Disease ⏤ Female Pseudohermaphroditism
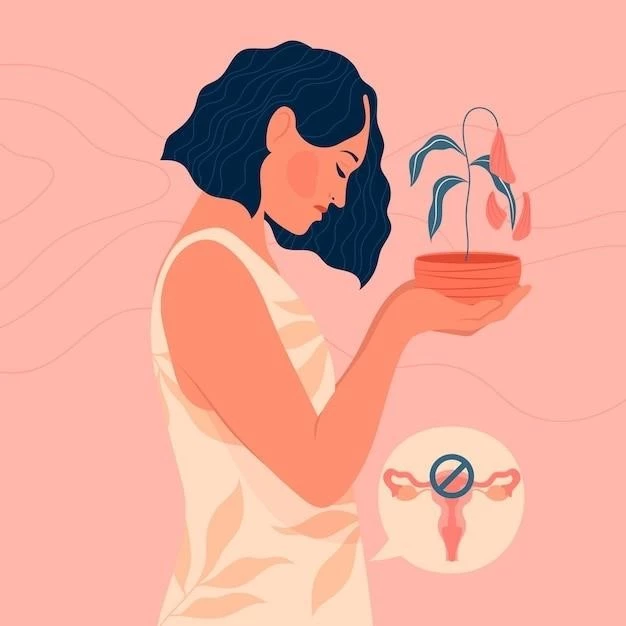
Female Pseudohermaphroditism is a complex condition related to Female Ambiguity and Androgenesis, affecting gender identity and sexual differentiation․ This article investigates the causes, symptoms, diagnosis, impact on the reproductive system, treatment options, and long-term outlook for individuals with this condition․
Introduction to Female Pseudohermaphroditism
Female Pseudohermaphroditism is a rare intersex condition characterized by the atypical development of the reproductive system and external genitalia․ It involves an ambiguity in the female genitalia, leading to challenges in identifying the individual as distinctly male or female․
Embryonic development plays a crucial role in sexual differentiation, where the presence or absence of certain hormones can result in variations in gender identity․ Hormonal imbalance, chromosomal abnormalities, and genetic mutations can contribute to the manifestation of Female Pseudohermaphroditism․
Individuals with this condition may experience masculinization of external genitalia due to elevated androgen levels․ Disorders such as Congenital Adrenal Hyperplasia or Gonadal Dysgenesis can impact hormone production, leading to the development of female ambiguity․
Diagnosis of Female Pseudohermaphroditism often involves a series of diagnostic tests to assess the genetic, hormonal, and anatomical aspects of the individual․ Understanding the factors contributing to this condition is vital for providing appropriate medical interventions and support for affected individuals․
Understanding Gender Identity and Sexual Differentiation
Gender identity development and sexual differentiation are intricate processes influenced by various factors, including genetic, hormonal, and environmental elements․ In the context of Female Pseudohermaphroditism, the typical trajectory of sexual development may be altered, leading to challenges in establishing a clear gender identity․
During embryonic development, the formation of the reproductive system and external genitalia is regulated by a complex interplay of hormones․ Any disruptions in this process can result in anomalies such as female ambiguity․ Understanding the mechanisms underlying sexual differentiation is essential for comprehending the complexities of Female Pseudohermaphroditism․
Hormonal imbalances, particularly in androgen levels, can play a significant role in the manifestation of female pseudohermaphroditism․ The exposure to atypical hormone levels during critical stages of development can influence the expression of primary and secondary sexual characteristics, leading to variations in gender presentation․
Furthermore, genetic variations and chromosomal abnormalities can impact the process of sexual differentiation, contributing to conditions like Female Pseudohermaphroditism․ The interplay between genetic predispositions and environmental factors underscores the importance of a multidisciplinary approach to understanding and addressing gender identity concerns in individuals affected by this condition․
Causes of Female Pseudohermaphroditism
Female Pseudohermaphroditism can have various underlying causes related to disruptions in the process of sexual differentiation during embryonic development․ Chromosomal abnormalities, such as variations in the number of sex chromosomes, can contribute to the manifestation of this condition․
Endocrinopathy, involving abnormalities in hormone production and signaling, can play a crucial role in the development of female pseudohermaphroditism․ Conditions like Congenital Adrenal Hyperplasia, where there is an excess production of androgens, can lead to virilization of external genitalia in individuals assigned female at birth․
Gonadal dysgenesis, characterized by incomplete or abnormal development of gonads, can also result in variations in sexual differentiation, potentially leading to female pseudohermaphroditism․ The interplay of genetic factors, hormonal influences, and environmental triggers can contribute to the complexity of this condition․
Androgenesis, a condition involving excessive masculinization, can also be a contributing factor to the development of female pseudohermaphroditism․ Understanding the diverse etiology of this condition is essential for accurate diagnosis, treatment planning, and providing appropriate support for individuals affected by Female Pseudohermaphroditism․
Types of Female Pseudohermaphroditism
Female Pseudohermaphroditism encompasses a spectrum of conditions that involve variations in the development of the reproductive system and external genitalia․ One type of this condition is characterized by the presence of female internal reproductive organs with ambiguous or masculinized external genitalia․
Another type of Female Pseudohermaphroditism may involve genetic variations or chromosomal abnormalities leading to atypical hormone production and sexual differentiation․ This can result in a mismatch between the genetic sex and the external appearance of the individual, causing challenges in gender identity development․
In some cases, Female Pseudohermaphroditism may be linked to specific endocrine disorders such as Congenital Adrenal Hyperplasia, where excess androgen production can influence the development of secondary sex characteristics․ Understanding the specific type of Female Pseudohermaphroditism is crucial for determining the appropriate diagnostic approach and treatment strategies tailored to the individual’s needs․
Each subtype of Female Pseudohermaphroditism presents its unique challenges and complexities, necessitating a comprehensive evaluation by healthcare providers specializing in intersex conditions․ By identifying the specific type of Female Pseudohermaphroditism, healthcare professionals can offer personalized care and support to individuals affected by this condition․
Symptoms and Diagnosis
Female Pseudohermaphroditism may present with a range of symptoms related to the atypical development of the reproductive system and external genitalia․ Symptoms can include ambiguity in the appearance of the genitalia, such as a combination of male and female characteristics, leading to challenges in assigning a clear gender identity․
