Article Plan⁚ Disease ― Papillitis of the Optic Nerve
Introduction to Papillitis. Optic nerve involvement with visual impairment can present in various forms, including papillitis and retrobulbar optic neuritis. Understanding these conditions is crucial for proper diagnosis and treatment.
Introduction to Papillitis
Papillitis, a specific type of optic neuritis, involves inflammation and deterioration of the optic nerve head known as the optic disk. Optic papillitis is often associated with substantial losses in visual fields and pain. Understanding the presentation and impact of papillitis is crucial for early diagnosis and effective management to preserve visual function.
Understanding Optic Neuritis
Optic neuropathy refers to dysfunction of the optic nerve, resulting in variable loss of visual acuity, visual field changes, and more. Optic neuritis, an inflammatory or demyelinating form of optic neuropathy, involves inflammation of one or both optic nerves, commonly associated with multiple sclerosis or idiopathic causes. Recognizing typical and atypical optic neuritis presentations, understanding the differential diagnoses, and the importance of prompt diagnosis and treatment are essential for preserving vision and avoiding long-term visual consequences.
Clinical Presentation of Papillitis
Papillitis, a subtype of optic neuritis, presents with inflammation and degeneration of the optic nerve head, specifically the optic disk. Common symptoms include visual field loss, pain in the affected eye, and impaired color vision. Recognizing these clinical manifestations promptly can aid in early diagnosis and initiation of appropriate treatment to prevent further visual deterioration.
Causes of Optic Nerve Papillitis
Optic papillitis can have various origins, including idiopathic factors, infectious agents, ischemic conditions like acute ischemic optic neuropathy, or even attributable to specific tumors affecting the optic nerve. Additionally, conditions like diabetes can lead to diabetic papillopathy, a rare manifestation related to the disease. Familiarity with the diverse causes of optic nerve papillitis is crucial for proper diagnosis and tailored treatment plans to address the underlying condition effectively.
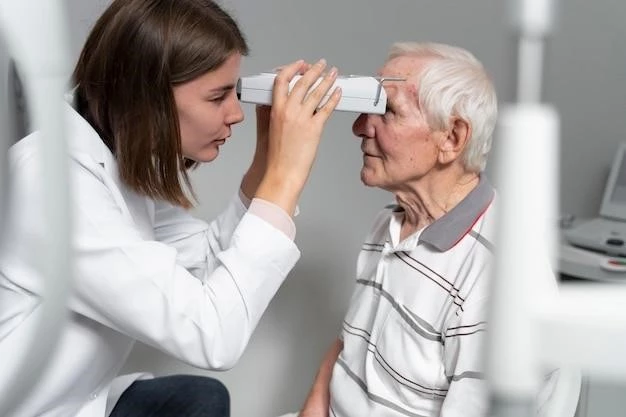
Diagnostic Tools for Papillitis
Diagnosing papillitis requires a combination of clinical evaluation and specific diagnostic tools to confirm the condition accurately. Various tools may include ophthalmoscopy to assess the optic nerve head appearance, visual field testing to detect visual impairments, and color vision assessments to identify any deficits. Additionally, imaging techniques such as optical coherence tomography (OCT) play a critical role in evaluating the structural integrity of the optic nerve and monitoring changes over time. Collaborating with an ophthalmologist for a comprehensive eye examination, including these diagnostic tools, is essential for an accurate diagnosis and tailored treatment plan for papillitis.
Differential Diagnosis of Papillitis
When evaluating a patient with papillitis, it is crucial to consider a differential diagnosis that includes various conditions affecting the optic nerve. These conditions may range from infectious causes to inflammatory disorders like anterior ischemic optic neuropathy or tumors affecting the optic nerve. Distinguishing papillitis from other etiologies is essential for appropriate management and treatment decisions to address the specific underlying cause effectively. Consulting with an eye care specialist for a comprehensive evaluation and differential diagnosis is important for optimal care.
Management and Treatment Options for Papillitis
Effective management of papillitis involves a multidisciplinary approach and individualized treatment plans tailored to the underlying cause. Treatment may include anti-inflammatory medications to reduce optic nerve inflammation, intravenous corticosteroids to speed up recovery, and immunosuppressive therapy in cases of autoimmune-related papillitis. Close monitoring of visual symptoms and regular follow-ups with an ophthalmologist are essential to track progress and adjust treatment as needed. Surgical interventions may be necessary in cases involving compressive lesions or tumors affecting the optic nerve. Seeking prompt medical attention and adhering to the prescribed treatment regimen are crucial for optimizing visual outcomes and overall management of papillitis.
