Disease Overview of Epidermolysis Bullosa, Junctional, with Pyloric Atrophy
Epidermolysis Bullosa, Junctional, with Pyloric Atrophy is a genetic disorder characterized by blistering of the skin and mucous membranes. This rare hereditary condition affects infants, causing difficulty in feeding due to pyloric atrophy, leading to malnutrition.
Understanding the impact of this disorder on digestion is crucial as it can result in scarring of the stomach. Early diagnosis is key for proper management. Learn more about the symptoms, diagnosis, treatment options, preventive measures, and support systems.
Understanding Epidermolysis Bullosa (EB)
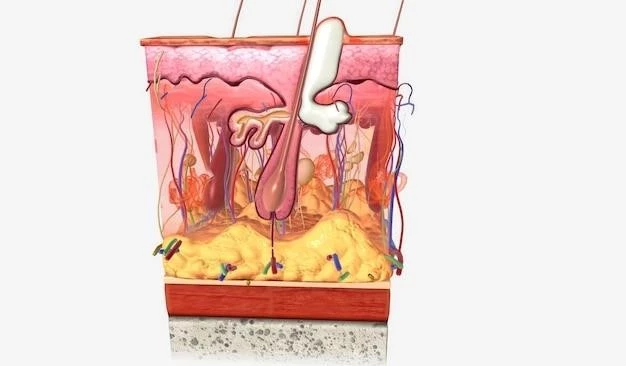
Epidermolysis Bullosa (EB) is a group of rare genetic disorders characterized by fragile skin that blisters and tears easily. In the case of Junctional EB with Pyloric Atrophy, this fragility extends to the mucous membranes, causing blistering in the body’s inner linings.
The primary cause of EB is mutations in certain genes responsible for the production of proteins that help anchor the skin layers together. Without these proteins, the skin is unable to withstand friction and other physical stresses, leading to the formation of blisters.
There are several subtypes of EB, with Junctional EB being one of the more severe forms. Adding pyloric atrophy to this condition further complicates the health of infants affected as it impacts their ability to feed properly.
Individuals with EB often experience blistering not only on the skin but also on internal organs, posing significant challenges to their health and quality of life. The constant formation of blisters can result in scarring, which may further impair skin integrity and function.
Living with EB requires careful management to prevent complications. Patients and caregivers must learn how to handle blistering episodes properly to minimize scarring and reduce the risk of infection.
Given the hereditary nature of EB, individuals with a family history of the disorder should seek genetic counseling to understand the risks and options for family planning. Early detection and awareness of symptoms are critical in providing timely interventions and support for those affected.
Overall, gaining a comprehensive understanding of Epidermolysis Bullosa is essential to promote effective management strategies, improve quality of life, and provide necessary care for individuals living with this challenging genetic disorder.
Symptoms of Junctional EB with Pyloric Atrophy
Junctional Epidermolysis Bullosa (EB) with Pyloric Atrophy presents a unique set of symptoms that affect both the skin and internal organs, particularly the stomach. Recognizing these symptoms is crucial for prompt diagnosis and appropriate management⁚
- Skin Blisters⁚ The hallmark symptom of EB is the formation of blisters on the skin in response to friction or trauma. These blisters are fragile and can lead to open sores if not properly cared for.
- Blisters on Mucous Membranes⁚ In Junctional EB, blistering can also occur on mucous membranes, such as the inside of the mouth, throat, and digestive tract, adding to the discomfort and risk of complications.
- Pyloric Atrophy⁚ Infants with this condition may exhibit difficulty feeding due to pyloric atrophy, a narrowing or blocking of the passage between the stomach and the small intestine. This can result in poor weight gain and malnutrition.
- Scarring⁚ Continuous blistering and healing cycles can lead to scarring of the skin and mucous membranes. This scarring may cause tightening and restriction of movement in affected areas.
- Infections⁚ Open blisters and skin erosions are vulnerable to infections. Keeping the skin clean and protected is essential to prevent secondary infections that can further compromise health.
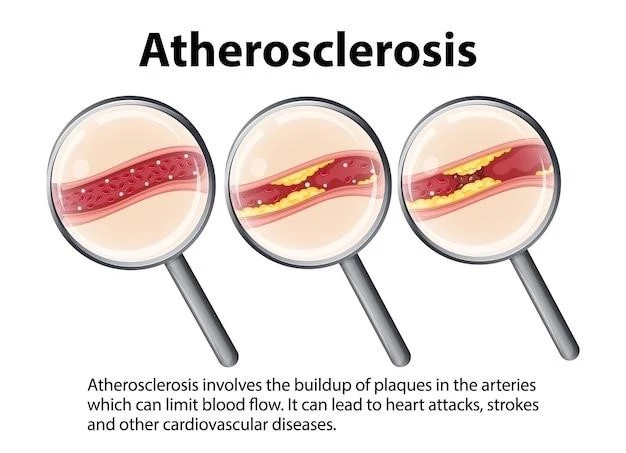
- Gastrointestinal Issues⁚ Pyloric atrophy can lead to digestive difficulties, including vomiting, bloating, and poor absorption of nutrients; These gastrointestinal issues can exacerbate malnutrition and growth delays in infants.
