Disease ⏤ Helminthiasis
Helminthiasis, a disease caused by parasitic worms, poses significant health risks. Understanding its symptoms, transmission, and treatment options is crucial in preventing and controlling infections. This article provides a comprehensive overview of helminthiasis.
Introduction
Helminthiasis is a prevalent infectious disease caused by parasitic worms known as helminths. These worms can infest the human body, leading to various health issues. The most common types of helminths that cause infections in humans include roundworms, tapeworms, and whipworms.
Helminthiasis can affect individuals of all ages, particularly those living in areas with poor sanitation and hygiene practices. The transmission of these parasitic worms usually occurs through contaminated food, water, soil, or contact with infected individuals or animals.
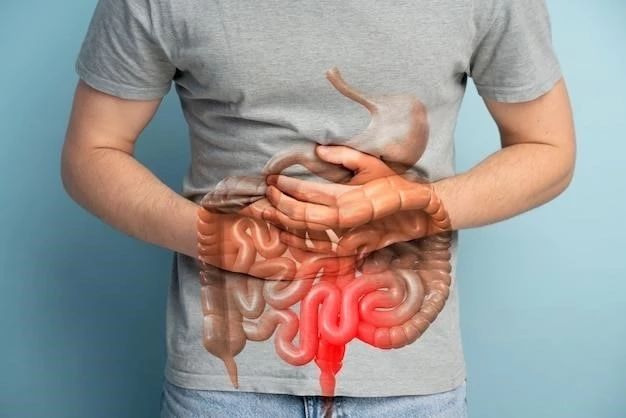
Once inside the human body, helminths can lead to an infestation in the intestines or other organs, causing symptoms such as abdominal pain, diarrhea, weight loss, and fatigue. Proper diagnosis of helminthiasis involves identifying the type of worm through stool tests or imaging studies.
Treatment for helminthiasis often involves medication to eliminate the parasites from the body. Preventive measures, including proper sanitation practices and hygiene, play a crucial role in reducing the risk of infection. Understanding the symptoms, transmission, diagnosis, treatment, and prevention of helminthiasis is essential for public health awareness and disease control.
Overview of Helminthiasis
Helminthiasis, characterized by infections caused by parasitic worms, affects millions of people worldwide, particularly in low-resource settings. These worms, including nematodes, cestodes, and trematodes, can invade the human body through various routes, leading to intestinal or tissue infestations.
Common symptoms of helminthiasis include abdominal discomfort, bloating, anemia, malnutrition, and in severe cases, organ damage. The diagnosis of helminthiasis involves analyzing stool samples for the presence of worm eggs or larvae and may require additional tests such as blood work or imaging studies.
Transmission of helminthiasis occurs through the ingestion of contaminated food or water, contact with infected soil, or through insect vectors. Individuals at higher risk include those living in unsanitary conditions, lacking access to clean water, or engaging in occupations with increased exposure to parasite-infested environments.
Treatment options for helminthiasis typically consist of anthelmintic medications that target and eliminate the worms from the body. In some cases, surgical intervention may be necessary to remove large worms causing blockages or other complications.
Prevention of helminthiasis involves promoting good hygiene practices, ensuring access to safe drinking water, proper sanitation facilities, and deworming programs in endemic areas. Public health efforts focused on education, early detection, and treatment are crucial in reducing the burden of helminth infections and improving overall community health.
Symptoms of Helminthiasis
The symptoms of helminthiasis can vary depending on the type of parasitic worm involved and the location of the infestation in the body. Common signs of helminth infections may include abdominal pain, diarrhea, nausea, vomiting, bloating, and unexplained weight loss.
In cases of severe infestations, individuals may experience anemia, fatigue, weakness, malnutrition, and complications related to the affected organs. Some types of helminths can migrate to different tissues, causing skin rashes, respiratory issues, and neurological symptoms.
Intestinal worms such as roundworms and tapeworms often lead to gastrointestinal symptoms, while tissue-invading parasites like schistosomes can cause liver and bladder problems. The presence of parasites in the body triggers an immune response, which can contribute to inflammation and allergic reactions.
It is essential to recognize the early signs of helminthiasis to seek prompt medical attention and prevent complications. Since symptoms can overlap with other health conditions, a thorough evaluation by healthcare professionals, including stool tests and imaging studies, is necessary for an accurate diagnosis.
