Disease ⎻ Essential Iris Atrophy
Introduction to Essential Iris Atrophy (EIA)
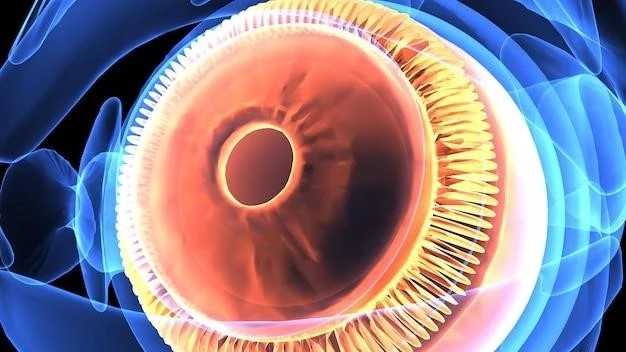
Essential Iris Atrophy (EIA) is a rare ocular disorder characterized by changes in the iris tissue. It is often associated with other conditions such as pigment dispersion syndrome, posterior polymorphous dystrophy, and iris transillumination defects. EIA can result in various clinical manifestations, including iris sphincter atrophy, pseudophakia, and intraocular pressure fluctuations.
The pathophysiology of EIA involves abnormalities in the iris leading to structural changes and pigmentation alterations. These changes can impact the functionality of the iris, causing symptoms such as ocular hypertension, corneal endothelial cell loss, and increased risk of developing glaucoma and cataracts. Early diagnosis and management of EIA are crucial to prevent further complications and preserve ocular health.
Understanding the etiology, clinical features, and diagnostic criteria of EIA is vital for healthcare professionals to provide optimal care for patients affected by this condition. Research into advancements in EIA treatment continues to improve outcomes and enhance the long-term prognosis for individuals with Essential Iris Atrophy.
Etiology and Pathophysiology of EIA
Essential Iris Atrophy (EIA) has a multifactorial etiology involving genetic predisposition and environmental factors. The pathophysiology of EIA is complex, encompassing structural changes in the iris tissue and alterations in pigment dispersion; Genetic studies have identified potential gene mutations that may contribute to the development of EIA.
The primary pathological mechanism underlying EIA is the degeneration and atrophy of iris sphincter muscle fibers, leading to iris thinning and structural weakness. This can result in iris transillumination defects, causing light to pass through the iris abnormally. Pigment dispersion syndrome and posterior polymorphous dystrophy are conditions often associated with EIA, further complicating its etiology.
Abnormalities in the iris architecture disrupt the normal flow of aqueous humor in the eye, contributing to intraocular pressure fluctuations and potential glaucoma development. The compromised iris structure also impacts the corneal endothelial cells, leading to cell loss and potential visual disturbances.
Understanding the intricate interplay between genetic predisposition, environmental factors, and structural changes in the iris is key to elucidating the etiology and pathophysiology of Essential Iris Atrophy. Further research into the underlying mechanisms driving EIA progression is essential for developing targeted treatment strategies and improving patient outcomes.
Clinical Features of EIA
Essential Iris Atrophy (EIA) presents with a spectrum of clinical features that reflect the underlying structural and functional changes in the iris. Patients with EIA may exhibit iris sphincter atrophy, characterized by a thinning and weakening of the iris tissue. This can manifest as irregular or constricted pupil shape, impacting light transmission and visual acuity.
Iris transillumination defects are commonly observed in individuals with EIA, where light passes through the iris due to its thinning and decreased pigment content. Pseudophakia, the presence of an artificial lens in the eye, is a frequent finding in EIA patients who have undergone cataract surgery, further complicating the clinical picture.
Intraocular pressure fluctuations are a hallmark feature of EIA, as the structural changes in the iris can impact the drainage pathways of aqueous humor, leading to ocular hypertension and increasing the risk of glaucoma development. Corneal endothelial cell loss may also occur secondary to these pressure changes, potentially resulting in corneal edema and visual disturbances.
Recognizing the diverse clinical manifestations of EIA is essential for accurate diagnosis and appropriate management strategies. Healthcare providers must be vigilant in identifying these features to initiate timely interventions and prevent further complications associated with Essential Iris Atrophy.
