Overview of Orotic Aciduria Hereditary
Orotic aciduria (AKA hereditary orotic aciduria) is a disease resulting from decreased pyrimidine synthesis ability due to an enzyme deficiency․ This disorder involves excessive orotic acid excretion in urine․
Definition and Causes
Orotic aciduria is an autosomal recessive disorder caused by deficiency of uridine monophosphate synthase enzyme, impacting pyrimidine synthesis․ Patients often present with megaloblastic anemia, growth delays, and increased orotic acid levels in urine due to enzyme deficiencies in the metabolic pathway․
Clinical Manifestations
Orotic aciduria hereditary manifests with symptoms such as megaloblastic anemia, developmental delays, and increased urinary excretion of orotic acid due to enzymatic deficiencies in pyrimidine synthesis․ Patients may present with growth retardation and hematologic abnormalities․
Genetic Aspects of Hereditary Orotic Aciduria
Orotic aciduria hereditary is an autosomal recessive disorder linked to deficiencies in pyrimidine synthesis enzymes due to genetic mutations affecting the UMPS gene․ These mutations lead to impaired conversion of orotic acid to uridine monophosphate․
Autosomal Recessive Inheritance
Orotic aciduria hereditary follows an autosomal recessive pattern of inheritance, with mutations in the UMPS gene leading to deficient pyrimidine synthesis enzymes․ Individuals must inherit two mutated copies of the gene to develop the disorder․
Enzyme Deficiencies
Orotic aciduria hereditary is characterized by deficiencies in enzymes involved in pyrimidine synthesis, specifically uridine monophosphate synthase․ These enzymatic deficiencies disrupt the conversion of orotic acid to uridine monophosphate, leading to the clinical manifestations of the disorder․
Orotic aciduria hereditary can be diagnosed through a urinary screening test based on excessive orotic acid excretion․ Enzymatic diagnosis can further confirm deficiencies in pyrimidine synthesis enzymes․
Urinary Screening Test
A urinary screening test is employed for the diagnosis of hereditary orotic aciduria, focusing on the excessive excretion of orotic acid․ The test involves specific chemical reactions to confirm elevated orotic acid levels in urine, indicating possible deficiencies in pyrimidine synthesis enzymes․
Diagnosis and Screening Tests
Diagnosis of hereditary orotic aciduria involves conducting a urinary screening test focusing on elevated levels of orotic acid․ Subsequent enzymatic diagnosis is performed to confirm deficiencies in pyrimidine synthesis enzymes, aiding in the accurate identification of the disorder․
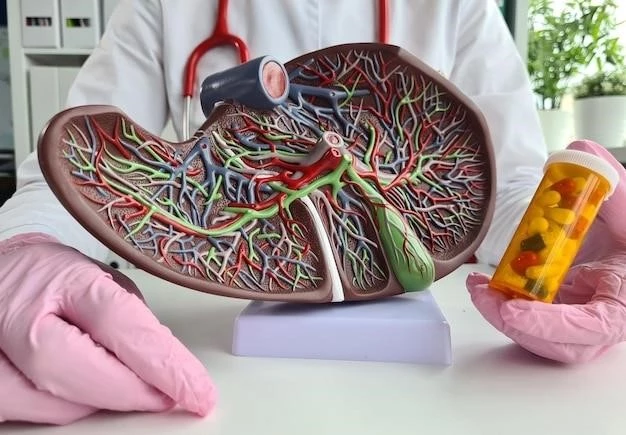
Treatment and Management
Hereditary orotic aciduria can be managed through uridine therapy and pyrimidine replacement therapy to address the enzymatic deficiencies affecting pyrimidine synthesis pathways․ These treatments aim to alleviate symptoms and improve patient outcomes․
Uridine Therapy
Uridine therapy is a crucial component in the treatment of hereditary orotic aciduria, aiming to supplement the deficient pyrimidine pathways․ By providing uridine, the therapy supports the synthesis of essential nucleotides, addressing the enzymatic deficiencies and improving patient outcomes․
Pyrimidine Replacement Therapy
Pyrimidine replacement therapy is a key aspect of managing hereditary orotic aciduria by supplementing the deficient pyrimidine synthesis pathways․ This therapy aims to restore the balance of pyrimidine nucleotides, addressing the enzymatic deficiencies that lead to clinical symptoms and improving patient outcomes․
Prognosis and Outlook
Prompt diagnosis and appropriate treatment significantly impact the prognosis of hereditary orotic aciduria, leading to improved outcomes and quality of life for affected individuals․ Early intervention with targeted therapies can help manage symptoms effectively․
Response to Treatment
Patients with hereditary orotic aciduria typically show positive responses to targeted therapies such as uridine supplementation and pyrimidine replacement․ These treatments help alleviate symptoms, improve hematologic parameters, and aid in the overall management of the disorder․
Long-Term Implications
The long-term implications of hereditary orotic aciduria include the potential for growth retardation, neurodevelopmental consequences, and ongoing management of hematologic abnormalities․ Monitoring and continued treatment are essential to address these implications and ensure optimal outcomes for affected individuals․
Epidemiology and Prevalence
Hereditary orotic aciduria is an exceptionally rare disorder, with a prevalence estimated to be less than 1 in 1,000,000 live births․ This autosomal recessive condition affects a very small number of individuals globally, highlighting its rarity in the population․