It is important to note that the severity of symptoms can vary depending on the subtype of EB and individual factors. Early recognition of these signs is crucial for initiating appropriate medical care, managing symptoms effectively, and improving the overall well-being of individuals living with Junctional EB with Pyloric Atrophy.
Diagnosis of Junctional EB with Pyloric Atrophy
Diagnosing Junctional Epidermolysis Bullosa (EB) with Pyloric Atrophy involves a comprehensive approach that considers the unique symptoms and challenges associated with this rare genetic disorder. Healthcare providers rely on various techniques and assessments to confirm the presence of the condition⁚
- Clinical Examination⁚ A thorough physical examination is conducted to assess the extent of blistering on the skin and mucous membranes, as well as any signs of scarring or skin fragility. The presence of pyloric atrophy may also be evaluated through physical exam findings related to feeding difficulties.
- Family History⁚ Since EB is a hereditary disorder, a detailed family history is essential in identifying patterns of inheritance and determining the likelihood of a genetic component in the individual’s condition.
- Genetic Testing⁚ Genetic tests, such as DNA sequencing, can help identify specific gene mutations associated with Junctional EB with Pyloric Atrophy. These tests can confirm the diagnosis and provide information about the subtype of EB present.
- Skin Biopsy⁚ In some cases, a skin biopsy may be performed to examine the skin under a microscope. This can reveal characteristic changes in the skin layers that are indicative of EB and help differentiate it from other skin conditions.
- Endoscopy⁚ To assess the extent of mucous membrane involvement and investigate pyloric atrophy, an endoscopy may be recommended. This procedure allows for visual examination of the digestive tract to identify any abnormalities.
- Nutritional Assessment⁚ Given the presence of pyloric atrophy and its impact on feeding and nutrition, healthcare providers may conduct nutritional assessments to evaluate the infant’s growth, weight gain, and overall nutritional status.
Early and accurate diagnosis of Junctional EB with Pyloric Atrophy is crucial for creating a tailored treatment plan and implementing appropriate interventions to address the complex symptoms associated with this condition. Individuals suspected of having EB should seek evaluation and guidance from healthcare professionals experienced in managing genetic skin disorders.
Impact on Infants and Children
Epidermolysis Bullosa (EB) Junctional with Pyloric Atrophy can have a profound impact on the lives of infants and children affected by this complex genetic disorder. Understanding the challenges and implications for their well-being is vital for providing optimal care and support⁚
- Feeding Difficulties⁚ Pyloric atrophy in Junctional EB can lead to significant feeding difficulties in infants, causing malnutrition, poor weight gain, and growth delays. This poses a direct threat to their health and development.
- Physical Discomfort⁚ Constant blistering and skin fragility result in physical discomfort for children with EB. The pain and itching associated with blisters can impact their quality of life and daily activities.
- Scarring and Mobility Limitations⁚ The scarring that follows recurrent blistering episodes can lead to skin tightening and mobility limitations. This can affect movement, range of motion, and overall independence in children.
- Social and Emotional Well-being⁚ Children with EB may experience social challenges due to their visible symptoms, such as blisters and scarring. The emotional toll of living with a chronic condition can also impact their self-esteem and mental health.
- Medical Interventions⁚ Managing EB often involves frequent medical interventions, such as wound care, bandaging, and medications. These treatments can be time-consuming and may cause additional stress for both children and their caregivers.
- Educational Considerations⁚ Children with EB may require special accommodations at school to address their unique needs, including skin protection measures, modified physical activities, and support for any educational challenges arising from their condition.
It is essential for healthcare providers, families, and educators to work collaboratively to address the multifaceted impact of Junctional EB with Pyloric Atrophy on infants and children. By implementing a holistic care approach that considers physical, emotional, and social aspects, it is possible to enhance the quality of life and well-being of young individuals navigating the complexities of this challenging genetic disorder.
Treatment Options for Junctional EB with Pyloric Atrophy
Managing Junctional Epidermolysis Bullosa (EB) with Pyloric Atrophy requires a multidisciplinary approach to address the diverse symptoms and complications associated with this complex genetic disorder. Treatment options aim to alleviate symptoms, promote skin healing, and support overall well-being⁚
- Wound Care⁚ Proper wound care is critical for individuals with EB to prevent infection and promote healing. Gentle cleansing, application of dressings, and protective bandages help manage blisters and minimize the risk of complications.
- Pain Management⁚ Pain associated with blistering and skin fragility can be significant. Healthcare providers may recommend pain management strategies, such as topical or oral medications, to improve comfort and quality of life.
- Nutritional Support⁚ Infants with Junctional EB and pyloric atrophy may require nutritional interventions to address feeding difficulties and ensure adequate calorie intake. Working with a dietitian can help tailor a nutritional plan to support growth and development.