Diagnosis of EIA
Diagnosing Essential Iris Atrophy (EIA) involves a comprehensive ophthalmic evaluation to identify characteristic signs and symptoms associated with the condition. Clinical examination of the iris for features such as sphincter atrophy, transillumination defects, and pseudophakia is crucial in the diagnostic process.
Specialized imaging techniques, including anterior segment optical coherence tomography (AS-OCT) and slit-lamp biomicroscopy, can provide detailed visualization of iris morphology and structural changes indicative of EIA. AS-OCT enables the assessment of iris thickness and integrity, aiding in the diagnosis and monitoring of disease progression.
Furthermore, assessing intraocular pressure and performing visual field testing are essential components of the diagnostic workup for EIA. Patients with EIA often exhibit fluctuations in intraocular pressure due to impaired aqueous humor dynamics, necessitating regular monitoring to detect and manage ocular hypertension.
A thorough review of the patient’s medical history, including a family history of ocular disorders, can provide valuable insights into the genetic predisposition for EIA. Genetic testing may be considered in certain cases to identify specific gene mutations associated with the development of Essential Iris Atrophy.
Collaboration between ophthalmologists and other healthcare professionals is paramount in the accurate diagnosis of EIA. A multidisciplinary approach ensures comprehensive evaluation, timely intervention, and personalized management strategies tailored to address the unique needs of patients with this rare ocular condition.
Management of EIA
The management of Essential Iris Atrophy (EIA) focuses on addressing the underlying causes, alleviating symptoms, and preventing complications associated with the condition. Treatment strategies for EIA aim to manage intraocular pressure fluctuations, preserve visual function, and improve the quality of life for affected individuals.
Topical medications, such as intraocular pressure-lowering eye drops, may be prescribed to control ocular hypertension and reduce the risk of glaucoma progression in patients with EIA. Regular monitoring of intraocular pressure is essential to adjust medication dosages and ensure optimal pressure control.
In cases where conservative measures are insufficient, surgical interventions like trabeculectomy or minimally invasive glaucoma surgery (MIGS) may be considered to enhance aqueous humor outflow and reduce intraocular pressure. These procedures can help prevent further optic nerve damage and preserve visual acuity in EIA patients at risk of glaucomatous complications.
Additionally, managing associated conditions such as cataracts or corneal endothelial cell loss is crucial in the overall care of individuals with EIA. Surgical techniques like cataract extraction with intraocular lens implantation or corneal endothelial cell transplantation may be implemented to address these comorbidities and improve visual outcomes.
Regular follow-up visits with an ophthalmologist are essential for monitoring disease progression, assessing treatment efficacy, and adjusting management strategies as needed. Patient education on the importance of medication adherence, lifestyle modifications, and ocular health maintenance plays a key role in the long-term management of Essential Iris Atrophy.
Complications Associated with EIA
Essential Iris Atrophy (EIA) is associated with various complications that can impact ocular health and visual function. One of the primary complications of EIA is the development of glaucoma due to intraocular pressure fluctuations resulting from structural changes in the iris.
Individuals with EIA are at an increased risk of developing cataracts, particularly following pseudophakia or prior cataract surgery. The presence of cataracts can further compromise vision and necessitate additional surgical interventions to restore visual acuity in affected patients.
Ocular hypertension is a common complication in EIA patients, requiring close monitoring and management to prevent optic nerve damage and vision loss. Corneal endothelial cell loss may also occur as a result of increased intraocular pressure, leading to corneal edema and potential visual disturbances.
Pigment dispersion syndrome and posterior polymorphous dystrophy are conditions often associated with EIA, further complicating the clinical course and increasing the complexity of disease management. These additional complications underscore the importance of comprehensive evaluation and targeted interventions to address the multifaceted nature of Essential Iris Atrophy.
Understanding the potential complications linked to EIA is essential for healthcare providers to implement proactive measures, optimize treatment outcomes, and mitigate the risk of long-term ocular sequelae. By addressing associated complications promptly and effectively, clinicians can help mitigate the impact of Essential Iris Atrophy on patients’ visual health and overall well-being.
Prognosis and Long-Term Outlook for EIA Patients
The prognosis for individuals with Essential Iris Atrophy (EIA) varies based on the severity of structural changes in the iris, associated complications, and response to treatment interventions. Long-term outlook for EIA patients is influenced by the management of intraocular pressure, glaucoma risk, and visual outcomes.
