Lipomatosis Central Non-Encapsulated
Lipomatosis central non-encapsulated is a rare disorder characterized by benign growth of adipose tissue. It can lead to fat accumulation in various parts of the body. Anderson lipomatosis, Cushing’s syndrome, dyslipidemia, HIV, and protease inhibitors are some associated factors.
Understanding Lipomatosis
Lipomatosis central non-encapsulated is a rare condition characterized by the non-cancerous growth of adipose tissue, resulting in the enlargement of fatty masses in different areas of the body. The condition is also known as Madelung’s disease or benign symmetric lipomatosis.
These fatty masses typically develop around the neck, shoulders, upper arms, and upper trunk. They are usually soft to the touch and may cause cosmetic concerns for affected individuals. Lipomatosis central non-encapsulated is more common in males, particularly those with a history of alcohol abuse.
While the exact cause of lipomatosis is not fully understood, it is believed to be associated with metabolic abnormalities, genetic factors, and hormonal imbalances. Individuals with certain underlying conditions like Anderson lipomatosis, Cushing’s syndrome, dyslipidemia, HIV infection, or the use of protease inhibitors may be at increased risk of developing lipomatosis.
Understanding the nature of lipomatosis and its potential complications is crucial for accurate diagnosis and management. Treatment options may include surgical removal of the fatty masses for symptomatic relief or to address cosmetic concerns. However, recurrence of lipomatosis after surgery is possible.
Causes of Lipomatosis
The exact causes of lipomatosis central non-encapsulated are not fully understood, but several factors have been identified as potential contributors to the development of this condition. One of the main theories suggests that lipomatosis may be linked to genetic mutations that affect the regulation of fat cell growth and metabolism.
Individuals with certain underlying conditions are more predisposed to developing lipomatosis. For instance, Anderson lipomatosis, a genetic disorder characterized by multiple fatty deposits in the body, has been associated with an increased risk of lipomatosis central non-encapsulated.
Cushing’s syndrome, a hormonal disorder that leads to high levels of cortisol in the body, is another condition that may contribute to the development of lipomatosis. Dyslipidemia, a condition characterized by abnormal levels of lipids in the blood, has also been linked to the formation of adipose tissue growths.
In addition, individuals living with HIV who are taking protease inhibitors as part of their treatment regimen may be at a higher risk of developing lipomatosis central non-encapsulated; These medications are known to affect fat metabolism and distribution in the body, potentially leading to the accumulation of adipose tissue in various locations.
Understanding the underlying causes of lipomatosis is essential for effective management and treatment strategies. Research into the genetic, hormonal, and metabolic factors involved in the development of this condition is ongoing to improve diagnostic methods and therapeutic interventions.
Symptoms and Diagnosis
Lipomatosis central non-encapsulated may present with various symptoms, including the development of non-cancerous fatty masses in different regions of the body. These masses are typically soft to the touch and can cause cosmetic concerns due to their size and distribution.
Individuals with lipomatosis may experience discomfort or restricted movement in areas where the fatty deposits have accumulated. In some cases, the enlargement of these adipose tissue growths can lead to compression of nearby structures, causing symptoms such as pain or numbness.
Diagnosing lipomatosis often involves a physical examination to assess the size, location, and texture of the fatty masses. Imaging studies like ultrasound, MRI, or CT scans may be used to visualize the extent of adipose tissue enlargement and determine the involvement of surrounding tissues.
In cases where there is uncertainty about the nature of the fatty masses, a biopsy may be performed to confirm the diagnosis of lipomatosis. Biopsies involve the removal of a small sample of tissue for laboratory analysis to rule out malignancy and establish the non-cancerous nature of the growths.
It is essential for healthcare providers to consider the individual’s medical history, including any underlying conditions like Anderson lipomatosis, Cushing’s syndrome, dyslipidemia, HIV infection, or the use of protease inhibitors, when evaluating symptoms and making a diagnosis of lipomatosis central non-encapsulated.
