Understanding Delayed Sleep Phase Syndrome
Sleep disorder characterized by a delay in the typical sleep-wake schedule, impacting circadian rhythm. Melatonin regulation affected, leading to insomnia. Diagnosis involves assessing sleep patterns. Treatment includes Chronotherapy, Bright Light Therapy, and maintaining good sleep hygiene. Impacts adolescents’ sleep quality. Genetics play a role in its development.
I. Introduction to Delayed Sleep Phase Syndrome
Delayed Sleep Phase Syndrome (DSPD) is a sleep disorder that affects the timing of sleep. Individuals with DSPD often have difficulty falling asleep at conventional times and struggle to wake up in the morning, leading to sleep deprivation. This condition is characterized by a delay in the circadian rhythm, the body’s internal clock that regulates the sleep-wake cycle.
People with DSPD may find it challenging to adhere to a regular schedule due to their delayed sleep pattern, impacting daily functioning and overall well-being. This syndrome can disrupt daily activities, work performance, and social interactions.
Understanding DSPD is crucial as it can significantly impact an individual’s quality of life. By exploring the causes, symptoms, and treatment options for DSPD, individuals can learn how to manage their condition effectively and improve their sleep hygiene. Addressing DSPD early can lead to better sleep habits and overall health.
II. Understanding Circadian Rhythm and Melatonin
Circadian rhythm refers to the natural internal process that regulates the sleep-wake cycle in humans. This biological clock follows a roughly 24-hour cycle, influencing various physiological functions like hormone release, body temperature, and alertness levels. Disruption to the circadian rhythm can lead to sleep disturbances, including Delayed Sleep Phase Syndrome (DSPD).
Melatonin, known as the ″sleep hormone,″ is a key player in regulating the circadian rhythm. It is produced by the pineal gland in response to darkness, signaling the body that it’s time to sleep. Individuals with DSPD often have abnormal melatonin secretion patterns, leading to difficulties falling asleep at conventional bedtime hours.
Understanding the intricate relationship between the circadian rhythm and melatonin production is essential in comprehending the underlying mechanisms of DSPD. By exploring how these biological processes interact and influence sleep patterns, researchers and healthcare providers can develop effective treatment strategies to help individuals with DSPD manage their condition and improve their sleep quality.
III. Symptoms and Diagnosis of DSPD
The hallmark symptom of Delayed Sleep Phase Syndrome (DSPD) is the inability to fall asleep at a conventional bedtime. Individuals with DSPD often experience a delay in their sleep onset, resulting in staying awake until late hours of the night. As a result, they may struggle to wake up in the morning, leading to excessive daytime sleepiness.
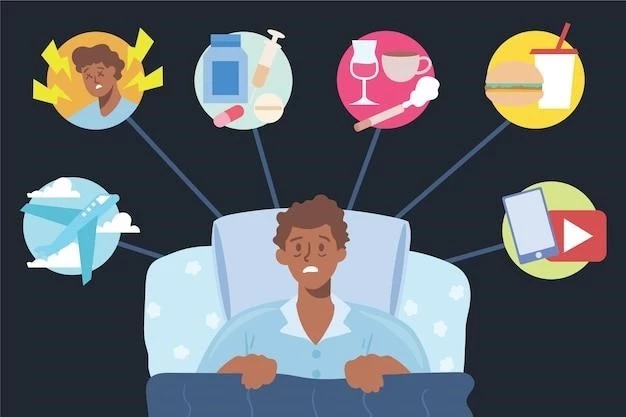
Other common symptoms of DSPD include irritability, poor concentration, and mood disturbances due to the disrupted sleep-wake cycle; These symptoms can significantly impact an individual’s daily life, work performance, and overall well-being.
Diagnosing DSPD involves assessing an individual’s sleep patterns over an extended period, typically through sleep logs and actigraphy monitoring. Healthcare providers may also conduct a clinical interview to evaluate the severity and impact of symptoms on the individual’s life. Differentiating DSPD from other sleep disorders is crucial for developing a tailored treatment plan that addresses the specific needs of the individual.
