Introduction
Posterior Uveitis‚ also known as choroiditis‚ refers to inflammation of the choroid‚ potentially leading to permanent vision loss by affecting the retina and/or optic nerve. It can be part of herpetic diseases or caused by microorganisms‚ toxins‚ or tissue damage.
Definition of Posterior Uveitis
Posterior Uveitis‚ also known as choroiditis‚ refers to inflammation of the choroid‚ which can damage the optic nerve and retina‚ potentially leading to permanent vision loss. This condition can be caused by various factors‚ including infections‚ autoimmune diseases‚ and toxins.
Causes and Risk Factors
Posterior uveitis can be caused by various factors‚ including infections‚ autoimmune diseases‚ and toxins. It is important to understand the risk factors associated with this condition‚ as they can help in prevention and management strategies.
Herpes Viruses and Posterior Uveitis
Posterior uveitis caused by herpes viruses can present as part of herpetic diseases or as an isolated condition. Herpetic posterior uveitis is often acute and severe‚ leading to potentially serious complications such as retinal detachment and proliferative vitreoretinopathy.
Microorganisms‚ Toxins‚ and Tissue Damage
Posterior uveitis‚ also known as choroiditis‚ can be triggered by microorganisms‚ toxins‚ or tissue damage. Infections‚ exposure to harmful substances‚ or underlying health conditions can lead to the inflammation of the choroid‚ impacting the optic nerve and retina.
Symptoms and Diagnosis
Posterior uveitis can manifest with symptoms such as blurred vision‚ eye pain‚ sensitivity to light‚ and floaters. Diagnosis involves a thorough eye examination‚ imaging tests like OCT or fluorescein angiography‚ and analyzing the patient’s medical history for underlying conditions.
Identification of Posterior Uveitis Symptoms
Posterior uveitis is characterized by symptoms such as blurred vision‚ eye pain‚ sensitivity to light‚ and the presence of floaters. These signs can help in identifying the inflammation affecting the back part of the eye that includes the retina and/or choroid.
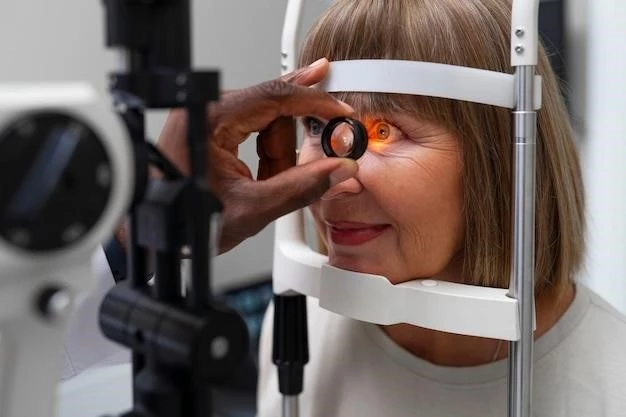
Diagnostic Methods for Posterior Uveitis
Diagnostic methods for posterior uveitis involve a comprehensive eye examination to assess inflammation in the back part of the eye; Imaging tests like optical coherence tomography (OCT) and fluorescein angiography are used to visualize and evaluate the extent of damage to the retina and choroid. Additionally‚ analyzing the patient’s medical history and symptoms helps in determining the underlying cause of posterior uveitis.
Treatment Options
Medical management with ocular or systemic therapy and surgical interventions play a crucial role in treating posterior uveitis. The goal is to control inflammation to prevent vision loss while managing potential side effects of therapy effectively.
Goal of Treatment for Posterior Uveitis
The primary objective in treating posterior uveitis is to control inflammation effectively to prevent vision loss and maintain ocular health. Therapeutic interventions aim to manage the inflammatory response while minimizing potential complications associated with the condition.
Medical Management and Surgical Interventions
Medical management with ocular or systemic therapy plays a key role in treating posterior uveitis. Additionally‚ surgical interventions are utilized for diagnostic or therapeutic purposes and for managing complications associated with uveitis effectively.
Management Strategies
Oral prednisone is commonly used for intermediate and panuveitis to manage inflammation. Advances in treating noninfectious posterior uveitis focus on optimizing inflammation control through local and systemic therapies‚ aiming to preserve vision and prevent complications.
Oral Prednisone for Intermediate and Panuveitis
In cases of intermediate and panuveitis‚ oral prednisone is commonly prescribed to manage inflammation effectively. Starting with an appropriate dosage helps in controlling the inflammatory response and minimizing the risk of complications‚ such as retinal involvement‚ which can potentially lead to vision loss if left untreated.
Latest Advances in Treating Noninfectious Posterior Uveitis
Recent advancements in managing noninfectious posterior uveitis focus on tailoring treatment approaches to optimize inflammation control. Updated strategies involve ruling out infectious causes‚ utilizing a combination of local and systemic therapies‚ and ensuring proactive measures to preserve vision and avert potential complications associated with posterior uveitis.
Complications and Prognosis
Posterior uveitis can lead to serious complications such as retinal detachment and proliferative vitreoretinopathy‚ resulting in vision loss. Permanent damage to the eye’s structures may occur‚ affecting the overall prognosis of individuals with this condition.
Retinal Detachment and Proliferative Vitreoretinopathy
Posterior uveitis can lead to complications like retinal detachment and proliferative vitreoretinopathy‚ both of which can severely impact vision. It is crucial to address these complications promptly to prevent permanent damage and preserve visual acuity.
Vision Loss and Permanent Damage
Complications of posterior uveitis‚ such as retinal detachment and proliferative vitreoretinopathy‚ can lead to vision loss. Additionally‚ the inflammation and damage to the eye’s structures may result in permanent visual impairment if not appropriately managed.

Prevention and Lifestyle
Timely treatment is crucial in preventing complications of posterior uveitis and preserving vision. Regular monitoring and follow-up care are essential to manage the condition effectively and maintain eye health.
Importance of Timely Treatment
Timely treatment for posterior uveitis is crucial to prevent complications such as vision loss and permanent damage to the eye’s structures. Regular monitoring and follow-up care are essential to ensure effective management and preservation of visual acuity.
Monitoring and Follow-Up Care
Regular monitoring and follow-up care are essential in managing posterior uveitis effectively. This proactive approach ensures timely intervention‚ ongoing assessment of treatment efficacy‚ and the prevention of potential complications that could impact the patient’s visual health in the long term.
