Introduction
Candida (Torulopsis) glabrata is a fungus with a diversity of habitats and an enlarging clinical spectrum that is now recognized as a cause of disease in both normal and compromised hosts. Initially considered nonpathogenic‚ this fungus has become increasingly associated with various clinical manifestations.
Overview of Torulopsis Disease
Candida (Torulopsis) glabrata‚ initially considered nonpathogenic‚ has evolved to cause various clinical manifestations in both normal and compromised hosts. As a fungus with a diverse habitat and clinical spectrum‚ it is increasingly recognized as a significant contributor to disease in individuals. Found as human flora in various body sites‚ it has transitioned from its saprophytic nature to becoming locally invasive and disseminating‚ especially in immunocompromised individuals.
Candida Glabrata⁚ The Fungus Behind Torulopsis
Candida (Torulopsis) glabrata‚ previously known as Torulopsis glabrata‚ is a fungus belonging to the Fungi Imperfecti class‚ with a unique nondimorphic blastoconidial morphology and a haploid genome. It has evolved into an opportunistic pathogen causing superficial mucosal and life-threatening bloodstream infections‚ primarily affecting immunocompromised individuals.
Characteristics of Candida Glabrata
Candida (Torulopsis) glabrata‚ previously known as Torulopsis glabrata‚ is a fungus belonging to the Fungi Imperfecti class. It exhibits a unique nondimorphic blastoconidial morphology and possesses a haploid genome‚ distinguishing it from other Candida species. Despite being frequently found as part of the human microflora‚ C. glabrata can cause disease in immunocompromised individuals. Its opportunistic nature enables it to transition from commensalism to pathogenicity‚ leading to various clinical manifestations.
Candida Glabrata as an Opportunistic Pathogen
Candida (Torulopsis) glabrata‚ despite its initial nonpathogenic nature‚ has emerged as an opportunistic pathogen capable of causing superficial mucosal to life-threatening bloodstream infections‚ particularly in individuals with compromised immune systems. Its evolution has led to a shift in its clinical significance‚ transitioning from a harmless commensal to a significant threat to vulnerable populations‚ necessitating careful management and treatment strategies.
Clinical Manifestations of Torulopsis Infection
Candida (Torulopsis) glabrata‚ previously considered nonpathogenic‚ now causes various clinical manifestations ranging from superficial mucosal to life-threatening bloodstream infections. It exhibits an opportunistic nature‚ especially affecting immunocompromised individuals‚ highlighting the evolving significance of this fungus in clinical settings.
Normal Flora and Pathogenicity
Candida (Torulopsis) glabrata is initially considered nonpathogenic and forms part of the human flora in various body sites. However‚ in certain circumstances‚ the organism can turn pathogenic‚ showcasing an ability to become locally invasive and potentially disseminate‚ especially posing threats to immunocompromised individuals.
Torulopsis Infections in Immunocompromised Individuals
Immunocompromised individuals are particularly vulnerable to Torulopsis infections caused by Candida (Torulopsis) glabrata. This opportunistic pathogen can lead to various clinical manifestations‚ including superficial mucosal and life-threatening bloodstream infections. As the normal flora can turn pathogenic‚ special attention is required to manage these infections effectively‚ especially in individuals with compromised immune systems.
Epidemiology and Pathogenesis
Candida (Torulopsis) glabrata‚ initially considered nonpathogenic‚ has evolved into an opportunistic pathogen causing a range of infections. Its prevalence and pathogenicity have expanded‚ especially in immunocompromised individuals‚ distinguishing it as a significant clinical concern.
Comparison with Other Candida Species
When compared to other Candida species‚ Candida (Torulopsis) glabrata stands out with its nondimorphic blastoconidial morphology and haploid genome. It ranks as a significant causative agent of various candidal infections‚ both superficial and systemic‚ with a notable impact on clinical outcomes‚ especially in healthcare settings.