IV. Differentiating DSPD from Other Sleep Disorders
It is crucial to differentiate Delayed Sleep Phase Syndrome (DSPD) from other sleep disorders to ensure accurate diagnosis and appropriate treatment; While DSPD is characterized by a delayed sleep-wake schedule and a shift in the circadian rhythm, other sleep disorders present with distinct symptoms and underlying causes.
One common disorder to differentiate from DSPD is insomnia, which involves difficulty falling asleep or staying asleep, leading to sleep deprivation and daytime impairment. In contrast, individuals with DSPD often have a delayed sleep onset but may experience a full night of sleep once they fall asleep.
Another condition to consider is Non-24-Hour Sleep-Wake Disorder, a circadian rhythm disorder where an individual’s sleep-wake pattern shifts later each day, causing difficulty maintaining a steady sleep schedule. Unlike DSPD, Non-24-Hour Sleep-Wake Disorder follows a free-running rhythm without external time cues.
By understanding the unique features of DSPD compared to other sleep disorders, healthcare providers can make an accurate diagnosis and implement tailored treatment strategies that address the specific challenges faced by individuals with delayed sleep phase syndrome.
V. Treatment Options for DSPD
Treatment for Delayed Sleep Phase Syndrome (DSPD) aims to align the individual’s sleep-wake schedule with their desired lifestyle while improving overall sleep quality. One common approach is Chronotherapy, which involves gradually adjusting bedtime and wake time until the desired schedule is achieved.
Bright Light Therapy is another effective treatment for DSPD, where exposure to bright light in the morning helps shift the circadian rhythm earlier, promoting earlier bedtime and wake-up times. This therapy helps synchronize the internal body clock with external light-dark cycles.
Improving sleep hygiene is essential in managing DSPD. Practicing good sleep habits, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing the sleep environment, can enhance sleep quality and promote better rest.
In some cases, medications like melatonin supplements may be prescribed to help regulate the sleep-wake cycle and improve sleep onset in individuals with DSPD. However, medication should be used under the guidance of a healthcare provider to ensure safety and efficacy.
By combining behavioral interventions, light therapy, and proper sleep hygiene practices, individuals with Delayed Sleep Phase Syndrome can effectively manage their condition and enjoy better sleep patterns, leading to improved overall well-being and quality of life.
VI. Importance of Sleep Hygiene in Managing DSPD
Sleep hygiene plays a vital role in managing Delayed Sleep Phase Syndrome (DSPD) by promoting healthy sleep habits and optimizing the sleep environment. Establishing a consistent sleep schedule is crucial for individuals with DSPD to regulate their sleep-wake cycle and improve the quality of their rest.
Creating a relaxing bedtime routine can help signal the body that it is time to wind down and prepare for sleep. This may include activities such as reading a book, practicing relaxation techniques, or taking a warm bath before bedtime.
Avoiding stimulants like caffeine, nicotine, and electronic devices close to bedtime can help reduce sleep disturbances and improve sleep onset in individuals with DSPD. Creating a sleep-conducive environment, which is cool, dark, and quiet, can enhance the quality and duration of sleep.
Engaging in regular physical activity during the day can promote restful sleep at night by reducing stress and anxiety levels. However, vigorous exercise should be avoided close to bedtime as it may stimulate the body and interfere with the ability to fall asleep.
By prioritizing good sleep hygiene practices, individuals with Delayed Sleep Phase Syndrome can create a supportive sleep routine that aligns with their circadian rhythm, leading to improved sleep quality and overall well-being. Consistency and commitment to healthy sleep habits are essential in managing DSPD and promoting better restorative sleep.
VII. Chronotherapy and Its Efficacy in Treating DSPD
Chronotherapy is a behavioral intervention commonly used to treat Delayed Sleep Phase Syndrome (DSPD) by gradually adjusting the individual’s sleep schedule to align with their desired bedtime and wake-up times. This therapy aims to shift the circadian rhythm to a more conventional time frame, improving sleep quality and daytime alertness.
