Disease ⏤ Exogenous Lipoid Pneumonia
Exogenous Lipoid Pneumonia is a medical condition characterized by the accumulation of lipid-laden macrophages in the alveoli, leading to respiratory inflammation․ This disorder is caused by the aspiration or inhalation of fatty substances which can result in pulmonary illness․
Overview of Exogenous Lipoid Pneumonia
Exogenous Lipoid Pneumonia is a rare respiratory condition characterized by the accumulation of lipid-laden macrophages in the alveoli, caused by the inhalation or aspiration of fatty substances․ These lipids trigger an inflammatory response in the lungs, leading to pulmonary illness․ The disorder can manifest acutely or chronically, and its severity can vary from mild symptoms to life-threatening complications․
Exogenous Lipoid Pneumonia is typically classified into two main types⁚ acute and chronic․ Acute episodes often present with sudden onset symptoms such as cough, chest pain, shortness of breath, and fever, while chronic cases may have a more insidious presentation with gradual respiratory decline and systemic manifestations․
Diagnosis of Exogenous Lipoid Pneumonia requires a thorough clinical evaluation, including imaging studies like chest X-rays or CT scans to assess the extent of lung involvement․ Treatment approaches range from supportive care to more aggressive interventions such as bronchoscopy to remove the lipid-laden material․ Complications associated with this condition include respiratory failure, lung abscess formation, and chronic respiratory insufficiency․
As research in the field advances, new strategies for the prevention and management of Exogenous Lipoid Pneumonia are being developed․ Understanding the pathophysiology of the disease is crucial in improving patient outcomes and reducing the burden of this rare but potentially severe pulmonary disorder․
Causes and Risk Factors
Exogenous Lipoid Pneumonia is primarily caused by the inhalation or aspiration of external substances containing fatty components, such as mineral oil, petroleum jelly, or certain medications․ These substances can enter the respiratory tract and reach the alveoli, where they disrupt normal lung function and trigger an inflammatory response․
Several risk factors contribute to the development of Exogenous Lipoid Pneumonia, including occupations that involve exposure to airborne lipid-containing substances, improper administration of oily medications via inhalation or aspiration, and certain cultural practices like oil pulling․ Individuals with conditions that affect swallowing or lung clearance mechanisms are also at higher risk of developing this disorder․
It is essential for healthcare providers to consider the occupational and environmental history of patients presenting with respiratory symptoms, as well as their medication use and lifestyle practices, to identify potential causes of Exogenous Lipoid Pneumonia․ Educating individuals on safe handling of lipid-containing substances and promoting proper administration of medications can help reduce the incidence of this rare pulmonary illness․
Understanding the specific causes and risk factors associated with Exogenous Lipoid Pneumonia is crucial in both preventing the condition and guiding appropriate diagnostic and treatment strategies for affected individuals․ By addressing these underlying factors, healthcare professionals can improve outcomes for patients with this unique form of pulmonary disease․
Pathophysiology of Exogenous Lipoid Pneumonia
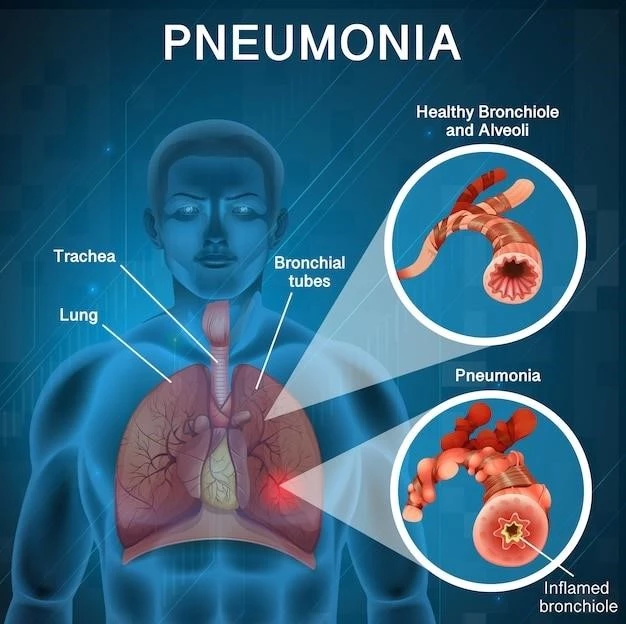
The pathophysiology of Exogenous Lipoid Pneumonia involves the deposition of lipid material in the alveoli of the lungs, leading to inflammation and respiratory dysfunction․ When lipid-containing substances are inhaled or aspirated, they can be phagocytosed by alveolar macrophages, forming lipid-laden macrophages․
These lipid-laden macrophages trigger an immune response, releasing pro-inflammatory mediators that attract more immune cells to the site of injury․ This cascade of inflammatory processes contributes to the development of respiratory symptoms and lung damage seen in Exogenous Lipoid Pneumonia․
Over time, the accumulation of lipid-laden macrophages in the alveoli can impair gas exchange, leading to hypoxemia and respiratory distress․ The presence of excess lipids in the lung tissue can also disrupt the normal architecture of the airways and alveoli, further compromising lung function․
Understanding the pathophysiology of Exogenous Lipoid Pneumonia is essential for developing effective treatment approaches that target the inflammatory response and promote the clearance of lipid material from the lungs․ By unraveling the mechanisms underlying this condition, researchers and clinicians can explore novel therapeutic strategies to improve outcomes for individuals affected by this rare pulmonary disorder․
