Article Plan⁚ Disease ⸺ Spastic Paraplegia Familial Autosomal Recessive Form
Today is 03/25/2024 19⁚32⁚51
Introduction to Hereditary Spastic Paraplegia (HSP)
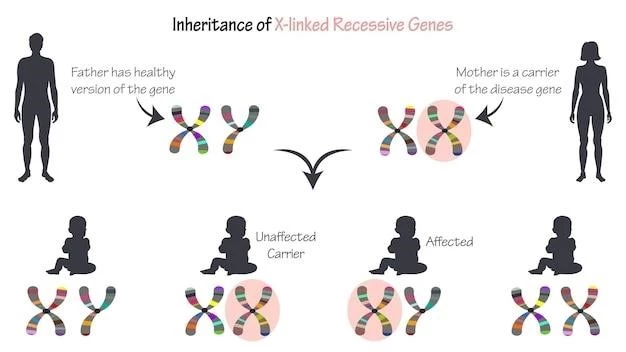
Hereditary Spastic Paraplegia (HSP) encompasses a group of neurodegenerative disorders characterized by progressive stiffness and weakness in the lower extremities. It involves the corticospinal tracts and typically presents with spastic gait. HSP can be inherited in various ways‚ including autosomal dominant‚ autosomal recessive‚ and X-linked patterns.
Various genetic loci‚ denoted as SPG followed by a number‚ have been identified to be associated with different forms of HSP. The prevalence of HSP‚ both autosomal dominant and autosomal recessive types combined‚ is estimated to be around 1.8 per 100‚000 cases. Diagnosis is crucial and is based on inheritance pattern‚ clinical phenotype‚ and molecular pathophysiology.
Individuals with HSP can experience a range of symptoms‚ including muscle stiffness‚ lower limb weakness‚ spasticity‚ bladder dysfunction‚ and in some cases‚ additional neurological manifestations. Understanding the genetic basis of HSP is advancing rapidly‚ leading to improved diagnostic accuracy and potentially targeted treatment approaches.
Autosomal Recessive Forms of HSP
Autosomal Recessive Spastic Paraplegia is a subset of Hereditary Spastic Paraplegia that follows an autosomal recessive inheritance pattern. Various forms of autosomal recessive HSP have been identified‚ such as SPG11‚ SPG30‚ SPG5A‚ and SPG46‚ each presenting with distinct clinical features.
For instance‚ SPG11 is one of the most common causes of autosomal recessive HSP‚ leading to muscle stiffness progressing to lower limb paralysis and other neurological symptoms. Understanding these distinct forms is crucial for accurate diagnosis and appropriate management strategies tailored to each individual’s needs.
Being informed about the genetic basis and inheritance patterns of autosomal recessive HSP can help individuals and families better navigate the complexities of this condition. It is essential to consult healthcare professionals for genetic counseling‚ accurate diagnosis‚ and to explore available support resources for optimal management and care.
Genetic Loci and Inheritance Patterns
Hereditary Spastic Paraplegia (HSP) comprises a diverse group of disorders with multiple inheritance patterns‚ including autosomal dominant‚ autosomal recessive‚ X-linked‚ and mitochondrial modes. Genetic loci associated with different forms of HSP are denoted as SPG followed by a sequential number.
Understanding the inheritance pattern of HSP is crucial for genetic counseling and accurate diagnosis. Genes like SPG11‚ SPG30‚ SPG5A‚ and SPG46 have been linked to autosomal recessive forms of HSP‚ each manifesting with distinct clinical presentations. The identification of these genetic loci aids in personalized treatment approaches and management strategies.

Individuals with HSP should be aware of the genetic basis of the condition to comprehend the risk of inheritance and the variability of symptoms among different forms of HSP. Genetic counseling and testing can provide valuable insights into the specific gene mutations associated with autosomal recessive HSP and guide families in making informed decisions regarding their healthcare.
Clinical Features of Autosomal Recessive Spastic Paraplegia
The clinical features of autosomal recessive spastic paraplegia vary depending on the specific genetic form. Individuals with SPG11 may experience muscle stiffness progressing to lower limb paralysis and additional neurological symptoms like speech difficulties‚ intellectual disability‚ and bladder control issues.
SPG30‚ initially considered rare‚ can present with a spectrum of phenotypes‚ including spastic gait and weakness. In contrast‚ SPG5A is characterized by progressive spastic paraplegia and can have a complex presentation involving cerebellar signs‚ muscle atrophy‚ and cognitive impairment.