- Skin Protection⁚ Protective measures, such as using special clothing, avoiding friction-inducing activities, and keeping the skin moisturized, can help reduce the risk of blistering and skin damage. Sun protection is also essential to prevent sunburn and further skin trauma.
- Surgical Interventions⁚ In some cases, surgical procedures may be necessary to address complications of EB, such as severe scarring, contractures, or gastrointestinal issues. These interventions aim to improve functionality and quality of life for individuals with the condition.
- Genetic Counseling⁚ Genetic counseling is valuable for families affected by EB to understand the genetic implications of the disorder, explore family planning options, and receive emotional support. It empowers individuals to make informed decisions about their health and future.
It is essential for healthcare professionals to tailor treatment plans to the specific needs of each individual with Junctional EB with Pyloric Atrophy. By combining medical interventions, supportive care, and lifestyle modifications, it is possible to enhance quality of life, manage symptoms effectively, and promote holistic well-being for those living with this challenging genetic disorder.
Preventive Measures and Care
Preventive measures and diligent care play a vital role in managing Junctional Epidermolysis Bullosa (EB) with Pyloric Atrophy, helping to minimize complications, reduce discomfort, and improve overall quality of life for individuals affected by this intricate genetic disorder; Consider the following preventive measures and care strategies⁚
- Skin Protection⁚ Implementing skin protection strategies is crucial to prevent blistering and skin damage. Use soft clothing, avoid rough fabrics, and apply gentle skincare products to maintain skin integrity.
- Wound Management⁚ Prompt and proper wound management is essential to reduce the risk of infection and promote healing. Cleanse wounds carefully, apply appropriate dressings, and seek medical attention for severe blisters.
- Pain Relief⁚ Addressing pain associated with blistering and skin fragility is paramount. Consult healthcare providers for pain management options, which may include topical treatments or pain medications prescribed as needed.
- Hydration and Nutrition⁚ Ensure adequate hydration and proper nutrition to support skin health and overall well-being. Stay well-hydrated, consume a balanced diet rich in essential nutrients, and consider nutritional supplements if necessary.
- Regular Medical Follow-ups⁚ Schedule regular check-ups with healthcare providers experienced in managing EB to monitor skin condition, address any emerging issues, and adjust treatment plans as needed.
- Psycho-Social Support⁚ Seek psycho-social support to address emotional challenges and mental well-being associated with living with a chronic condition. Engage in support groups, counseling, and other resources to enhance coping strategies.
- Sun Protection⁚ Protect the skin from sun exposure by using sunscreen with a high SPF, wearing protective clothing, and seeking shade during peak sun hours. Sun protection helps prevent sunburn and minimize skin damage.
- Educational Awareness⁚ Educate family members, caregivers, teachers, and peers about EB to promote understanding and create a supportive environment for individuals affected by the disorder.
By incorporating preventive measures and attentive care practices into daily routines, individuals living with Junctional EB with Pyloric Atrophy can navigate the challenges of the condition more effectively, reduce the frequency of complications, and uphold skin health and overall well-being for a better quality of life.
Support Systems for Families
Families impacted by Junctional Epidermolysis Bullosa (EB) with Pyloric Atrophy often face unique challenges that necessitate comprehensive support systems to navigate the complexities of managing this genetic disorder. Building a strong network of support is crucial for both practical assistance and emotional well-being⁚
- Medical Guidance⁚ Seek guidance from healthcare professionals specializing in EB to receive expert medical advice, treatment options, and ongoing support tailored to the specific needs of the individual with Junctional EB and pyloric atrophy.
- Genetic Counseling⁚ Engage in genetic counseling to understand the hereditary nature of EB, explore family planning options, and address any concerns related to the risk of passing on the genetic mutation to future generations.
- Support Groups⁚ Join EB support groups and communities to connect with other families facing similar challenges. These groups offer a platform for sharing experiences, exchanging information, and receiving emotional support from individuals who understand the journey.
- Psychological Support⁚ Access mental health resources, such as counseling or therapy, to address the emotional impact of living with a chronic condition. Mental health professionals can provide coping strategies and support families in managing stress and anxiety.
- Educational Advocacy⁚ Advocate for educational accommodations and support for children with EB in academic settings. Work closely with school administrators and teachers to ensure the child’s educational needs are met while accommodating any physical limitations or health considerations.
- Respite Care⁚ Explore respite care options to provide temporary relief for caregivers and family members. Respite care services offer much-needed breaks for caregivers, allowing them to recharge and prioritize self-care.
- Financial Assistance⁚ Investigate financial assistance programs, grants, and resources available to families managing EB. Financial support can help offset the costs associated with medical treatments, specialized care, and other related expenses.
- Care Coordination⁚ Foster open communication and coordination among healthcare providers, therapists, and caregivers involved in the care of the individual with EB. Collaborative care ensures continuity of treatment and holistic support for the entire family unit.
By leveraging the various support systems available, families can navigate the complexities of managing Junctional EB with Pyloric Atrophy more effectively, enhance their resilience in facing challenges, and cultivate a supportive environment conducive to the well-being of both the affected individual and the entire family unit.