Causes of Alcoholic Liver Cirrhosis
Alcoholic liver cirrhosis is primarily caused by chronic alcohol consumption,
Alcohol Consumption
Excessive and prolonged alcohol consumption damages liver cells, leading to inflammation and scarring. The liver metabolizes alcohol, producing harmful byproducts that can cause liver cirrhosis over time.
Genetics
Genetic factors play a role in the susceptibility to alcoholic liver cirrhosis. Variations in genes involved in alcohol metabolism and liver function can influence the risk of developing cirrhosis in individuals with a history of excessive alcohol consumption.
Duration of Alcohol Misuse
The longer the duration of alcohol misuse, the higher the risk of developing alcoholic liver cirrhosis. Prolonged exposure to excessive alcohol leads to cumulative damage to the liver, increasing the likelihood of cirrhosis and other related complications over time.
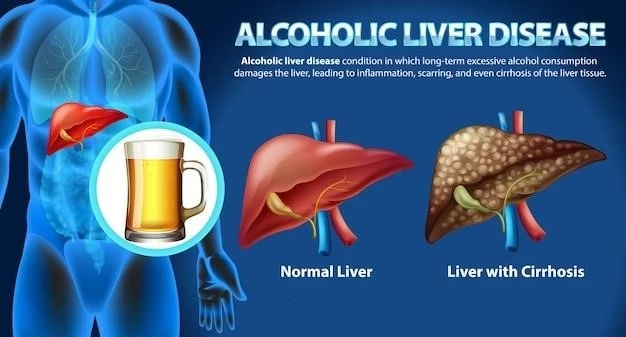
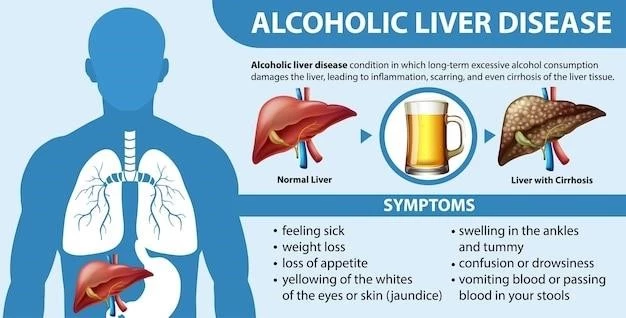
Symptoms of Alcoholic Liver Cirrhosis
Alcoholic cirrhosis may manifest through fatigue, jaundice, and abdominal swelling.
Fatigue and Weakness
Fatigue and weakness are common symptoms of alcoholic liver cirrhosis due to decreased liver function and impaired metabolism. These symptoms can significantly impact daily life and require medical attention.
Jaundice
Jaundice, characterized by yellowing of the skin and eyes, is a common sign of liver dysfunction in alcoholic liver cirrhosis. It results from the buildup of bilirubin in the blood due to impaired liver function.
Abdominal Swelling
Abdominal swelling, known as ascites, is a common symptom of alcoholic liver cirrhosis. It occurs due to fluid buildup in the abdominal cavity as a result of liver dysfunction and portal hypertension, leading to discomfort and increased abdominal girth.
Diagnosis and Treatment of Alcoholic Liver Cirrhosis
Diagnosing ALD may involve imaging tests, blood tests, and liver biopsy.
Diagnostic Tests
Diagnostic tests for ALD include liver function tests, imaging studies like ultrasound and CT scans, and sometimes a liver biopsy to confirm the presence of cirrhosis and assess liver damage.
Medications
Medications for alcoholic liver cirrhosis aim to manage symptoms, prevent complications, and reduce liver inflammation. Treatment may include medications to improve liver function, manage complications like ascites, and address nutritional deficiencies.
Liver Transplantation
Liver transplantation may be considered for advanced cases of alcoholic liver cirrhosis where other treatments are ineffective. It can provide a new, healthy liver to replace the damaged one, offering a chance for improved liver function and overall health.
Lifestyle Changes for Alcoholic Liver Cirrhosis Patients
Adopting a balanced diet, regular exercise, and abstaining from alcohol are key.
