Disease Overview ౼ Hemorrhagic Proctocolitis
Hemorrhagic Proctocolitis‚ also known as Hemorrhagic Ulcerative Colitis‚ is a chronic inflammatory disease that primarily affects the colon and rectum. It is characterized by inflammation‚ ulceration‚ bloody stools‚ abdominal pain‚ diarrhea‚ and flare-ups.
Introduction to Hemorrhagic Proctocolitis
Hemorrhagic Proctocolitis‚ also referred to as Hemorrhagic Ulcerative Colitis‚ is a chronic inflammatory bowel disease marked by inflammation of the colon and rectum. This condition causes ulceration in the lining of the colon and rectum‚ leading to various distressing symptoms.
The exact cause of Hemorrhagic Proctocolitis is not fully understood; however‚ it is believed to involve a combination of genetic‚ environmental‚ and immune system factors. This disease typically exhibits periods of remission and flare-ups‚ which can significantly impact the quality of life of affected individuals.
Individuals with Hemorrhagic Proctocolitis may experience symptoms such as bloody stools‚ abdominal pain‚ diarrhea‚ fatigue‚ and weight loss. The severity of the symptoms can vary from mild to severe and can fluctuate over time.
Management of Hemorrhagic Proctocolitis involves a multidisciplinary approach including medication‚ dietary modifications‚ lifestyle changes‚ and in some cases‚ surgical intervention. Treatment aims to reduce inflammation‚ control symptoms‚ and maintain long-term remission to improve the patient’s quality of life.
It is crucial for individuals with Hemorrhagic Proctocolitis to work closely with healthcare professionals to monitor their condition‚ adjust treatment plans as needed‚ and address any complications that may arise. By understanding this chronic inflammatory bowel disease and its impact‚ individuals can better navigate the challenges associated with Hemorrhagic Proctocolitis.
Understanding the Colon and Rectum
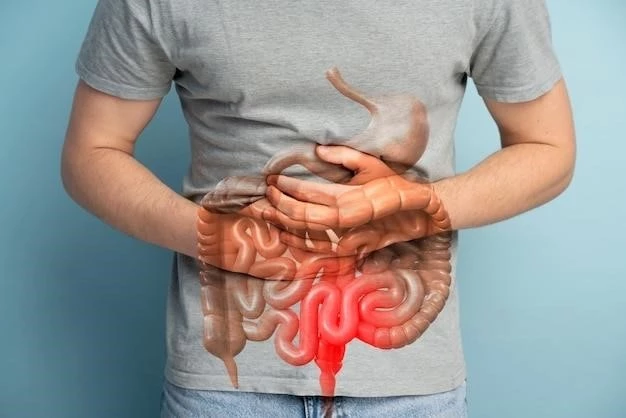
The colon and rectum are vital components of the digestive system. The colon‚ also known as the large intestine‚ plays a key role in absorbing water and electrolytes from digested food‚ while the rectum serves as the final part of the digestive tract where waste material is stored before elimination.
In Hemorrhagic Proctocolitis‚ these regions are specifically affected by inflammation and ulceration. The inflammation in the colon and rectum disrupts their normal function‚ leading to symptoms such as bloody stools‚ abdominal pain‚ and diarrhea.
It is essential to understand the anatomy and function of the colon and rectum to comprehend how Hemorrhagic Proctocolitis can impact these structures. The colon and rectum’s intricate network of tissues and cells can become inflamed and ulcerated in individuals with this chronic inflammatory bowel disease.
By grasping the normal physiology of the colon and rectum‚ individuals can appreciate the challenges faced when these organs are affected by Hemorrhagic Proctocolitis. Understanding the role these organs play in digestion and waste elimination helps patients and healthcare providers better manage the symptoms and complications associated with this condition.
Individuals diagnosed with Hemorrhagic Proctocolitis should work closely with healthcare professionals to monitor the health of their colon and rectum‚ receive appropriate treatment‚ and make lifestyle modifications aimed at alleviating symptoms and improving their overall well-being.
Symptoms and Manifestations
Individuals with Hemorrhagic Proctocolitis may experience a range of symptoms and manifestations that can significantly impact their quality of life. Common symptoms include bloody stools‚ which results from ulceration and inflammation of the colon and rectum.
Abdominal pain is another prevalent symptom‚ often described as cramping‚ sharp‚ or persistent discomfort in the abdomen. Diarrhea is a common manifestation‚ characterized by loose or watery stools that may be frequent and urgent.
Other symptoms of Hemorrhagic Proctocolitis may include fatigue‚ weight loss‚ reduced appetite‚ and anemia due to chronic bleeding in the digestive tract. Additionally‚ individuals may experience flare-ups where symptoms worsen‚ followed by periods of remission where symptoms subside;
It is crucial for individuals experiencing these symptoms to seek medical attention for proper diagnosis and management. Healthcare professionals can conduct diagnostic tests to confirm the presence of Hemorrhagic Proctocolitis and develop a personalized treatment plan based on the severity of symptoms.
By being aware of the symptoms and manifestations of Hemorrhagic Proctocolitis‚ individuals can proactively monitor their health‚ seek timely medical intervention‚ and work towards managing the condition effectively. Close collaboration with healthcare providers is essential to optimize treatment outcomes and improve overall well-being.