Diagnosing Female Pseudohermaphroditism often involves a comprehensive evaluation by healthcare providers specializing in intersex conditions․ Diagnostic tests may include genetic testing to assess chromosomal abnormalities, hormone level measurements to evaluate endocrine function, and imaging studies to visualize internal reproductive structures․
Individuals with Female Pseudohermaphroditism may undergo a series of examinations to determine the extent of anatomical variations and hormonal imbalances contributing to their condition․ Psychological assessments and counseling may also be integral in understanding the impact of the diagnosis on the individual’s mental well-being and gender identity development․
Early detection and accurate diagnosis of Female Pseudohermaphroditism are essential for initiating timely interventions and providing appropriate support to individuals affected by this condition․ A multidisciplinary approach involving endocrinologists, geneticists, psychologists, and other healthcare professionals is often necessary to ensure comprehensive care for individuals with Female Pseudohermaphroditism․
Effects on Reproductive System and Hormone Production
Female Pseudohermaphroditism can have profound effects on the reproductive system and hormone production in affected individuals․ The atypical development of the reproductive organs can lead to challenges in fertility and reproductive function․ Internal structures such as the uterus, fallopian tubes, and ovaries may exhibit anomalies that impact reproductive health․
Abnormal hormone production, particularly involving androgens and estrogens, can further complicate the hormonal balance in individuals with Female Pseudohermaphroditism․ Hormonal imbalances may contribute to the development of secondary sexual characteristics that do not align with the individual’s genetic sex, leading to potential distress and identity issues․
The impact of Female Pseudohermaphroditism on hormone production can extend beyond physical characteristics to affect overall endocrine function and metabolic processes․ Hormonal dysregulation may influence growth patterns, bone health, and cardiovascular health, necessitating close monitoring and hormonal management by healthcare providers․
Understanding the effects of Female Pseudohermaphroditism on the reproductive system and hormone production is crucial for devising individualized treatment plans and addressing the specific needs of each person affected by this condition․ Long-term management may involve hormone replacement therapy, surgical interventions, and ongoing monitoring to optimize reproductive and overall health outcomes․
Treatment and Medical Intervention
Treatment and medical intervention for Female Pseudohermaphroditism focus on addressing the specific needs of individuals affected by this complex condition․ The approach to treatment is often tailored to the type and severity of the presentation, aiming to optimize physical health and psychological well-being․
Medical management of Female Pseudohermaphroditism may involve hormone therapy to regulate endocrine imbalances and promote the development of secondary sexual characteristics consistent with the individual’s identified gender․ Hormone replacement therapy can help address issues related to feminization or masculinization, improving quality of life․
Surgical interventions may be considered in cases where anatomical anomalies need correction to enhance function and alleviate physical discomfort․ Procedures such as genital reconstruction surgery or gonadectomy may be recommended to align external genitalia with the individual’s gender identity and improve overall genital health․
Psychological and emotional support is an integral component of the treatment plan for individuals with Female Pseudohermaphroditism․ Counseling, support groups, and therapy sessions can help individuals navigate the challenges of gender identity, self-acceptance, and social interactions in a supportive environment․
Collaboration between healthcare providers, including endocrinologists, surgeons, mental health professionals, and support services, is essential in ensuring comprehensive care for individuals with Female Pseudohermaphroditism․ A multidisciplinary approach enables a holistic treatment strategy that acknowledges the diverse needs of patients and promotes their overall well-being․
Puberty and Long-Term Outlook
Puberty is a critical stage in the life of individuals with Female Pseudohermaphroditism, marked by significant physical and hormonal changes․ During puberty, the effects of hormonal imbalances and variations in sexual development may become more pronounced, impacting the individual’s experience of this developmental milestone․
Healthcare providers play a crucial role in supporting individuals with Female Pseudohermaphroditism during puberty, providing guidance on managing hormonal transitions and addressing any concerns related to gender identity and body image․ Monitoring hormone levels and physical changes is essential to ensure optimal health outcomes․
The long-term outlook for individuals with Female Pseudohermaphroditism depends on various factors, including the type and severity of the condition, the effectiveness of medical interventions, and the individual’s psychological adaptation to their unique circumstances․ Regular follow-up care and monitoring are essential to assess physical development, hormonal balance, and overall well-being․
Psychosocial support and access to mental health services are vital components of long-term care for individuals with Female Pseudohermaphroditism․ Ongoing psychological support can help individuals navigate the complexities of gender identity, self-acceptance, and societal acceptance, promoting resilience and well-being․

By addressing the challenges associated with Female Pseudohermaphroditism comprehensively throughout puberty and beyond, healthcare providers strive to empower individuals to lead fulfilling lives and navigate the complexities of their condition with resilience and dignity․