Causes of Ankyloblepharon filiforme imperforate anus
– Genetic factors
– Developmental abnormalities
– Environmental influences
– Genetic factors
Genetic abnormalities during fetal development can play a role, impacting the formation of the anal opening and surrounding tissues.
– Developmental abnormalities
Issues during the formation of the anorectal region in the embryo may lead to improper development of the anal canal and adjacent structures.
– Environmental influences
External factors like exposure to toxins, infections, or certain medications during pregnancy can contribute to the development of ankyloblepharon filiforme imperforate anus.
Symptoms of Ankyloblepharon filiforme imperforate anus
– Absence of anal opening
– Skin covering the anal opening
– Difficulty passing stool
– Absence of anal opening
This symptom is a key indicator, where the newborn lacks a visible anal opening, indicating potential issues with anorectal development.
– Skin covering the anal opening
In cases of imperforate anus, a thin membrane or skin may obstruct the anal opening, causing complications in stool passage and requiring medical attention.
– Difficulty passing stool
The presence of an imperforate anus can lead to challenges in passing stool due to the blockage or narrowing of the anal opening, necessitating prompt medical evaluation and intervention.
Treatment options for Ankyloblepharon filiforme imperforate anus
– Stoma creation
– Surgical correction
– Medication management
– Stoma creation
In cases where a direct correction is not immediately feasible, a stoma may be surgically created to divert fecal matter and manage the condition effectively.
– Surgical correction
Various surgical procedures are available to repair the anatomical defect, allowing for the creation of a functional anal opening and improving the patient’s quality of life.
– Medication management
In some cases, medications like laxatives or stool softeners may be prescribed to help regulate bowel movements and alleviate constipation issues associated with ankyloblepharon filiforme imperforate anus.
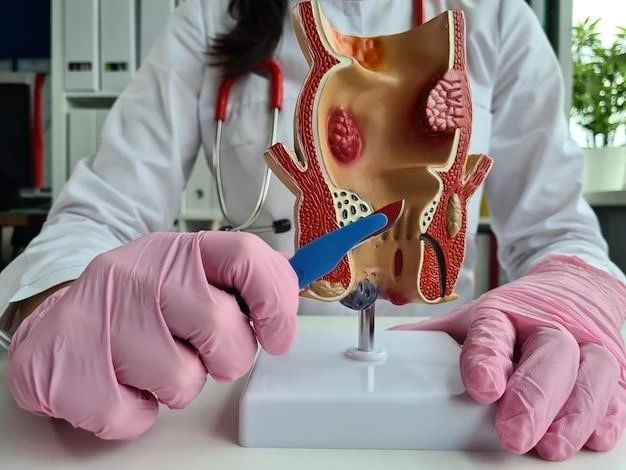
Surgical procedures for Ankyloblepharon filiforme imperforate anus
– Posterior sagittal anorectoplasty (PSARP)
– Colostomy
– Anal dilatation procedures
– Posterior sagittal anorectoplasty (PSARP)
PSARP is a surgical technique used to reconstruct the anal region, creating a new anal opening and correcting any associated defects in patients with ankyloblepharon filiforme imperforate anus.
– Colostomy
Colostomy is a procedure where an opening, called a stoma, is created in the abdominal wall to divert stool, alleviating temporary bowel complications in individuals with ankyloblepharon filiforme imperforate anus.
– Anal dilatation procedures
Anal dilatation involves gently stretching the anal canal to promote proper function and alleviate issues related to ankyloblepharon filiforme imperforate anus, aiding in bowel movement regularity.

Ankyloblepharon filiforme imperforate anus in infants
– Diagnosis challenges in newborns
– Early intervention strategies
– Parental support and education
– Diagnosis challenges in newborns
Diagnosing ankyloblepharon filiforme imperforate anus in infants can be challenging due to variations in symptoms and the need for specialized medical evaluation to confirm the condition accurately.
– Early intervention strategies
Early intervention through prompt medical care and surgical correction can improve outcomes, ensuring optimal anorectal function and overall well-being in infants with ankyloblepharon filiforme imperforate anus.
– Parental support and education
Offering parents guidance, emotional support, and information about the condition is vital to help them navigate the challenges of caring for an infant with ankyloblepharon filiforme imperforate anus.
Complications of Ankyloblepharon filiforme imperforate anus
– Constipation
– Fecal incontinence
– Urinary tract infections
– Constipation
Constipation can arise as a complication of ankyloblepharon filiforme imperforate anus, leading to discomfort and difficulty in passing stool, requiring management to prevent further complications.
– Fecal incontinence
Fecal incontinence may occur in individuals with ankyloblepharon filiforme imperforate anus, resulting in the inability to control stool passage, impacting daily life and necessitating appropriate management strategies.
– Urinary tract infections
Urinary tract infections can develop as a complication of ankyloblepharon filiforme imperforate anus, necessitating prompt medical attention to prevent further health issues and ensure proper management of the condition.
Prognosis of Ankyloblepharon filiforme imperforate anus
– Long-term outcomes
– Quality of life considerations
– Follow-up care recommendations
– Long-term outcomes
Long-term outcomes for individuals with ankyloblepharon filiforme imperforate anus can vary, with some experiencing bowel control improvements post-treatment, while others may require ongoing management strategies for optimal quality of life.
– Quality of life considerations
Factors such as continence, social well-being, and psychosocial support play crucial roles in enhancing the quality of life for individuals living with ankyloblepharon filiforme imperforate anus, emphasizing a holistic approach to care.
Research updates on Ankyloblepharon filiforme imperforate anus
– Advances in surgical techniques
– Genetic studies on causative factors
– Future treatment possibilities