Symptoms and Clinical Presentation
The symptoms and clinical presentation of Exogenous Lipoid Pneumonia can vary depending on the duration and severity of the condition․ Acute cases may present with sudden onset symptoms such as cough, chest pain, shortness of breath, fever, and fatigue․ Patients may also experience respiratory distress and cyanosis in severe cases․
Chronic Exogenous Lipoid Pneumonia often manifests with more insidious symptoms, including progressive shortness of breath, chronic cough, weight loss, and recurrent respiratory infections․ Patients may exhibit signs of respiratory failure, such as decreased oxygen saturation levels and respiratory distress on exertion․
In some individuals, Exogenous Lipoid Pneumonia can be asymptomatic or present with nonspecific symptoms that mimic other respiratory conditions, making diagnosis challenging․ Clinical examination may reveal crackles on auscultation, dullness to percussion over affected lung areas, and signs of respiratory compromise․
Early recognition of the symptoms and clinical features of Exogenous Lipoid Pneumonia is crucial for prompt diagnosis and appropriate management․ Healthcare providers should maintain a high index of suspicion for this rare pulmonary disorder, especially in individuals with a history of lipid exposure or risk factors predisposing them to the condition․
Diagnosis of Exogenous Lipoid Pneumonia
Diagnosing Exogenous Lipoid Pneumonia requires a comprehensive approach that includes clinical assessment, imaging studies, and laboratory tests․ Chest X-rays are often the initial diagnostic tool used to identify abnormalities in the lungs, such as consolidations, opacities, or ground-glass infiltrates suggestive of lipid-laden material․
Computed tomography (CT) scans provide detailed images of the lung parenchyma and can reveal characteristic findings of Exogenous Lipoid Pneumonia, such as crazy-paving patterns, nodules, or areas of parenchymal consolidation․ These imaging studies help assess the extent of lung involvement and guide further diagnostic workup․
Bronchoscopy with bronchoalveolar lavage (BAL) is a crucial diagnostic procedure for confirming the presence of lipid-laden macrophages in the alveoli․ BAL fluid analysis can reveal an increased lipid-laden macrophage content, supporting the diagnosis of Exogenous Lipoid Pneumonia․
Laboratory tests, including complete blood count (CBC), blood gas analysis, and pulmonary function tests, help evaluate the patient’s respiratory status and overall lung function․ In cases where the diagnosis remains uncertain, a lung biopsy may be performed to obtain tissue samples for histopathological examination․
Given the nonspecific nature of the symptoms associated with Exogenous Lipoid Pneumonia, a multidisciplinary approach involving pulmonologists, radiologists, and pathologists is essential for an accurate diagnosis․ Timely recognition and confirmation of this condition facilitate appropriate treatment interventions and improve patient outcomes․
Treatment Approaches
The management of Exogenous Lipoid Pneumonia involves a combination of supportive care, pharmacological interventions, and procedural therapies tailored to the individual patient’s clinical presentation․ In cases where the condition is mild and asymptomatic, observation and monitoring may be sufficient․
Symptomatic treatment focuses on alleviating respiratory distress and addressing underlying inflammation․ Oxygen therapy is often administered to maintain adequate oxygen saturation levels, while bronchodilators may be used to relieve bronchospasm and improve airway patency․
Corticosteroids may be prescribed to reduce lung inflammation and suppress the immune response in more severe cases of Exogenous Lipoid Pneumonia․ These medications help mitigate the inflammatory cascade triggered by lipid accumulation in the alveoli, facilitating symptom resolution․
In instances where there is a significant burden of lipid-laden material in the lungs, bronchoscopy with bronchoalveolar lavage (BAL) or therapeutic lavage may be necessary to remove the obstructing substance․ This procedure helps clear the airways of lipid-laden macrophages, promoting lung recovery․
Long-term management of Exogenous Lipoid Pneumonia involves monitoring respiratory function, addressing any complications, and promoting lung health through smoking cessation, respiratory therapy, and vaccination against respiratory infections․ Multidisciplinary collaboration between pulmonologists, respiratory therapists, and other healthcare providers is essential for optimizing patient care and outcomes․
Complications Associated with Exogenous Lipoid Pneumonia