Understanding the diverse range of symptoms associated with helminth infections is crucial in distinguishing them from other diseases and initiating appropriate treatment strategies. Public awareness campaigns highlighting the symptoms of helminthiasis can aid in early detection and management, reducing the impact of these parasitic infections on individual health and well-being.
Diagnosis of Helminthiasis
The diagnosis of helminthiasis involves a combination of clinical assessment, laboratory tests, and imaging studies to identify the presence of parasitic worms in the body. Stool examinations are commonly used to detect worm eggs or larvae, aiding in the identification of the specific type of helminth causing the infection.
In cases where intestinal parasites are suspected, a stool sample is collected and analyzed under a microscope for the presence of characteristic worm eggs or segments. Blood tests may also be conducted to assess the impact of the infection on hemoglobin levels, immune response, and organ function.
Imaging techniques such as ultrasound, X-rays, or CT scans may be employed to visualize the location of worms within the body, especially in cases where tissue-invading parasites are involved. Serological tests can detect the presence of antibodies produced in response to certain helminth infections, providing additional diagnostic information.
Healthcare providers carefully evaluate the patient’s symptoms, travel history, and potential exposure to contaminated environments to guide the diagnostic process. Differential diagnosis may be necessary to distinguish helminthiasis from other gastrointestinal or systemic conditions with similar clinical presentations.
Timely and accurate diagnosis of helminthiasis is essential for initiating appropriate treatment interventions and preventing the spread of infection to others. Close collaboration between clinicians, laboratory professionals, and public health authorities is crucial in ensuring effective disease surveillance, diagnosis, and management of helminth infections.
Transmission of Helminthiasis
The transmission of helminthiasis occurs through various routes involving contact with contaminated sources harboring parasitic worms. Ingestion of food or water contaminated with helminth eggs or larvae is a common mode of transmission, particularly in areas with poor sanitation and hygiene practices.
Soil-transmitted helminths such as roundworms, hookworms, and whipworms spread through contact with fecally contaminated soil, where the parasites thrive. Poor hygiene habits, inadequate waste disposal systems, and lack of access to clean water contribute to the transmission of these intestinal worms.
Parasitic worms can also be transmitted through direct skin penetration, as seen in the case of hookworm larvae entering the body through contact with contaminated soil or water. Certain helminths require intermediate hosts such as snails or insects to complete their life cycle before infecting humans, adding complexity to the transmission dynamics.
Individuals living in crowded or unsanitary conditions, including areas with inadequate sewage systems or open defecation practices, are at higher risk of helminthiasis transmission. Occupational exposure to contaminated environments, poor personal hygiene, and lack of preventive measures further increase the likelihood of infection.
Educational campaigns promoting proper hygiene, safe food handling practices, and environmental sanitation are essential in preventing the transmission of helminthiasis. Community-wide efforts to improve water quality, sanitation facilities, and deworming initiatives play a crucial role in reducing the burden of parasitic worm infections and safeguarding public health.
Types of Helminths Causing Infection
Helminthiasis is caused by a diverse group of parasitic worms classified into three main categories⁚ nematodes (roundworms), cestodes (tapeworms), and trematodes (flukes). Each type of helminth exhibits distinct characteristics and life cycles that contribute to the complexity of human infections.
Nematodes, the most common helminths infecting humans, include species such as Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), and hookworms (Ancylostoma duodenale and Necator americanus). These intestinal parasites thrive in the human gastrointestinal tract, causing symptoms ranging from abdominal discomfort to anemia.
Cestodes, represented by tapeworms, are segmented parasites that can reach considerable lengths in the intestines of infected individuals. Examples of human-infecting tapeworms include Taenia solium (pork tapeworm) and Echinococcus granulosus (dog tapeworm), with transmission occurring through ingestion of contaminated food or undercooked meat.
Trematodes, commonly known as liver flukes or blood flukes, belong to the class of digenetic parasites with complex life cycles involving intermediate hosts such as snails or fish. Schistosoma species are notorious for causing schistosomiasis, a debilitating disease prevalent in tropical regions where freshwater snails serve as intermediate hosts.
Each type of helminth presents unique challenges in terms of diagnosis, treatment, and prevention due to their varying life cycles and pathogenic mechanisms. Understanding the distinct characteristics of nematodes, cestodes, and trematodes is essential for healthcare professionals to effectively manage helminth infections and mitigate their impact on public health.