Chronotherapy typically involves delaying the bedtime by a few hours each night until reaching the desired sleep schedule. This gradual adjustment allows the body’s internal clock to adapt to the new sleep-wake cycle, making it easier for individuals with DSPD to fall asleep and wake up at the desired times.
Research has shown that Chronotherapy can be effective in resetting the circadian rhythm in individuals with DSPD, leading to improvements in sleep onset, sleep duration, and overall sleep quality. By gradually shifting the bedtime and wake-up times, individuals can experience better alignment between their internal body clock and external light-dark cycles.
While Chronotherapy can be an effective treatment for DSPD, it is essential for individuals to maintain consistency and dedication throughout the adjustment period. Working closely with healthcare providers or sleep specialists can help monitor progress and optimize the timing of sleep schedule changes to achieve optimal results;
Overall, Chronotherapy offers a non-invasive and practical approach to managing Delayed Sleep Phase Syndrome, helping individuals establish a more regular sleep pattern that supports their daily activities and promotes better overall well-being.
VIII. Bright Light Therapy for DSPD
Bright Light Therapy is a non-pharmacological treatment method used to manage Delayed Sleep Phase Syndrome (DSPD) by exposing individuals to bright light, typically in the morning. This therapy aims to reset the circadian rhythm and improve sleep patterns by synchronizing the body’s internal clock with external light cues.
Individuals with DSPD often have a delayed sleep-wake cycle due to a shift in their circadian rhythm. Bright Light Therapy helps correct this delay by providing exposure to intense light, mimicking natural sunlight, which signals the body to reset its internal clock earlier, promoting an earlier bedtime and wake-up time.
Research has shown that regular exposure to bright light therapy can be effective in advancing the circadian phase, improving sleep onset latency, and reducing daytime sleepiness in individuals with DSPD. The therapy’s success relies on the consistency of light exposure and adherence to a structured schedule.
Bright Light Therapy is a safe and well-tolerated intervention for DSPD, offering a natural approach to regulating the sleep-wake cycle without the need for medications. Healthcare providers may recommend specific light intensities and durations based on individual needs and response to treatment to optimize its efficacy.
By incorporating Bright Light Therapy into a comprehensive treatment plan for DSPD, individuals can benefit from improved sleep quality, reduced daytime impairments, and better alignment with their desired sleep schedule, ultimately enhancing their overall quality of life.
IX. Impact of Shift Work on DSPD
Shift work can exacerbate the symptoms of Delayed Sleep Phase Syndrome (DSPD) due to the irregular and often rotating work schedules that disrupt the body’s natural circadian rhythm. Individuals who work night shifts or irregular hours may experience difficulty falling asleep at conventional times and struggle to maintain a consistent sleep routine.
The mismatch between work schedules and the body’s internal clock can lead to chronic sleep deprivation, increased daytime sleepiness, and poor cognitive performance in individuals with DSPD. Shift workers with DSPD may find it challenging to adjust to their work demands while managing their delayed sleep-wake cycle.
Research has shown that shift work can impact the overall health and well-being of individuals with DSPD, increasing the risk of developing other health conditions such as cardiovascular issues, metabolic disorders, and mental health problems. The disruption of the circadian rhythm caused by shift work can have long-term implications on both physical and mental health.
Managing the impact of shift work on DSPD requires implementing strategies to promote healthy sleep habits and optimize the sleep environment. Creating a consistent bedtime routine, prioritizing restful sleep, and incorporating relaxation techniques can help mitigate the negative effects of shift work on individuals with DSPD.
By recognizing the challenges posed by shift work on individuals with Delayed Sleep Phase Syndrome and implementing tailored interventions to support their sleep health, employers and healthcare providers can help mitigate the impact of irregular work schedules and promote better overall well-being for individuals with DSPD.
X. DSPD in Adolescents
Delayed Sleep Phase Syndrome (DSPD) commonly affects adolescents, manifesting as a delay in the sleep-wake cycle that is out of sync with typical societal schedules. Adolescents with DSPD often struggle to fall asleep at conventional bedtime hours, leading to insufficient sleep duration and daytime sleepiness.