Rarity of the Disorder
Hereditary orotic aciduria is an exceptionally rare disorder, with limited documented cases worldwide․ This autosomal recessive condition has an extremely low prevalence, highlighting the rarity and infrequency of the disorder in the global population․
Birth Prevalence
The birth prevalence of hereditary orotic aciduria is estimated to be less than 1 in 1,000,000 live births․ This rarity underscores the low occurrence of the disorder at birth, highlighting the importance of early recognition and management in affected individuals․
Newborn Screening and Early Detection
Early detection of hereditary orotic aciduria through newborn screening is crucial for timely intervention and management․ Identifying the disorder in newborns allows for prompt treatment initiation and improved clinical outcomes for affected individuals․
Importance of Early Diagnosis
Early diagnosis of hereditary orotic aciduria through newborn screening is crucial for timely intervention and initiation of appropriate therapies․ Detecting the disorder in newborns allows for early treatment, which can significantly impact long-term outcomes and prevent complications associated with the condition․
Impact on Disease Course
Early detection through newborn screening and subsequent early intervention can have a significant impact on the disease course of hereditary orotic aciduria․ Timely identification allows for the initiation of appropriate treatments, potentially improving long-term outcomes and mitigating the progression of the disorder․
Hereditary orotic aciduria results from deficiency in the enzyme uridine monophosphate synthase (UMPS), impacting the final step of pyrimidine biosynthesis․ This deficiency leads to the accumulation of orotic acid in urine due to the impaired conversion to uridine monophosphate․
Mutation Analysis
Hereditary orotic aciduria is associated with mutations in the UMPS gene, leading to deficient uridine monophosphate synthase enzyme activity․ These mutations disrupt the final pyrimidine biosynthesis step, resulting in impaired conversion of orotic acid to uridine monophosphate․
Molecular Basis of Hereditary Orotic Aciduria
Hereditary orotic aciduria results from a deficiency in the uridine monophosphate synthase enzyme, impacting pyrimidine biosynthesis; This deficiency leads to disrupted conversion of orotic acid to uridine monophosphate, affecting nucleotide synthesis․
Hereditary orotic aciduria presents with symptoms such as anemia with large immature red blood cells and delays in growth and development․ The condition is characterized by elevated levels of orotic acid in urine and is associated with enzymatic deficiencies in pyrimidine synthesis pathways․
Symptomatology and Clinical Presentation
Hereditary orotic aciduria presents clinically with anemia characterized by large immature red blood cells and growth delays․ Patients may exhibit elevated urinary levels of orotic acid due to enzymatic deficiencies in pyrimidine synthesis, leading to distinct clinical manifestations․
Hereditary orotic aciduria is associated with growth retardation and developmental delays, including physical and intellectual development․ The condition’s enzymatic deficiencies in pyrimidine synthesis pathways contribute to these delays, highlighting the importance of early diagnosis and intervention․
Enzyme Deficiency and Pyrimidine Synthesis
Hereditary orotic aciduria results from a deficiency in the uridine monophosphate synthase (UMPS) enzyme, impacting the final step of pyrimidine synthesis․ This deficiency leads to disrupted conversion of orotic acid to uridine monophosphate, affecting nucleotide synthesis․
Growth and Developmental Delays
Individuals with hereditary orotic aciduria may experience growth retardation and developmental delays affecting their physical and intellectual development․ These delays are linked to the enzymatic deficiencies in pyrimidine synthesis, underscoring the importance of early detection and management․
Effects on Pyrimidine Biosynthesis
Its hereditary form, an autosomal recessive disorder, can be caused by a deficiency in the enzyme UMPS, a bifunctional protein that includes the enzyme activities of orotate phosphoribosyltransferase and orotidine 5-phosphate decarboxylase․ Orotic aciduria has an autosomal recessive of inheritance․ It can also arise secondary to blockage of ․․․
Association with Other Disorders
Hereditary orotic aciduria is a genetic disorder resulting from deficiencies in pyrimidine biosynthesis enzymes․ Its clinical manifestations include anemia, growth delays, and extensive orotic acid excretion in urine due to impaired pyrimidine synthesis․
Relationship to Urea Cycle Defects