Treatment Options
The treatment of lipomatosis central non-encapsulated aims to address symptoms, improve cosmetic appearance, and prevent complications associated with the growth of adipose tissue. The choice of treatment depends on factors such as the size, location, and number of fatty masses, as well as the individual’s overall health.
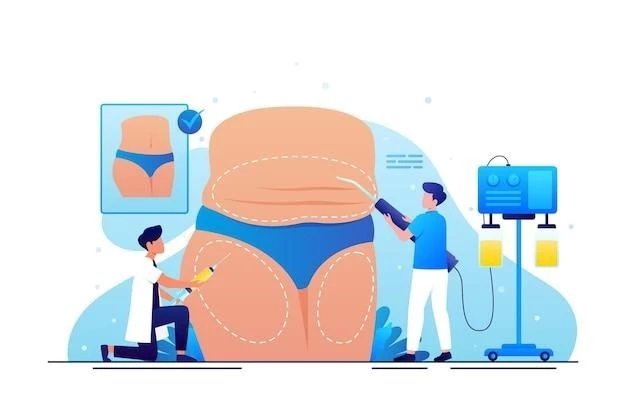
Surgical removal, or excision, is a common treatment option for lipomatosis. This procedure involves the physical extraction of the fatty masses through incisions in the skin. Surgical excision is often recommended for symptomatic or large lipomatosis growths that affect mobility or cause discomfort.
Liposuction, a minimally invasive procedure that suctions out fat deposits through a thin tube called a cannula, may also be considered for the treatment of lipomatosis; Liposuction can help reduce the size of fatty masses and improve cosmetic appearance, especially in areas where surgical excision may not be feasible.
In cases where surgical intervention is not preferred or feasible, non-surgical options such as steroid injections or lipolysis (injection of substances to break down fat cells) may be explored to reduce the size of the fatty deposits. These non-invasive treatments are generally used for smaller lipomatosis growths.
Regular monitoring and follow-up are essential for individuals with lipomatosis to evaluate the growth of adipose tissue, assess symptoms, and address any potential complications. Treatment decisions should be made in consultation with healthcare providers based on the individual’s specific circumstances and preferences.
Lipomatosis in Rare Disorders
Lipomatosis central non-encapsulated has been observed in association with certain rare disorders that are characterized by abnormal fat accumulation in the body. One such condition is Anderson lipomatosis, a genetic disorder that leads to the development of multiple lipomas or fatty deposits.
Individuals with Anderson lipomatosis may present with symmetric distribution of fatty masses in various body regions, resembling the pattern seen in lipomatosis central non-encapsulated. The underlying genetic mutations responsible for Anderson lipomatosis contribute to the unregulated growth of adipose tissue.
Cushing’s syndrome, a hormonal disorder caused by prolonged exposure to high levels of cortisol, has also been linked to the development of lipomatosis. The excess cortisol in the body can disrupt fat metabolism and distribution, leading to the accumulation of adipose tissue in different areas.
Moreover, dyslipidemia, a condition characterized by abnormalities in lipid levels, can result in the formation of fatty masses similar to those seen in lipomatosis central non-encapsulated. Dyslipidemia may alter the way fats are processed and stored in the body, contributing to the enlargement of fatty deposits.
Understanding the relationship between lipomatosis and these rare disorders is essential for accurate diagnosis and management. Healthcare providers should consider the presence of Anderson lipomatosis, Cushing’s syndrome, or dyslipidemia when evaluating individuals with lipomatosis central non-encapsulated to provide appropriate care and address potential underlying conditions.
Lipomatosis in HIV Patients
Individuals living with HIV may experience lipomatosis central non-encapsulated as a result of the infection itself or the use of antiretroviral medications, particularly protease inhibitors. HIV infection can lead to metabolic imbalances and alterations in fat distribution, contributing to the abnormal growth of adipose tissue.
