Understanding Progressive Familial Intrahepatic Cholestasis (PFIC)
Understanding the causes of Progressive Familial Intrahepatic Cholestasis is crucial for effective management.
Causes of Progressive Familial Intrahepatic Cholestasis
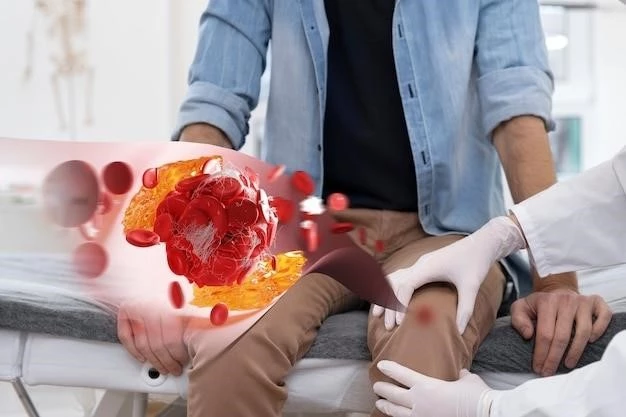
PFIC can be caused by genetic mutations affecting bile formation and flow, leading to liver damage. Specific genes like ABCB11 or ATP8B1 are often involved. In some cases, the condition may result from abnormal bile salt metabolism or transport issues.
Symptoms and Diagnosis of Cholestasis
Recognizing symptoms and conducting proper diagnosis are essential for managing cholestasis effectively.
Symptoms of Cholestasis in Children
Children with cholestasis may experience jaundice, itching, pale stool, dark urine, and abdominal pain. Other signs include poor growth, easy bruising, and vitamin deficiencies. Timely recognition of these symptoms is crucial for early intervention and management.
Diagnosis of Intrahepatic Cholestasis
Diagnosis of intrahepatic cholestasis involves physical exams, blood tests for liver function, imaging scans, and sometimes liver biopsy. Genetic testing may help in specific cases like PFIC. Early and accurate diagnosis is key for initiating appropriate treatment strategies to manage the condition effectively.

Treatment and Management of Cholestasis
Effective treatment and management strategies are crucial in handling cholestasis and improving patient outcomes;
Treatment Options for Progressive Familial Intrahepatic Cholestasis
Treatment for PFIC may involve medications to improve bile flow, nutritional support, surgery like liver transplant in severe cases, and ongoing monitoring. Specialized care and a multidisciplinary approach are essential for managing PFIC effectively and improving quality of life for patients.
Management of Cholestasis During Pregnancy
Managing cholestasis during pregnancy involves close monitoring of liver function, fetal well-being, and potential complications. Treatment may include medication to reduce bile acids, monitoring of blood levels, and timely delivery to minimize risks to both mother and baby. Collaborative care between obstetricians and hepatologists is crucial for ensuring optimal outcomes.
Research and Complications
Staying informed about research advancements and possible complications is vital for managing cholestasis effectively.
Research Updates on Progressive Familial Intrahepatic Cholestasis
Ongoing research on PFIC focuses on identifying new treatment options, understanding genetic factors, and improving diagnostic methods. Studies aim to enhance patient care, outcomes, and quality of life for individuals with this rare liver disorder.
Complications of Cholestasis in Infants
Cholestasis in infants can lead to malabsorption of nutrients, poor growth, vitamin deficiencies, and in severe cases, liver damage. Prompt diagnosis and appropriate management are crucial in preventing long-term complications and ensuring the well-being of the infant.
Dietary Recommendations for Cholestasis Patients
Cholestasis patients should follow a diet low in fat, adequate in protein, and rich in vitamins and minerals. They may benefit from small, frequent meals and avoiding certain foods like fried or processed items. Dietary modifications play a key role in managing symptoms and supporting liver function in individuals with cholestasis.