The natural shift in circadian rhythm during adolescence can exacerbate the symptoms of DSPD, making it challenging for teenagers to adhere to early school start times and maintain a consistent sleep schedule. This can impact academic performance, mood regulation, and overall quality of life for adolescents with DSPD.
Addressing DSPD in adolescents requires a multi-faceted approach that considers the unique developmental factors and lifestyle demands of this population. Interventions such as adjusting school start times, promoting healthy sleep hygiene practices, and incorporating behavioral therapies can help adolescents with DSPD manage their condition effectively.
Educating parents, teachers, and healthcare providers about the challenges faced by adolescents with Delayed Sleep Phase Syndrome is essential in creating supportive environments that prioritize sleep health. By raising awareness and implementing tailored strategies, the impact of DSPD on adolescents can be minimized, allowing them to thrive academically and socially.
Supporting adolescents with DSPD in establishing healthy sleep habits and embracing their unique sleep patterns can empower them to navigate the challenges of their condition and achieve optimal sleep quality, contributing to their overall well-being and success during this critical stage of development.
XI. Genetics and DSPD
Genetics play a significant role in the development of Delayed Sleep Phase Syndrome (DSPD), highlighting the hereditary component of this circadian rhythm disorder. Research indicates that individuals with a family history of DSPD are more likely to experience disruptions in their sleep-wake cycle due to genetic influences.
Specific genetic variations have been linked to the regulation of the circadian rhythm and the production of melatonin, both of which are crucial factors in the onset and manifestation of DSPD. Variants in clock genes and melatonin receptors can impact an individual’s susceptibility to developing delayed sleep phase syndrome.
The presence of genetic predispositions does not guarantee the development of DSPD, as environmental factors and lifestyle choices also contribute to the expression of this sleep disorder. However, understanding the genetic underpinnings of DSPD can provide valuable insights into the biological mechanisms that influence the circadian system and sleep patterns.
Genetic testing and research studies focusing on the genetic basis of DSPD continue to enhance our understanding of how genes interact with environmental factors to shape an individual’s sleep-wake cycle. By unraveling the genetic complexity of DSPD, researchers aim to develop personalized treatment approaches that target specific genetic markers associated with this circadian disorder.
Ultimately, exploring the intricate relationship between genetics and Delayed Sleep Phase Syndrome offers promising avenues for future research and personalized medicine initiatives aimed at tailoring interventions to individuals based on their genetic profiles, advancing the management and treatment of DSPD for improved outcomes.
XII. Conclusion⁚ Managing DSPD for Better Quality of Life
Delayed Sleep Phase Syndrome (DSPD) can significantly impact an individual’s daily functioning, productivity, and overall well-being by disrupting the natural sleep-wake cycle. However, with the right interventions and strategies, managing DSPD is possible, leading to improved sleep quality and a better quality of life.
Effective treatment options such as Chronotherapy and Bright Light Therapy can help individuals with DSPD align their sleep schedule with their desired lifestyle, promoting healthier sleep patterns and increased daytime alertness. By incorporating these therapies into a comprehensive treatment plan, individuals can establish a more stable sleep routine and enhance their overall sleep quality.
Furthermore, the importance of practicing good sleep hygiene cannot be overstated in managing DSPD. Creating a consistent bedtime routine, optimizing the sleep environment, and avoiding stimulants close to bedtime can significantly improve sleep onset and maintenance for individuals with delayed sleep phase syndrome.
Addressing the impact of shift work, particularly in adolescents, and recognizing the role of genetics in the development of DSPD are essential steps in providing tailored care and support for individuals affected by this circadian disorder. By raising awareness, educating stakeholders, and implementing personalized treatment approaches, the management of DSPD can be optimized for better outcomes and an enhanced quality of life.
Overall, by prioritizing sleep health, implementing evidence-based interventions, and fostering a supportive environment, individuals with Delayed Sleep Phase Syndrome can effectively manage their condition and experience improved sleep patterns, leading to better overall health and well-being.