Exogenous Lipoid Pneumonia can lead to various complications that impact respiratory function and overall health․ One of the primary complications of this condition is respiratory failure, where the impaired gas exchange in the lungs causes a decrease in oxygen levels and an increase in carbon dioxide levels in the blood․
Prolonged inflammation and the presence of lipid-laden material in the alveoli can contribute to the development of lung abscesses, which are pockets of infected and necrotic lung tissue․ These abscesses can lead to worsening respiratory symptoms, systemic infection, and potential lung damage if left untreated․
Chronic Exogenous Lipoid Pneumonia can result in progressive lung fibrosis, where the lung tissue becomes thickened and scarred, leading to irreversible damage and compromised lung function․ This fibrotic process can significantly impact the quality of life and long-term prognosis of affected individuals․
Recurrence of lipid aspiration or inadequate treatment of Exogenous Lipoid Pneumonia may predispose patients to recurrent respiratory infections, exacerbating the underlying lung pathology and increasing the risk of further complications․ Complications associated with this condition require close monitoring and prompt intervention to prevent adverse outcomes and preserve lung health․
Prognosis and Outlook
The prognosis of Exogenous Lipoid Pneumonia varies depending on the severity of the condition, the timeliness of diagnosis, and the effectiveness of treatment interventions․ In mild cases with prompt recognition and management, individuals may experience complete resolution of symptoms and lung function restoration․
However, in more severe or advanced cases of Exogenous Lipoid Pneumonia, the prognosis can be guarded, especially in instances where complications such as respiratory failure, lung abscess formation, or progressive fibrosis occur․ Long-term outcomes may be influenced by the extent of lung damage and the presence of underlying comorbidities․
Early diagnosis and appropriate treatment are crucial factors in improving the prognosis of Exogenous Lipoid Pneumonia; Multidisciplinary care involving pulmonologists, respiratory therapists, and other specialists can enhance patient outcomes by ensuring comprehensive management and monitoring of the condition․
Individuals who have experienced Exogenous Lipoid Pneumonia may benefit from long-term respiratory follow-up to assess lung function, monitor for potential complications, and provide ongoing support for respiratory health․ Prognosis and outlook for patients with Exogenous Lipoid Pneumonia can be optimistic with diligent medical care and proactive management strategies․
Prevention Strategies
Preventing Exogenous Lipoid Pneumonia involves implementing measures to reduce the risk of inhaling or aspirating lipid-containing substances and promoting respiratory health․ Occupational safety protocols should be followed to minimize exposure to airborne lipid particles in industries where such substances are used․
Proper handling and storage of lipid-based products, including mineral oils, petroleum jelly, and oily medications, are essential to prevent accidental ingestion or inhalation․ Labels on containers should provide clear instructions for safe use and storage, reducing the likelihood of exposure to these substances․
Healthcare providers play a key role in preventing Exogenous Lipoid Pneumonia by ensuring correct administration of lipid-based medications and educating patients on the risks of inhalation or aspiration․ Counseling individuals with swallowing difficulties on aspiration precautions can help prevent lipid-induced lung injury․
Community awareness campaigns and public health initiatives can raise awareness about the risks associated with lipid aspiration and promote safe practices in handling lipid-containing substances․ Encouraging smoking cessation, maintaining good respiratory hygiene, and staying up to date on respiratory vaccinations are also important preventive measures․
By adopting preventive strategies at the individual, healthcare, and community levels, the incidence of Exogenous Lipoid Pneumonia can be reduced, ultimately contributing to better respiratory health outcomes and improved quality of life for individuals at risk of this rare pulmonary condition․
Research and Recent Developments
Ongoing research in the field of Exogenous Lipoid Pneumonia has focused on elucidating the underlying mechanisms of lipid-induced lung injury, exploring novel diagnostic approaches, and evaluating emerging treatment modalities to enhance patient outcomes․ Recent studies have highlighted the importance of early recognition and management of this rare pulmonary disorder․
