin helps prevent excessive clotting in individuals with hemorrhagic thrombocythemia.
- Hydroxyurea⁚ Hydroxyurea is a medication that reduces platelet production in the bone marrow, lowering platelet counts and minimizing the risk of thrombosis. It is commonly used to manage thrombocythemia and improve overall blood flow.
- Interferon⁚ Interferon therapy may be recommended to regulate blood cell production, including platelets, in individuals with hemorrhagic thrombocythemia. By modulating the bone marrow’s activity, interferon can help stabilize platelet levels and reduce symptoms.
- Anagrelide⁚ Anagrelide is a medication that specifically targets platelet production, helping to lower platelet counts in individuals with essential thrombocythemia. By affecting megakaryocyte maturation and platelet release, anagrelide contributes to maintaining appropriate platelet levels.
These medications are prescribed based on individual health factors, disease progression, and response to treatment. Proper monitoring of platelet levels and regular assessments by healthcare providers are essential to adjust medication doses and ensure optimal management of hemorrhagic thrombocythemia.
B. Procedures to Address Hemorrhagic Thrombocythemia
In cases where medication alone is insufficient to manage hemorrhagic thrombocythemia, specific procedures may be considered to address high platelet levels and reduce the risk of complications associated with abnormal blood clotting. These procedures aim to rapidly lower platelet counts and alleviate symptoms⁚
- Platelet Apheresis⁚ Platelet apheresis is a therapeutic procedure that involves removing platelets from the bloodstream. By reducing the number of circulating platelets, this treatment helps lower overall platelet counts quickly, minimizing the risk of clotting events in individuals with hemorrhagic thrombocythemia.
- Thrombectomy⁚ Thrombectomy is a surgical procedure performed to remove blood clots from affected blood vessels. In cases where thrombosis poses a significant risk due to high platelet counts, thrombectomy can help restore normal blood flow and prevent complications such as strokes or heart attacks.
- Radioactive Phosphorus Therapy⁚ Radioactive phosphorus therapy may be utilized to target and decrease the production of platelets in the bone marrow. By selectively impacting the bone marrow’s ability to produce excess platelets, this therapy can aid in controlling platelet levels and managing symptoms of hemorrhagic thrombocythemia.
These procedures are typically performed under the supervision of healthcare professionals experienced in managing blood disorders like hemorrhagic thrombocythemia. The decision to undergo a specific procedure is based on individual health considerations, disease progression, and the presence of complications that may require immediate intervention.
Collaboration between patients, hematologists, and healthcare teams is essential in determining the most appropriate treatment approach for addressing high platelet counts and reducing the risk of thrombotic events in individuals with hemorrhagic thrombocythemia. Regular follow-up visits and monitoring are crucial in ensuring the effectiveness of procedures and maintaining optimal platelet levels over time.
VIII. Role of a Hematologist in Treating Hemorrhagic Thrombocythemia
A hematologist, a medical specialist trained in the diagnosis and treatment of blood disorders, plays a crucial role in managing hemorrhagic thrombocythemia. Their expertise in hematology enables them to provide comprehensive care and individualized treatment plans for patients with this rare blood disorder.
Key aspects of the hematologist’s role in treating hemorrhagic thrombocythemia include⁚
- Diagnosis⁚ Hematologists are skilled in interpreting blood test results, bone marrow biopsies, and genetic tests to accurately diagnose hemorrhagic thrombocythemia and differentiate it from other blood disorders.
- Treatment Planning⁚ Based on the individual’s health status and disease progression, hematologists develop personalized treatment strategies that may include medications, procedures, and ongoing monitoring.
- Medication Management⁚ Hematologists oversee the administration of medications aimed at controlling platelet levels and reducing the risk of abnormal clotting, ensuring proper dosing and monitoring for side effects.
- Procedural Guidance⁚ In cases where procedures like platelet apheresis or thrombectomy are necessary, hematologists provide guidance on when these interventions are appropriate and collaborate with other specialists to optimize outcomes.
- Monitoring and Follow-Up⁚ Regular monitoring of platelet counts, symptoms, and treatment responses is essential in managing hemorrhagic thrombocythemia. Hematologists track disease progression and adjust treatment plans as needed to achieve optimal outcomes.
- Education and Support⁚ Hematologists play a vital role in educating patients about their condition, treatment options, and lifestyle modifications to enhance their overall well-being. They offer support and guidance throughout the treatment journey, addressing concerns and fostering a collaborative relationship with patients.
By working closely with a hematologist, individuals with hemorrhagic thrombocythemia can receive specialized care tailored to their unique needs and ensure effective management of their condition. The hematologist’s expertise, combined with a multidisciplinary approach involving other healthcare providers, optimizes treatment outcomes and quality of life for individuals living with this challenging blood disorder.
