Managing Idiopathic Edema
Idiopathic edema can be challenging to manage, but with the right approach, it is possible to alleviate symptoms and improve quality of life. This article will provide insights on understanding, identifying, and treating idiopathic edema effectively.
Understanding Idiopathic Edema
Idiopathic edema, also known as fluid retention, is a condition where the body holds onto excess fluid, leading to swelling, weight gain, bloating, and puffiness. This can be caused by various factors, including hormonal imbalance, kidney function issues, circulatory system problems, or salt sensitivity. It is essential to address the root cause of fluid retention to effectively manage idiopathic edema.
Individuals with idiopathic edema may experience water retention due to factors such as sodium intake, proteinuria, or hypoalbuminemia. Monitoring kidney function is crucial as impaired kidney function can contribute to fluid buildup in the body. Understanding the relationship between the circulatory system and edema is key to managing symptoms.
To effectively address idiopathic edema, treatment options such as diuretics may be prescribed to help reduce fluid retention. Additionally, a sodium-restricted diet can help manage salt sensitivity and decrease water retention. It is important to work closely with healthcare providers to determine the most suitable treatment plan based on individual needs and underlying health conditions.
Identifying Signs of Edema
Recognizing the signs of edema is crucial in managing idiopathic edema effectively. Symptoms may include swelling in the hands, legs, or abdomen, weight gain, bloating, puffiness, and water retention. It is essential to pay attention to these signs and symptoms to seek appropriate medical advice.
Individuals with idiopathic edema may also experience salt sensitivity, which can worsen fluid retention. If you notice persistent swelling, especially in the lower extremities, consult a healthcare provider for further evaluation. Monitoring changes in your body weight and any unusual swelling can help in early identification of edema.
Other indicators of edema may include proteinuria, a condition characterized by the presence of excess protein in the urine, and hypoalbuminemia, low levels of albumin in the blood. If you observe these signs along with swelling or weight gain, it is important to discuss them with a healthcare professional for proper diagnosis and management.
Assessing Kidney Function in Edema
Monitoring kidney function is paramount when dealing with idiopathic edema. The kidneys play a vital role in fluid balance and waste removal from the body. Impaired kidney function can lead to fluid retention, contributing to edema. Regular kidney function tests, such as blood and urine tests, can help assess and manage kidney health.
If you have edema, it is essential to consult a healthcare provider for kidney function evaluation. Conditions like proteinuria, where excess protein is detected in the urine, can indicate kidney damage. Additionally, hypoalbuminemia, low albumin levels in the blood, can be a sign of kidney dysfunction affecting fluid balance.
By closely monitoring kidney function through routine tests, healthcare professionals can determine if kidney issues are contributing to edema. Treatment strategies tailored to improving kidney health can help alleviate fluid retention and swelling associated with idiopathic edema. Working collaboratively with your healthcare team is key to managing kidney-related factors contributing to edema.
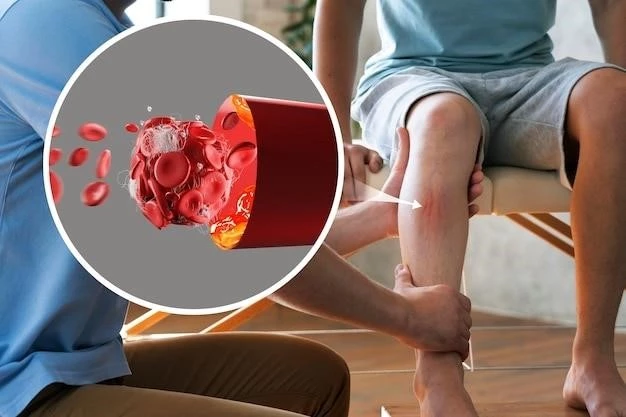
Impact of Circulatory System on Edema
The circulatory system plays a significant role in the development of edema. In idiopathic edema, poor circulation can contribute to fluid retention and swelling in various parts of the body. Understanding how the circulatory system impacts edema is crucial in managing this condition effectively.
Issues such as blood vessel damage, blood clot formation, or heart failure can hinder proper fluid movement and lead to edema. It is important to address circulatory issues that may be exacerbating fluid retention. Lifestyle changes, medication, and interventions to improve circulation can help mitigate edema symptoms.
Consulting with healthcare professionals can provide insights into how the circulatory system is affecting edema. Vascular assessments, imaging studies, and blood flow tests may be recommended to evaluate circulation and identify areas of concern. By addressing circulatory issues, individuals with idiopathic edema can work towards reducing swelling and improving overall health.
Treatment Options for Edema
Managing idiopathic edema involves various treatment options aimed at reducing fluid retention and alleviating symptoms. Diuretics are commonly prescribed to help the body eliminate excess fluids. It is essential to use diuretics under medical supervision to prevent electrolyte imbalances and monitor kidney function.
In addition to medications, lifestyle modifications can play a crucial role in managing edema. Adopting a low-sodium diet can help reduce water retention due to salt sensitivity. Regular physical activity and elevation of swollen limbs can promote circulation and decrease swelling.
Other treatment approaches for edema include compression garments, which can help reduce swelling in the affected areas. Elevating the legs above heart level and avoiding prolonged sitting or standing can also aid in fluid drainage. It is important to discuss these treatment options with a healthcare provider to determine the most suitable approach for individual needs.
Complications Related to Edema
Untreated idiopathic edema can lead to various complications that impact overall health. Prolonged fluid retention can strain the circulatory system, increasing the risk of cardiovascular issues. Severe edema may also impair mobility and quality of life, causing discomfort and limitation in daily activities.
Chronic edema can result in skin changes, such as hardening or discoloration, making the skin more susceptible to infections; In some cases, edema can progress to lymphedema, a chronic condition characterized by persistent swelling in specific areas. It is crucial to address edema promptly to prevent these complications.
Complications associated with edema may include compromised wound healing, increased risk of infections, and reduced quality of life. Seeking medical attention for persistent or worsening edema is essential to prevent complications and improve outcomes. Healthcare providers can offer guidance on managing edema and minimizing the risk of related complications.
Lifestyle Changes to Manage Edema
Implementing lifestyle modifications is key to effectively managing idiopathic edema and reducing fluid retention. One crucial change is adopting a low-sodium diet to alleviate salt sensitivity, a common cause of water retention. Limiting processed foods and consuming more fresh fruits and vegetables can help regulate fluid balance.
Regular physical activity is essential in promoting circulation and reducing swelling. Engaging in activities like walking, swimming, or cycling can enhance blood flow and decrease fluid buildup in the body. Elevating the legs periodically and avoiding prolonged sitting or standing can also aid in fluid drainage.
Adequate hydration is important in preventing dehydration, which can worsen edema. Drinking enough water throughout the day helps maintain proper fluid balance and supports kidney function. Additionally, maintaining a healthy body weight and avoiding excessive alcohol consumption can contribute to managing idiopathic edema effectively.
