Disease Overview ⏤ Ichthyosis and Male Hypogonadism
Ichthyosis is a genetic disorder characterized by dry, scaly skin, while male hypogonadism is a condition involving testosterone deficiency and issues with the male reproductive system. This article delves into the connection between these two conditions and explores how they can coexist in individuals;
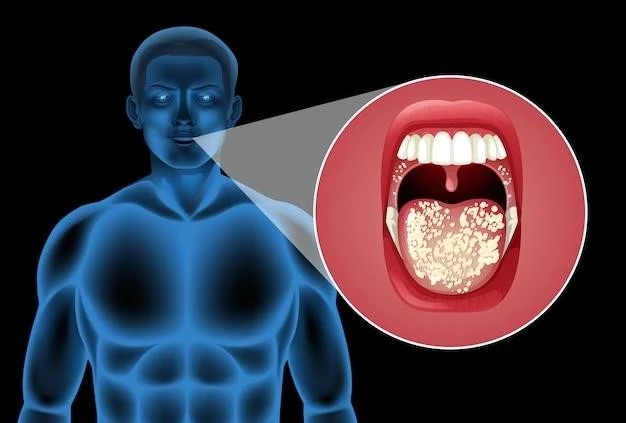
Understanding Ichthyosis
Ichthyosis is a genetic disorder that affects the skin, leading to dry, scaly patches. This condition is caused by mutations in genes that control skin cell regeneration. Individuals with ichthyosis produce skin cells at a faster rate than normal, resulting in a buildup of dry, thick scales;
There are several types of ichthyosis, with symptoms ranging from mild dryness to severe scaling across the body. These symptoms can impact a person’s quality of life, causing discomfort and self-esteem issues. While ichthyosis is typically diagnosed in infancy or early childhood, the severity can vary widely among individuals.
Management of ichthyosis involves regular skincare routines to moisturize the skin and reduce scaling. This often includes the use of emollients, bath oils, and gentle exfoliation to maintain skin health. In more severe cases, prescription medications such as steroid creams may be recommended to manage inflammation and improve skin texture.
Living with ichthyosis requires ongoing attention to skincare, as dry skin can lead to complications such as infections. Despite the challenges it presents, many individuals with ichthyosis lead fulfilling lives and find ways to effectively manage their skin condition.
Exploring Male Hypogonadism
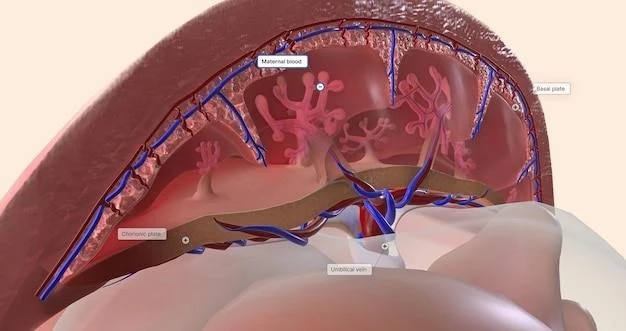
Male hypogonadism is a condition characterized by testosterone deficiency, impacting the male reproductive system and hormone production. Testosterone plays a crucial role in the development of male reproductive organs, muscle mass, and bone density. When testosterone levels are low, it can lead to various symptoms and health issues.
There are two main types of male hypogonadism⁚ primary and secondary. Primary hypogonadism occurs when the testes are unable to produce enough testosterone, often due to genetic abnormalities, infections, or testicular injury. Secondary hypogonadism involves a problem with the hypothalamus or pituitary gland, leading to inadequate hormone signaling.
Symptoms of male hypogonadism may include low libido, erectile dysfunction, reduced muscle mass, fatigue, and mood changes; In adolescents, this condition can affect puberty, delaying sexual development and growth. Long-term consequences of untreated hypogonadism can include osteoporosis and infertility.
Diagnosis of male hypogonadism involves a combination of blood tests to measure testosterone levels and imaging studies to assess the reproductive organs. Treatment options depend on the underlying cause and may include hormone replacement therapy to restore testosterone levels. Lifestyle changes, such as diet and exercise, can also have a positive impact on symptoms.
Connection Between Ichthyosis and Male Hypogonadism
While ichthyosis and male hypogonadism are distinct conditions affecting different systems in the body, there can be a connection between the two in some cases. Research suggests that individuals with certain types of ichthyosis, especially those with severe forms involving gene mutations, may be at a higher risk of hormonal imbalances, including testosterone deficiency.