Diagnosis and Evaluation
Diagnosing Hemorrhagic Proctocolitis involves a comprehensive evaluation that includes medical history assessment‚ physical examination‚ and diagnostic tests. Healthcare providers may inquire about symptoms‚ family history‚ and overall health to help determine the presence of the condition.
Physical examination may reveal signs such as abdominal tenderness‚ bloating‚ or weight loss consistent with Hemorrhagic Proctocolitis. In addition to a thorough clinical assessment‚ various diagnostic tests are utilized to confirm the diagnosis.
Endoscopic procedures‚ such as colonoscopy and sigmoidoscopy‚ allow healthcare providers to visualize the colon and rectum for signs of inflammation‚ ulceration‚ and bleeding. Biopsy samples may be collected during these procedures for further analysis.
Imaging tests‚ including CT scans and MRI scans‚ are sometimes employed to assess the extent of inflammation and damage to the colon and rectum. Blood tests can help identify markers of inflammation and anemia associated with Hemorrhagic Proctocolitis.
Once a diagnosis is confirmed‚ healthcare providers can establish a treatment plan tailored to the individual’s specific needs. Regular monitoring and evaluation are essential to track disease progression‚ assess treatment effectiveness‚ and make appropriate adjustments to the management approach.
Diagnostic and evaluation processes play a crucial role in managing Hemorrhagic Proctocolitis‚ guiding healthcare providers in providing targeted care and support to individuals affected by this chronic inflammatory bowel disease. Collaboration between patients and healthcare teams is vital in ensuring timely and effective diagnosis and treatment.
Treatment Options
Managing Hemorrhagic Proctocolitis involves a multifaceted approach that combines medication‚ lifestyle modifications‚ and in some cases‚ surgical intervention to alleviate symptoms‚ induce remission‚ and prevent disease progression. The choice of treatment options is tailored to the individual’s specific needs and the severity of the condition.
Medication plays a central role in treating Hemorrhagic Proctocolitis. Anti-inflammatory drugs such as aminosalicylates‚ corticosteroids‚ and immunomodulators are commonly prescribed to reduce inflammation and control symptoms. Biologic therapies‚ including antibodies targeting specific molecules involved in the inflammatory process‚ may be recommended for individuals who do not respond to conventional treatments.
Dietary modifications can also help manage symptoms of Hemorrhagic Proctocolitis. Avoiding trigger foods that exacerbate symptoms‚ focusing on a well-balanced diet rich in nutrients‚ and staying hydrated can support digestive health and overall well-being.
In severe cases or when complications arise‚ surgical intervention may be necessary. Surgery for Hemorrhagic Proctocolitis typically involves removal of the colon and rectum (proctocolectomy) with the creation of an ostomy or an ileal pouch-anal anastomosis to restore digestive continuity.
Complementary therapies such as stress management techniques‚ regular exercise‚ and supportive care from healthcare professionals can complement medical treatments and improve the quality of life for individuals living with Hemorrhagic Proctocolitis.
Regular follow-up appointments with healthcare providers are essential to monitor treatment efficacy‚ assess disease progression‚ and address any emerging issues. Collaborating closely with a healthcare team enables individuals to optimize their treatment plan‚ manage symptoms effectively‚ and work towards long-term wellness.
Living with Hemorrhagic Proctocolitis
Living with Hemorrhagic Proctocolitis requires individuals to adopt strategies that promote overall health‚ manage symptoms‚ and enhance quality of life. It is crucial for patients to work collaboratively with healthcare providers to develop a comprehensive care plan that addresses their unique needs and challenges.

Regular monitoring of symptoms‚ medication adherence‚ and lifestyle modifications are essential components of managing Hemorrhagic Proctocolitis. Patients should stay informed about their condition‚ recognize potential triggers‚ and seek timely medical attention for any changes in symptoms.
Support networks‚ including patient advocacy groups‚ counseling services‚ and educational resources‚ can provide valuable support to individuals coping with Hemorrhagic Proctocolitis. Connecting with others who share similar experiences can offer emotional support and practical tips for navigating life with a chronic inflammatory bowel disease.
Embracing stress-reduction techniques such as mindfulness practices‚ relaxation exercises‚ and seeking professional mental health support can help individuals cope with the emotional challenges associated with Hemorrhagic Proctocolitis. Maintaining a positive outlook‚ setting realistic goals‚ and practicing self-care are vital for overall well-being.
Engaging in regular physical activity‚ following a balanced diet‚ staying hydrated‚ and getting an adequate amount of sleep are key components of living well with Hemorrhagic Proctocolitis. These lifestyle factors can help manage symptoms‚ reduce inflammation‚ and support overall gastrointestinal health.
By taking an active role in their care‚ seeking ongoing support‚ and implementing healthy lifestyle habits‚ individuals with Hemorrhagic Proctocolitis can lead fulfilling lives while effectively managing their condition. With a positive attitude‚ a strong support system‚ and a proactive approach to health‚ living with Hemorrhagic Proctocolitis can be navigated successfully.