Early diagnosis and proactive management of EIA can positively impact the prognosis, helping to preserve visual function and prevent vision-threatening complications. Timely interventions to control intraocular pressure and address associated conditions like cataracts and corneal endothelial cell loss are crucial for optimizing long-term outcomes.
Regular monitoring of disease progression, visual acuity, and intraocular pressure is essential in assessing the efficacy of treatment modalities and adjusting management strategies as needed. Close collaboration between ophthalmologists, optometrists, and other healthcare providers is vital in ensuring comprehensive care and improving the long-term prognosis for EIA patients.
Despite the challenges posed by complications such as glaucoma and cataracts, advances in diagnostic technologies, surgical techniques, and pharmacological therapies offer promising prospects for enhancing the long-term outlook for individuals with Essential Iris Atrophy. Ongoing research efforts aimed at elucidating the underlying mechanisms of EIA and developing targeted treatments further contribute to improving the prognosis and quality of life for affected patients.
Empowering patients with education on disease management, lifestyle modifications, and regular ophthalmic follow-up can also play a significant role in promoting positive long-term outcomes and maintaining ocular health in individuals living with EIA.
Research and Advancements in EIA Treatment
Ongoing research efforts in the field of Essential Iris Atrophy (EIA) focus on elucidating the underlying pathophysiology of the condition, identifying novel treatment targets, and developing innovative therapeutic strategies to improve patient outcomes. Advances in diagnostic imaging modalities and genetic testing have enhanced our understanding of EIA’s etiology and progression.
Emerging pharmacological therapies aimed at modulating iris structure, controlling intraocular pressure, and managing associated complications show promise in the treatment of EIA. Targeted drug delivery systems, including sustained-release implants and topical formulations, offer new avenues for personalized treatment approaches and improved patient compliance.
Minimally invasive glaucoma surgeries (MIGS) and micro-invasive procedures represent significant advancements in the surgical management of EIA-related glaucoma. These techniques provide effective options for optimizing aqueous humor outflow and reducing intraocular pressure while minimizing surgical risks and enhancing postoperative recovery.
Research into regenerative medicine approaches, such as corneal endothelial cell transplantation and iris tissue engineering, holds potential for restoring vision and addressing corneal complications in EIA patients. These cutting-edge techniques offer innovative solutions for managing the sequelae of Essential Iris Atrophy and improving long-term visual outcomes.
Clinical trials investigating the safety and efficacy of novel therapies, including gene-based treatments and stem cell interventions, continue to expand the treatment landscape for EIA. Through collaborative research initiatives and multidisciplinary efforts, the development of targeted, personalized treatment regimens for individuals with Essential Iris Atrophy is advancing, paving the way for improved patient care and outcomes.
Conclusion
In conclusion, Essential Iris Atrophy (EIA) is a complex ocular disorder characterized by structural changes in the iris tissue that can lead to various clinical manifestations and complications. The etiology of EIA involves genetic predisposition and environmental factors, contributing to iris atrophy, pigment dispersion, and intraocular pressure dysregulation.
Diagnosis of EIA requires a comprehensive ophthalmic evaluation, including detailed imaging studies and intraocular pressure assessments. Management strategies for EIA focus on controlling intraocular pressure, addressing glaucoma risk, and managing associated conditions like cataracts and corneal endothelial cell loss.
Despite the challenges posed by EIA and its associated complications, advancements in research and treatment modalities offer hope for improved outcomes and enhanced quality of life for affected individuals. Research into regenerative medicine, pharmacological therapies, and surgical innovations continues to drive progress in the field of EIA management.
By increasing awareness, promoting early detection, and implementing personalized care plans, healthcare providers can make significant strides in optimizing the prognosis and long-term outlook for patients with Essential Iris Atrophy. Collaborative efforts across disciplines and ongoing research endeavors hold promise for advancing the understanding and treatment of this rare ocular condition.
Moving forward, continued dedication to research, clinical innovation, and patient-centered care is essential in improving outcomes and enhancing the overall well-being of individuals living with Essential Iris Atrophy. By staying at the forefront of advancements in EIA management, healthcare professionals can strive to provide comprehensive, effective, and compassionate care for those affected by this challenging condition.