The exact mechanisms underlying the link between ichthyosis and male hypogonadism are not yet fully understood but could involve genetic factors or common pathways that influence hormone production. It is important for healthcare providers to consider the possibility of concurrent conditions when assessing and treating patients with both ichthyosis and male hypogonadism.
Individuals with ichthyosis may already be managing complex skincare routines and medical treatments to address their skin condition. The addition of male hypogonadism can present additional challenges, requiring a comprehensive approach to address both the dermatological and endocrine aspects of their health.
Collaboration between dermatologists and endocrinologists is crucial to provide integrated care for individuals with both ichthyosis and male hypogonadism. By understanding the potential interplay between these conditions, healthcare providers can develop tailored treatment plans that address the unique needs of each patient.
Symptoms and Diagnosis
Symptoms of ichthyosis primarily involve the skin, presenting as dry, scaly patches that may be mild or severe depending on the type of ichthyosis. Individuals may experience itching, redness, and thickened skin, which can impact their daily life and self-confidence. In some cases, ichthyosis can be associated with other health issues such as eye problems or joint stiffness.
On the other hand, male hypogonadism manifests with symptoms related to testosterone deficiency, including decreased libido, erectile dysfunction, fatigue, and mood changes. Adolescent males with hypogonadism may exhibit delayed puberty or incomplete sexual development. Long-term consequences can affect bone health and fertility.
Diagnosing ichthyosis involves a physical examination of the skin, family history assessment, and sometimes a skin biopsy to confirm the specific type of ichthyosis. For male hypogonadism, blood tests to measure testosterone levels, as well as imaging studies of the reproductive organs, are typically conducted to determine the cause and severity of hormone deficiency.
Given the complexity of these conditions, a multidisciplinary approach involving dermatologists, endocrinologists, and other specialists is often necessary to accurately diagnose and treat ichthyosis and male hypogonadism. Early detection and intervention can help improve outcomes and quality of life for individuals affected by these disorders.
Treatment Options
Managing ichthyosis involves a combination of skincare strategies aimed at hydrating the skin and reducing scaling. Basic measures include regular use of moisturizers, gentle exfoliation, and avoiding harsh soaps that can worsen dryness. In more severe cases, topical medications such as emollients, keratolytics, or prescription steroid creams may be prescribed.
For male hypogonadism, treatment options depend on the underlying cause and may include hormone replacement therapy to restore testosterone levels to normal. This can be administered through injections, patches, gels, or implants. Lifestyle modifications such as regular exercise, a balanced diet, and weight management can also support hormone production.
In cases where ichthyosis and male hypogonadism coexist, a comprehensive treatment approach is essential. Healthcare providers may need to coordinate care to address both the dermatological and endocrine aspects of the conditions. This can involve a tailored skincare regimen along with hormonal therapies to manage testosterone deficiency effectively.
Regular follow-up appointments with healthcare professionals are important for monitoring the progress of treatment and adjusting interventions as needed. Patients should communicate any changes in symptoms or concerns to their medical team to ensure optimal management of both ichthyosis and male hypogonadism.
Managing Hormone Levels
In individuals with male hypogonadism, managing hormone levels is crucial to address testosterone deficiency and promote overall well-being. Hormone replacement therapy (HRT) is a common treatment approach that aims to restore testosterone levels to normal ranges. This can help alleviate symptoms such as low libido, fatigue, and muscle weakness.
HRT can be administered through various methods, including injections, patches, gels, or implants. The choice of treatment depends on factors such as the underlying cause of hypogonadism, individual preferences, and lifestyle considerations. Close monitoring by healthcare providers is essential to ensure that hormone levels are effectively regulated.
When ichthyosis coexists with male hypogonadism, managing hormone levels becomes an integral part of a comprehensive treatment plan. Healthcare providers may need to collaborate to tailor therapies that address both the skin condition and testosterone deficiency. This coordinated approach can optimize outcomes for individuals facing these dual challenges.
Regular blood tests to monitor testosterone levels and evaluate the response to HRT are essential for adjusting treatment as needed. Adhering to prescribed medications and following a healthy lifestyle, including regular exercise and a balanced diet, can further support hormone balance and overall health in individuals with ichthyosis and male hypogonadism.