Nosocomial Infections by Candida Glabrata
The prevalence of nosocomial infections caused by Candida (Torulopsis) glabrata has been increasing‚ posing a significant challenge in healthcare settings. This opportunistic pathogen is known to cause a variety of infections‚ including bloodstream infections‚ particularly affecting immunocompromised patients. Understanding the epidemiology and pathogenesis of these infections is crucial for effective management and prevention strategies in healthcare facilities.

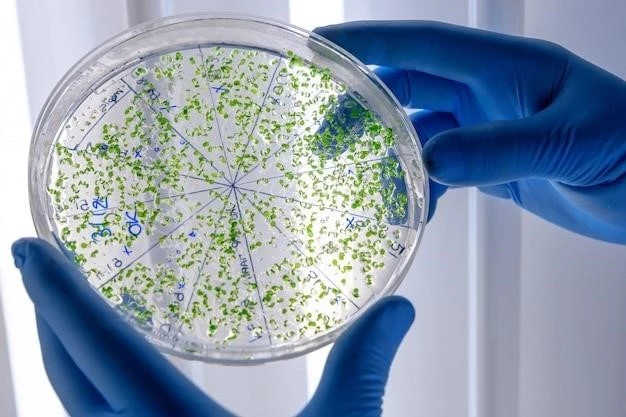
Diagnosis and Screening Methods
Candida (Torulopsis) glabrata‚ with its expanding clinical spectrum‚ presents challenges in diagnosis. Screening methods‚ such as the trehalose screening test‚ play a crucial role in detecting T. glabrata infections with high sensitivity and specificity. Understanding the intricacies of diagnosis is essential for timely and accurate identification of this opportunistic pathogen.
Trehalose Screening Test for T. Glabrata
The trehalose screening test plays a significant role in diagnosing T. Glabrata infections with high accuracy. This screening method demonstrates exceptional sensitivity and specificity‚ providing clinicians with a valuable tool for the efficient detection of T. Glabrata‚ contributing to timely and appropriate management of infections.
Sensitivity and Specificity of Screening Methods
Screening methods for Candida (Torulopsis) glabrata infections exhibit high sensitivity (97.8%) and specificity (95.8%)‚ demonstrating reliable accuracy in identifying the pathogen. With a positive predictive value of 97.4% and a negative predictive value of 96.5%‚ these screening tests offer clinicians effective tools for the detection of T. glabrata‚ aiding in prompt and precise diagnosis.
Treatment and Management
Effective management of Candida (Torulopsis) glabrata infections often involves antifungal therapies targeting the unique characteristics of this fungus. Alongside antifungal treatments‚ clinical management practices focus on tailored approaches to address the challenges posed by this opportunistic pathogen‚ especially in immunocompromised individuals.
Antifungal Therapies for Torulopsis Infections
Antifungal therapies play a critical role in the treatment of Candida (Torulopsis) glabrata infections. Tailored antifungal treatments are essential to combat the unique characteristics of this fungus effectively. Combined with appropriate clinical management strategies‚ antifungal therapies contribute significantly to the successful management of Torulopsis infections‚ particularly in immunocompromised individuals.
Clinical Management of Torulopsis Disease
The clinical management of Torulopsis disease involves a multifaceted approach aimed at addressing the complex nature of Candida (Torulopsis) glabrata infections. Tailored clinical strategies and treatment regimens are crucial in effectively managing the diverse clinical manifestations of this opportunistic pathogen‚ especially in immunocompromised individuals.

Case Studies and Outcomes
Successful treatment of Torulopsis Glabrata fungemia showcases the importance of tailored therapies. Impact of comorbidities on disease progression requires a comprehensive approach for optimal outcomes.
Successful Treatment of Torulopsis Glabrata Fungemia
Successful treatment of Torulopsis Glabrata fungemia exemplifies tailored therapy in clinical practice. Effective management contributes to positive outcomes in patients battling this opportunistic fungal infection.
Impact of Various Comorbidities on Disease Progression
The progression of Torulopsis disease can be influenced by various comorbidities in affected individuals. Understanding the impact of these underlying conditions on disease severity and outcomes is crucial for tailoring effective treatment strategies and improving patient prognosis.