Intestinal Worms
Intestinal worms, known as helminths, are parasitic organisms that infect the gastrointestinal tract of humans, causing a condition known as helminthiasis. Common examples of intestinal worms include roundworms (nematodes), whipworms, and tapeworms (cestodes).
Roundworms such as Ascaris lumbricoides are among the most prevalent intestinal parasites worldwide, with infections often occurring through the ingestion of contaminated food or water. These worms can grow to considerable lengths within the intestines, leading to symptoms such as abdominal pain, malnutrition, and intestinal blockages.
Whipworms (Trichuris trichiura) are named for their whip-like appearance and typically inhabit the large intestine. Infections occur through the ingestion of soil or food contaminated with whipworm eggs. Symptoms may include bloody diarrhea, abdominal discomfort, and weight loss.
Tapeworms, characterized by their segmented bodies, include species like Taenia solium and Taenia saginata. Transmission of tapeworms to humans commonly happens through the ingestion of undercooked or raw meat containing encysted larvae. Symptoms of tapeworm infections may include abdominal pain, weight loss, and segments of the worm in feces.
Intestinal worms disrupt normal digestive functions, leading to nutrient deficiencies, inflammation, and gastrointestinal disturbances. Diagnosis of intestinal worm infections involves stool examinations to identify worm eggs or segments. Treatment typically involves anthelmintic medications to eliminate the parasites from the body.
Preventing intestinal worm infections requires practicing good hygiene, washing hands before eating, cooking meat thoroughly, and avoiding contact with contaminated soil. Public health initiatives promoting deworming programs, sanitation improvements, and health education play a vital role in controlling the spread of intestinal worms and reducing the burden of helminthiasis.
Parasites, Eggs, and Larvae
Helminthiasis, a disease caused by parasitic worms, involves intricate life cycles that include various stages of development such as eggs and larvae. These parasites rely on different hosts and environments to complete their life cycle and continue their reproductive process.
The eggs of helminths are typically produced by adult worms living within the human host’s intestines or other tissues. These eggs are excreted in feces, contaminating the environment and serving as a source of infection for new hosts. Humans can inadvertently ingest helminth eggs through contaminated food, water, or soil.
Once inside the human body, helminth eggs hatch into larvae, initiating the infection process. These microscopic larvae have the potential to migrate through various tissues and organs, causing damage and triggering immune responses. Certain types of helminth larvae can remain dormant in the body for extended periods before developing into adult worms.
The development of helminth larvae often involves intermediate hosts such as snails, insects, or other animals, depending on the species of parasite. For example, schistosomes, which cause schistosomiasis, require freshwater snails as intermediate hosts to complete their life cycle and infect humans through skin contact with contaminated water.
Understanding the life cycles of helminths, including the production of eggs, hatching of larvae, and transmission between hosts, is vital for effective disease control and prevention strategies. Public health programs focused on interrupting the transmission of helminthiasis by targeting the stages of parasites, eggs, and larvae can significantly reduce the burden of these infections on global health.
Risk Factors for Helminthiasis
Several factors contribute to the risk of acquiring helminthiasis, a parasitic infection caused by various worms. Lack of access to clean water and sanitation facilities increases the likelihood of exposure to contaminated sources harboring parasitic eggs or larvae.
Living in areas with poor hygiene practices and inadequate waste management systems raises the risk of helminthiasis transmission. Individuals residing in overcrowded or unsanitary environments, such as slums or refugee camps, face heightened exposure to parasitic worms due to limited access to basic healthcare and preventive measures.
Engaging in activities that involve contact with soil, such as farming, gardening, or playing in dirt, can facilitate the transmission of soil-transmitted helminths like roundworms and whipworms. Occupational exposure to environments contaminated with human or animal waste also poses a risk for helminth infections.
Poor personal hygiene habits, including inadequate handwashing practices, can contribute to the ingestion of helminth eggs present on contaminated surfaces. Consuming undercooked or raw meat infected with tapeworm larvae, common in regions where traditional food preparation methods are prevalent, increases the risk of tapeworm infestations.
Children, especially in low-resource settings, are particularly vulnerable to helminthiasis due to their playful behavior, exploratory nature, and limited understanding of hygiene practices. Pregnant women and individuals with weakened immune systems are also at higher risk of developing severe complications from helminth infections.