Protease inhibitors, a class of antiretroviral drugs commonly used in HIV treatment, have been associated with metabolic complications such as lipodystrophy and lipomatosis. These medications can interfere with fat metabolism and lead to the accumulation of fat in specific areas of the body, including the neck, abdomen, and trunk.
Lipomatosis in HIV patients can impact quality of life and may cause distress due to changes in body shape and appearance. The accumulation of adipose tissue in visible areas can result in cosmetic concerns and emotional challenges for individuals living with HIV.
Management of lipomatosis in HIV patients often involves a multidisciplinary approach that addresses both the underlying HIV infection and the metabolic consequences of antiretroviral therapy. Healthcare providers may consider modifying medication regimens, implementing lifestyle changes, or exploring surgical options to address lipomatosis and improve patient outcomes.
Regular monitoring and communication between healthcare providers and HIV patients are crucial to assess the progression of lipomatosis, manage symptoms effectively, and provide necessary support and guidance to optimize the overall well-being of individuals living with both HIV and lipomatosis central non-encapsulated.
Complications and Risks
Lipomatosis central non-encapsulated, while typically benign, can present certain complications and risks, particularly when the growth of adipose tissue affects surrounding structures or leads to functional impairments. One of the potential risks of lipomatosis is the compression of nerves, blood vessels, or organs by the enlarged fatty masses.
In cases where lipomatosis growths impinge on nerves, individuals may experience symptoms such as pain, tingling, numbness, or weakness in the affected areas. Compression of blood vessels by adipose tissue can restrict blood flow, potentially causing ischemia or other vascular complications.
Furthermore, the enlargement of fatty masses in critical regions of the body can lead to functional limitations and cosmetic concerns. Mobility restrictions, discomfort, or changes in body shape may impact the quality of life and psychological well-being of individuals with lipomatosis.
Although lipomatosis central non-encapsulated is non-cancerous, the presence of extensive adipose tissue growths can result in challenges related to diagnosis, treatment, and recurrence. Surgical removal of large lipomatosis masses may carry risks such as scarring, infection, or incomplete excision.
Healthcare providers evaluating individuals with lipomatosis should be vigilant for potential complications and risks associated with the condition. Regular monitoring, appropriate imaging studies, and multidisciplinary collaboration are essential to mitigate complications, address symptoms effectively, and provide optimal care for individuals at risk of experiencing adverse outcomes related to lipomatosis central non-encapsulated.
Research and Future Perspectives
Ongoing research on lipomatosis central non-encapsulated aims to enhance understanding of the underlying mechanisms that contribute to the development and progression of this rare disorder. Studies focusing on genetic factors, metabolic pathways, and hormonal influences are crucial for advancing knowledge in the field.
Emerging technologies, such as advanced imaging modalities and genetic testing, provide valuable tools for researchers and healthcare providers to explore the complexities of lipomatosis. These advancements contribute to early detection, accurate diagnosis, and personalized treatment strategies for individuals affected by this condition.
Future perspectives in lipomatosis research may involve the development of targeted therapies that address the specific molecular pathways involved in the growth of adipose tissue. Precision medicine approaches tailored to individual genetic profiles and metabolic characteristics could revolutionize the management of lipomatosis central non-encapsulated.
Collaboration between clinicians, geneticists, endocrinologists, and researchers from various disciplines is essential to drive progress in the field of lipomatosis. By sharing insights, expertise, and data, the scientific community can work towards improving diagnostic techniques, advancing treatment options, and ultimately enhancing outcomes for individuals with lipomatosis.
Investments in research funding, clinical trials, and interdisciplinary collaborations hold promise for elucidating the complexity of lipomatosis central non-encapsulated and paving the way for innovative approaches that optimize patient care and quality of life. The pursuit of novel insights and therapeutic interventions underscores a commitment to addressing the unmet needs of individuals affected by lipomatosis.