Alcohol Cessation
Complete cessation of alcohol consumption is crucial to prevent further liver damage and improve liver function in patients with alcoholic liver cirrhosis. Professional support and counseling may be necessary to maintain sobriety.
Balanced Diet
A well-balanced diet rich in nutrients is essential for managing alcoholic liver cirrhosis. Emphasizing fruits, vegetables, lean proteins, and whole grains can support liver health and overall well-being. Consultation with a healthcare provider or dietitian is recommended for personalized dietary guidance.
Regular Exercise
Regular physical exercise plays a crucial role in managing alcoholic liver cirrhosis. It can help improve overall health, weight management, and energy levels. Consultation with a healthcare provider before starting an exercise regimen is recommended to ensure safety and effectiveness.
Complications of Alcoholic Liver Cirrhosis
Alcoholic liver cirrhosis can lead to serious complications such as portal hypertension.
Portal Hypertension
Portal hypertension is a serious complication of alcoholic liver cirrhosis that results from increased blood pressure in the portal vein. This condition can lead to severe complications such as varices, ascites, and hepatic encephalopathy, necessitating medical management and close monitoring.
Hepatic Encephalopathy
Hepatic encephalopathy is a neurological complication of alcoholic liver cirrhosis characterized by cognitive impairment and altered mental function. It is crucial to manage this condition promptly with medications and dietary modifications to prevent further neurological decline and improve quality of life.
Liver Cancer
Liver cancer, also known as hepatocellular carcinoma, is a severe complication of alcoholic liver cirrhosis. Regular screenings, early detection, and appropriate medical interventions are essential for managing liver cancer in cirrhotic patients and improving treatment outcomes.
Prevention Strategies for Alcoholic Liver Cirrhosis
Preventing ALD involves moderate alcohol consumption, regular health check-ups, and counseling.
Moderate Alcohol Consumption
Practicing moderate alcohol consumption is key to preventing alcoholic liver cirrhosis. Limiting intake and understanding alcohol-related risks can significantly reduce the likelihood of developing liver damage and cirrhosis over time.
Regular Health Check-ups
Regular health check-ups are essential in monitoring liver health and detecting early signs of liver damage. Routine screenings, liver function tests, and consultations with healthcare providers can help prevent and manage alcoholic liver cirrhosis effectively.
Education and Counseling
Education and counseling play a vital role in preventing alcoholic liver cirrhosis. Providing information on the risks of excessive alcohol consumption and offering support for lifestyle changes can empower individuals to make healthier choices and reduce the likelihood of developing liver cirrhosis.
Alcoholic Liver Cirrhosis in Young Adults
Rising trends, challenges in diagnosis, and long-term health impact are vital.
Rising Trends
The increasing prevalence of alcoholic liver cirrhosis among young adults is a concerning trend. Factors such as changing drinking patterns and societal influences contribute to this rise, emphasizing the importance of targeted interventions and education to address this public health issue.
Challenges in Diagnosis
Diagnosing alcoholic liver cirrhosis in young adults poses challenges due to atypical symptoms and potential delays in seeking medical help. Increased awareness among healthcare professionals and the public is crucial for early detection and timely management of this condition in this age group.
Impact on Long-term Health
Alcoholic liver cirrhosis in young adults has significant implications for long-term health, including increased risks of liver failure, liver cancer, and overall morbidity. Early intervention, lifestyle modifications, and regular monitoring are essential in mitigating these long-term health consequences and improving outcomes in this population.
Research Updates on Alcoholic Liver Cirrhosis
Recent studies, promising treatments, and future research directions are critical.
Recent Studies and Findings
Recent studies on alcoholic liver cirrhosis have focused on novel treatment approaches and biomarkers for early detection. Findings provide valuable insights into potential therapeutic strategies and personalized care for patients with this condition.
Promising Treatments in Development
Ongoing research is exploring innovative therapies such as regenerative medicine and targeted drug interventions for alcoholic liver cirrhosis. These developments show promise in improving outcomes and quality of life for individuals with advanced liver disease.
Future Directions in Research
Future research on alcoholic liver cirrhosis aims to deepen our understanding of disease mechanisms, explore personalized treatment approaches, and enhance liver regeneration strategies. By addressing these areas, researchers strive to improve patient outcomes and advance the field of liver disease management.