Educational campaigns promoting good sanitation, hygiene practices, and deworming initiatives are essential in addressing the risk factors associated with helminthiasis. Improving access to clean water, sanitation facilities, and preventive healthcare services can help mitigate the burden of parasitic worm infections and safeguard public health.
Health Risks Associated with Helminthiasis
Helminthiasis poses significant health risks to affected individuals, impacting various organ systems and overall well-being. Intestinal worms, tissue-invading parasites, and blood flukes can lead to a range of complications and long-term health consequences.
Infestations with intestinal worms like roundworms and whipworms can result in malabsorption of nutrients, leading to malnutrition, growth stunting, and cognitive impairment, particularly in children. Severe cases of intestinal blockages caused by large worm burdens may require surgical intervention.
Tapeworm infections can lead to deficiencies in essential vitamins and minerals, causing weakness, fatigue, and neurological symptoms. In cases of cysticercosis, a complication of Taenia solium infestation, cyst formation in the brain or other tissues can result in seizures, vision problems, and neurological damage.
Tissue-invading helminths such as schistosomes can cause chronic inflammation of the liver, bladder, or intestines, leading to fibrosis, organ dysfunction, and an increased risk of cancer. Blood fluke infections can result in urogenital schistosomiasis, characterized by reproductive health issues and bladder cancer.
Helminthiasis can also trigger immune responses, including allergic reactions and inflammation, exacerbating existing health conditions such as asthma or autoimmune disorders. Chronic infections with parasitic worms can impair the body’s ability to mount effective immune defenses against other pathogens.
Addressing the health risks associated with helminthiasis requires early detection, prompt treatment with anthelmintic medications, and supportive care to manage complications. Public health strategies focused on prevention, deworming programs, and health education aim to reduce the burden of helminth infections and improve health outcomes for affected populations.
Immune Response to Helminth Infections
The immune response to helminth infections is a complex interplay between the host’s immune system and the parasitic worms. Upon infestation, helminths release various antigens and molecules that interact with the host’s immune cells, triggering a multifaceted response.
Helminths have evolved strategies to evade or modulate the host’s immune defenses, allowing them to persist in the body for extended periods. Certain helminths can secrete immunomodulatory factors that suppress inflammation or induce regulatory immune responses, creating a conducive environment for their survival.
The immune response to helminth infections often involves the activation of innate immune cells such as eosinophils, mast cells, and macrophages, which play crucial roles in combating parasitic worms. Eosinophils release toxic granules to target helminths, while mast cells contribute to allergic reactions and tissue repair mechanisms.
Chronic helminthiasis can lead to a state of immune dysregulation characterized by increased levels of regulatory T cells and anti-inflammatory cytokines. This immune profile may dampen the host’s ability to mount effective immune responses to other infections or vaccines, impacting overall immunity.
Helminth-induced immune responses can also result in allergic manifestations, including asthma, eczema, and allergic rhinitis. The influx of eosinophils and IgE antibodies in response to helminth antigens can cross-react with environmental allergens, exacerbating allergic symptoms in infected individuals.
Understanding the immune response dynamics during helminth infections is essential for developing novel treatment strategies and vaccines that target both the parasites and the host immune system. Research into immunomodulatory mechanisms employed by helminths may provide insights into harnessing the immune response for therapeutic interventions against these parasitic infections.
Treatment Options for Helminthiasis
The treatment of helminthiasis typically involves the use of anthelmintic medications designed to eliminate parasitic worms from the human body. Depending on the type of helminth infection and the severity of symptoms, different classes of anthelmintics may be prescribed by healthcare providers.
For intestinal worms such as roundworms, whipworms, and hookworms, common anthelmintic drugs like albendazole, mebendazole, or pyrantel pamoate are often recommended. These medications work by disrupting the worms’ ability to absorb nutrients, leading to their expulsion from the intestines.
Tapeworm infections may require specific anthelmintics such as praziquantel or niclosamide, which target the tapeworm’s physiology and structure. These medications are effective in killing adult tapeworms and preventing further growth and reproduction within the intestines.
Tissue-invading parasites like schistosomes may necessitate a different approach to treatment, including the use of praziquantel to target the blood flukes at various stages of their life cycle. This drug is highly effective against adult schistosomes and is often used in mass drug administration programs to control schistosomiasis.