Understanding the distinct clinical features of autosomal recessive spastic paraplegia forms is crucial for accurate diagnosis and appropriate management. It is essential for individuals affected by these conditions to seek medical advice for tailored care and support resources to enhance their quality of life.
Diagnosis and Molecular Pathophysiology
Diagnosing Autosomal Recessive Spastic Paraplegia involves a multidimensional approach. Clinical evaluation with a focus on spastic gait‚ muscle weakness‚ and additional neurological symptoms is essential. Genetic testing plays a crucial role in identifying specific gene mutations associated with forms like SPG11‚ SPG30‚ and SPG5A.
Molecular pathophysiology of autosomal recessive Spastic Paraplegia often involves mutations in genes like SPG11 or KIF1A‚ leading to progressive muscle stiffness and neurological manifestations. Understanding these molecular mechanisms aids in accurate diagnosis and potentially targeted therapeutic interventions.
Individuals suspected of Autosomal Recessive Spastic Paraplegia should seek consultation with genetic specialists for comprehensive genetic testing and counseling. Early diagnosis not only helps in initiating appropriate management strategies but also enables individuals to access evolving treatment options and participate in research advancements.
Spastic Paraplegia Type 11 (SPG11)
Spastic Paraplegia Type 11 (SPG11) is a form of hereditary spastic paraplegia characterized by worsening muscle stiffness leading to lower limb paralysis. Individuals with SPG11 may also experience other neurological symptoms like speech difficulties‚ intellectual disability‚ and bladder control issues.
Understanding the specific features of SPG11 is vital for accurate diagnosis and personalized treatment plans. It is recommended for individuals presenting with symptoms of SPG11 to consult healthcare professionals specialized in genetic disorders for comprehensive evaluation and management strategies tailored to their unique needs.
Treatment and Management Strategies
The management of Autosomal Recessive Spastic Paraplegia focuses on symptom relief‚ physical rehabilitation‚ and supportive care. Treatment plans often include physical therapy to maintain mobility and strength. Assistive devices like canes or wheelchairs may be recommended to enhance mobility.
Additionally‚ management strategies for specific forms like SPG11 or SPG5A involve multidisciplinary approaches‚ including speech therapy for speech difficulties and cognitive interventions for intellectual disability. Regular monitoring by healthcare professionals is essential to adjust treatment regimens as needed.
Individuals with Autosomal Recessive Spastic Paraplegia benefit from personalized care plans that address their unique symptoms and challenges. Engaging in a support network‚ including genetic counselors‚ healthcare providers‚ and patient advocacy groups‚ can provide valuable resources for managing the condition effectively.
Support Resources for Individuals with HSP
For individuals living with Hereditary Spastic Paraplegia (HSP)‚ accessing support resources is essential for holistic care. Organizations like the Genetic Alliance‚ the Lilly Blair Foundation‚ and the National Organization for Rare Disorders can provide valuable information‚ advocacy‚ and community connections.
Genetic counselors play a crucial role in offering guidance on genetic testing‚ inheritance patterns‚ and family planning. Additionally‚ engaging with patient advocacy groups can offer emotional support and shared experiences with others facing similar challenges associated with HSP.
Individuals‚ families‚ friends‚ and caregivers impacted by HSP should explore these support resources to enhance their understanding of the condition‚ access updated information on treatments and research‚ and connect with a supportive community for shared insights and encouragement.
Future Research and Developments in HSP
Research in Hereditary Spastic Paraplegia (HSP) is rapidly evolving‚ with a focus on understanding the genetic basis‚ molecular pathophysiology‚ and developing targeted therapies. Future studies aim to uncover additional genetic loci associated with HSP‚ expanding the spectrum of known genes and inheritance patterns.
Advancements in genetic technologies‚ such as next-generation sequencing‚ continue to enhance diagnostic capabilities‚ enabling more precise identification of gene mutations linked to HSP subtypes like SPG11‚ SPG30‚ and SPG5A. This deeper genetic understanding opens avenues for personalized treatment approaches.
Furthermore‚ ongoing research endeavors seek to elucidate the intricate mechanisms underlying HSP pathogenesis‚ paving the way for innovative therapeutic interventions that may modify disease progression. Collaborative efforts between researchers‚ clinicians‚ and individuals affected by HSP aim to improve diagnostic accuracy‚ treatment outcomes‚ and ultimately enhance the quality of life for those living with this condition.