Prognosis and Visual Recovery in Papillitis
Understanding the prognosis and potential visual recovery in papillitis is crucial for both patients and healthcare providers. While the outcomes may vary depending on the underlying cause and severity of the condition, prompt diagnosis and appropriate treatment offer the best chance for positive results. Monitoring visual symptoms, adhering to the prescribed treatment plan, and regular follow-ups with healthcare professionals can significantly impact visual recovery in individuals with papillitis. It is essential to stay informed about the prognosis to set realistic expectations and actively participate in the management of the condition for optimal visual outcomes.
Relationship Between Papillitis and Multiple Sclerosis
Optic neuritis, including papillitis, can often be an early sign of multiple sclerosis (MS), a condition characterized by inflammation and damage to nerves in the brain and spinal cord. The association between papillitis and MS is significant, with optic nerve inflammation being a common occurrence in individuals with MS. Recognizing this relationship is crucial as prompt management of optic neuritis can help in the early detection and management of multiple sclerosis. As optic neuritis and MS may have overlapping symptoms, a thorough evaluation by a healthcare provider is essential to determine the appropriate course of action and treatment plan.
Importance of Optic Coherence Tomography (OCT) in Papillitis
Optic coherence tomography (OCT) plays a significant role in the assessment of papillitis by enabling non-invasive imaging and measurement of the peripapillary retinal nerve fiber layer. This tool facilitates the evaluation of structural changes in the optic nerve and can help monitor the progression of papillitis over time. By measuring the thickness of the peripapillary retinal nerve fiber layer, OCT provides valuable insights into the status of the optic nerve in papillitis, aiding in the diagnosis, management, and follow-up of the condition. Collaborating with healthcare professionals experienced in utilizing OCT can enhance the precision of assessment and contribute to better treatment outcomes for individuals with papillitis.
Recognizing Atypical Optic Neuritis
Atypical optic neuritis presents a challenging diagnosis as it may be caused by various underlying conditions such as neuromyelitis optica, autoimmune optic neuropathy, or systemic diseases. Distinguishing atypical optic neuritis from typical forms is crucial for initiating appropriate treatment strategies and preserving vision. Early recognition and targeted management are essential in addressing the specific etiologies associated with atypical optic neuritis, ensuring optimal visual outcomes for affected individuals. Collaboration with healthcare professionals experienced in diagnosing and managing atypical optic neuritis is recommended for comprehensive care.
Demographics and Incidence of Optic Neuritis
Optic neuritis is a condition that can affect a wide demographic range, with typical cases commonly seen in young white women aged 20-40 years and having a female preponderance. However, atypical optic neuritis can impact individuals of various ages and genders, deviating from the typical demographic profile. Incidence rates of optic neuritis have been estimated at 5 per 100,000 individuals annually in the United States. Prompt evaluation with a comprehensive eye examination, including automated perimetry, is crucial for accurate diagnosis and management based on the patient’s specific characteristics and clinical presentation.
Imaging Techniques for Optic Neuritis Diagnosis
Imaging techniques play a crucial role in diagnosing optic neuritis, including papillitis. Optic coherence tomography (OCT) is a non-invasive imaging tool used to measure the thickness of the peripapillary retinal nerve fiber layer, providing essential information for evaluating structural changes in the optic nerve. Optical coherence tomography can aid in monitoring the progression of optic neuritis over time and guide treatment decisions based on the extent of nerve fiber layer thickness. Collaborating with healthcare providers experienced in interpreting OCT results can enhance the accuracy of diagnosis and treatment planning for individuals with optic neuritis.
Role of MRI and OCT in Differentiating Optic Neuritis Etiologies
Magnetic Resonance Imaging (MRI) and Optical Coherence Tomography (OCT) are instrumental in distinguishing between various etiologies of optic neuritis. MRI offers detailed imaging of the brain and optic nerves, aiding in the identification of demyelinating lesions characteristic of conditions like multiple sclerosis. Contrast-enhanced MRI can reveal optic nerve enhancement patterns specific to different types of optic neuropathies, helping differentiate between demyelinating and non-demyelinating causes. On the other hand, OCT provides precise measurements of the peripapillary retinal nerve fiber layer thickness, offering insights into structural changes in the optic nerve that can assist in diagnosing and monitoring optic neuritis comprehensively. Collaboration with healthcare providers skilled in interpreting MRI and OCT results is essential for accurate etiology differentiation and optimal management of optic neuritis.