Advancements in imaging technologies, such as high-resolution computed tomography (HRCT) and magnetic resonance imaging (MRI), have facilitated the identification of characteristic radiological patterns associated with Exogenous Lipoid Pneumonia, aiding in more accurate and timely diagnosis․ These imaging modalities provide valuable insights into the extent of lung damage and the response to treatment․
Immunohistochemical analyses of lung tissue samples have contributed to a better understanding of the inflammatory pathways and cellular responses involved in Exogenous Lipoid Pneumonia․ Targeted therapies that modulate immune reactions and promote lipid clearance from the lungs are being investigated as potential treatment options for this condition․
Clinical trials evaluating the efficacy of corticosteroids, bronchoscopy-assisted therapies, and adjunctive treatments in Exogenous Lipoid Pneumonia are underway to establish evidence-based guidelines for optimal management․ Collaborative efforts between researchers, healthcare professionals, and patient advocacy groups are essential for advancing knowledge and improving clinical outcomes in individuals affected by this respiratory illness․
Future research directions in Exogenous Lipoid Pneumonia aim to enhance preventative strategies, refine diagnostic algorithms, and personalize treatment regimens based on individual patient characteristics․ By integrating research findings into clinical practice, the medical community can optimize care for individuals with this unique form of lipid-related pulmonary disease․
Case Studies and Real-Life Examples
Case studies of Exogenous Lipoid Pneumonia have demonstrated the diverse clinical presentations and outcomes associated with this condition․ A recent report described a case of a 45-year-old male who presented with acute respiratory distress and was found to have lipid-laden macrophages on bronchoalveolar lavage, confirming the diagnosis․
In another real-life example, a 62-year-old female with a history of chronic mineral oil ingestion for constipation developed chronic cough٫ weight loss٫ and progressive dyspnea․ Imaging studies revealed bilateral pulmonary infiltrates consistent with Exogenous Lipoid Pneumonia٫ highlighting the importance of recognizing the systemic effects of lipid aspiration․
Case reports have also underscored the challenges in diagnosing Exogenous Lipoid Pneumonia, particularly in patients with atypical symptoms or nonspecific radiological findings․ A case study of a 55-year-old individual with recurrent pneumonia revealed delayed diagnosis of Exogenous Lipoid Pneumonia due to overlapping clinical features with other respiratory conditions․
Real-life examples of Exogenous Lipoid Pneumonia emphasize the significance of a thorough patient history, including occupational exposures, medication use, and cultural practices, in identifying potential risk factors for lipid aspiration․ These cases highlight the importance of a multidisciplinary approach to diagnosis and treatment to improve patient outcomes․
By documenting and sharing compelling case studies, clinicians and researchers can enhance awareness of Exogenous Lipoid Pneumonia, refine diagnostic criteria, and inform evidence-based therapeutic strategies for individuals affected by this unique pulmonary disorder․
Conclusion
In conclusion, Exogenous Lipoid Pneumonia is a rare but potentially serious pulmonary disorder characterized by the accumulation of lipid-laden macrophages in the alveoli, leading to respiratory inflammation and dysfunction․ The inhalation or aspiration of fatty substances can trigger this unique form of lung injury, presenting with a spectrum of acute and chronic symptoms․
Diagnostic approaches encompass a comprehensive evaluation, including imaging studies, bronchoscopy, and lung biopsy, to confirm the presence of lipid-induced lung injury․ Treatment strategies aim to alleviate respiratory symptoms, reduce inflammation, and promote the clearance of lipid material from the lungs․
Complications associated with Exogenous Lipoid Pneumonia, such as respiratory failure, lung abscess formation, and lung fibrosis, underscore the importance of early recognition and intervention․ Prognosis and outlook depend on the timely diagnosis, appropriate management, and the presence of any underlying comorbidities․
Preventive measures, including safe handling of lipid-containing substances, patient education, and occupational safety guidelines, are key in reducing the risk of Exogenous Lipoid Pneumonia․ Research advancements are continuously improving our understanding of this condition, paving the way for enhanced diagnostic modalities and innovative treatment options․
By integrating knowledge from case studies, research developments, and clinical experiences, healthcare professionals can optimize care for individuals with Exogenous Lipoid Pneumonia, ultimately striving for improved outcomes, enhanced quality of life, and a better understanding of this complex pulmonary disorder․