While hereditary orotic aciduria is primarily associated with enzyme deficiencies in pyrimidine biosynthesis, it can also occur as a secondary condition related to urea cycle defects, parenteral nutrition, or essential amino acid deficiency․ The coexistence of urea cycle defects may contribute to the development of orotic aciduria in affected individuals․
Secondary Causes of Orotic Aciduria
In addition to being a primary genetic disorder, hereditary orotic aciduria can also manifest as a secondary condition, often associated with urea cycle defects, parenteral nutrition, or essential amino acid deficiencies․ These secondary causes may contribute to the development of orotic aciduria alongside other metabolic disruptions․
Impact of Hereditary Orotic Aciduria
Hereditary orotic aciduria can lead to various consequences, including neurodevelopmental issues and effects on multiple organ systems․ The disorder’s impact on patients underscores the need for comprehensive management strategies;
Neurodevelopmental Consequences
Hereditary orotic aciduria can have significant neurodevelopmental consequences, potentially leading to delays in cognitive and physical development․ The disorder’s impact on the nervous system underscores the importance of early intervention and comprehensive care to address these specific challenges․
Effects on Organ Systems
Hereditary orotic aciduria can impact various organ systems due to enzymatic deficiencies affecting pyrimidine biosynthesis․ Patients may experience manifestations such as anemia, growth delays, and distinctive urinary excretion patterns, highlighting the systemic consequences of the disorder․
Research Advances and Insights
Research on hereditary orotic aciduria has provided valuable insights into the genetic basis and biochemical pathways involved in the disease․ Recent findings have shed light on potential therapeutic targets and management strategies for affected individuals, highlighting the ongoing advancements in understanding this rare disorder․
Recent Findings in Genetic Studies
Recent genetic studies have unveiled crucial insights into the molecular basis of hereditary orotic aciduria, particularly focusing on mutations in the UMPS gene responsible for deficient uridine monophosphate synthase activity․ These findings contribute to a deeper understanding of the disorder’s genetic underpinnings and potential therapeutic targets․
Molecular Characterization of the Disorder
Further research has focused on the molecular characterization of hereditary orotic aciduria, revealing specific gene mutations that underlie the deficiency in uridine monophosphate synthase enzyme․ Understanding these molecular mechanisms is essential for advancing diagnostic methods and developing targeted therapies for affected individuals․
Managing hereditary orotic aciduria involves addressing clinical challenges such as anemia and growth delays through uridine therapy and pyrimidine replacement strategies․ Multidisciplinary care teams play a crucial role in developing comprehensive management plans for affected individuals․
Clinical Challenges and Management Strategies
Clinical challenges in hereditary orotic aciduria encompass addressing anemia, growth delays, and urinary orotic acid excretion․ Management strategies include uridine therapy and pyrimidine replacement approaches to mitigate symptoms and enhance patient outcomes․
Multidisciplinary Care Teams
In managing hereditary orotic aciduria, a multidisciplinary care team approach is crucial․ Various specialists collaborate to tailor individualized treatment plans addressing anemia, growth delays, and metabolic aspects of the disorder․ This comprehensive approach ensures holistic care for affected individuals․
Future Directions in Orotic Aciduria Research
Further research in hereditary orotic aciduria aims to explore novel therapeutic innovations and advance genetic counseling strategies to enhance patient outcomes․ Focuses on understanding the disease’s molecular mechanisms and developing targeted treatment approaches are essential for future directions in orotic aciduria research․
Therapeutic Innovations
This rare genetic disorder known as hereditary orotic aciduria is characterized by its link to pyrimidine biosynthesis enzyme deficiencies․ These deficiencies lead to clinical manifestations such as anemia, growth delays, and distinctive urinary excretion patterns․
Genetic Counseling and Family Planning
Based on recent data, Hereditary Orotic Aciduria is a rare autosomal recessive disorder characterized by excessive excretion of orotic acid due to enzyme deficiencies in pyrimidine biosynthesis pathways․ This condition typically presents with anemia and growth delays, requiring specialized treatment approaches for optimal management․