In cases of severe helminth infestations or complications, surgical interventions may be required to remove large worms causing blockages or damage to internal organs. Surgical procedures aim to extract the worms and repair any tissue damage resulting from the parasitic infection.
Combating helminthiasis also involves supportive care to manage symptoms such as abdominal pain, nutritional deficits, and anemia associated with worm infestations. Rehydration therapy, nutritional supplementation, and monitoring for potential complications are essential components of comprehensive treatment for helminthiasis.
Effective treatment of helminth infections not only alleviates symptoms but also prevents the spread of parasitic worms to others. Healthcare professionals play a crucial role in diagnosing, prescribing appropriate medications, and monitoring the response to treatment to ensure successful eradication of helminths and restoration of patient health.
Medication for Helminthiasis
Medications used in the treatment of helminthiasis, parasitic infections caused by worms, play a crucial role in eliminating the parasites from the human body. Anthelmintic drugs are specifically designed to target different types of helminths and disrupt their life cycles, promoting recovery and preventing further complications.
Primary anthelmintic medications for common intestinal worms like roundworms, whipworms, and hookworms include albendazole, mebendazole, and pyrantel pamoate. These drugs are administered orally and work by interfering with the worms’ metabolism, leading to paralysis and expulsion from the intestines.
For tapeworm infections, praziquantel and niclosamide are the recommended anthelmintics. Praziquantel is particularly effective against adult tapeworms, causing damage to their outer layers and facilitating their removal from the intestines through the host’s digestive processes.
Schistosomiasis, caused by blood flukes known as schistosomes, is treated with praziquantel, which targets the parasite’s nervous system and muscular activity. Praziquantel is highly effective in killing adult schistosomes and reducing the burden of infection in endemic areas through mass drug administration programs.
Administration of anthelmintic medications for helminth infections requires careful dosing, considering the patient’s age, weight, and overall health status. Follow-up assessments and repeat treatments may be necessary to ensure complete eradication of the parasites and prevent reinfection.
Side effects from anthelmintic medications are generally mild and may include gastrointestinal disturbances, headaches, and fatigue. Monitoring for adverse reactions and providing supportive care as needed are essential components of helminthiasis treatment to ensure patient comfort and compliance.
Selection of the appropriate anthelmintic drug, dosage regimen, and treatment duration are guided by the specific type of helminth infection, the severity of symptoms, and any existing medical conditions in the patient. Healthcare professionals play a pivotal role in prescribing and managing medication therapy for helminthiasis to promote successful outcomes and improve patient well-being.

Sanitation Practices
Sanitation practices play a pivotal role in preventing and controlling helminthiasis, a disease caused by parasitic worm infections. Implementing effective sanitation measures can significantly reduce the transmission of helminths and safeguard public health in communities at risk of infestation.
Ensuring access to clean water sources is essential in preventing contamination with helminth eggs or larvae. Promoting proper water treatment, storage, and hygiene practices can minimize the risk of ingesting waterborne parasites, particularly in areas lacking reliable sanitation infrastructure.
Proper waste management practices, including safe disposal of human and animal feces, are critical in preventing the spread of intestinal worms like roundworms and hookworms in the environment. Building adequate latrines, sewage systems, and waste treatment facilities can limit the exposure to parasitic infections.
Hygiene education programs focused on handwashing with soap, especially before handling food or after using the toilet, can reduce the risk of helminthiasis transmission through contaminated hands. Teaching children and adults about proper hygiene practices is fundamental in breaking the cycle of infection.
Avoiding the consumption of raw or undercooked meat and fish, which may contain encysted larvae of tapeworms, is another important sanitation measure to prevent tapeworm infections. Proper cooking techniques and food hygiene practices can eliminate the risk of acquiring parasitic diseases from contaminated foods.
Safe agricultural practices, such as minimizing soil contact and using protective gear when working in parasite-infected areas, can help prevent soil-transmitted helminthiasis. Implementing deworming programs for livestock and pets also reduces the risk of zoonotic helminth infections in humans.
Community-wide efforts to improve sanitation practices, access to clean water, and hygiene behaviors are essential in reducing the burden of helminthiasis and promoting overall health and well-being. Public health initiatives focused on sanitation infrastructure development, education, and behavioral change interventions are key components of successful helminthiasis control programs.