Understanding Diverticulosis
Diverticulosis is a common condition affecting the colon and intestine. This article will delve into the causes of inflammation, symptoms, impact on digestive health, fiber in the diet, managing constipation, bloating, medical treatments, complications, surgical options, infection prevention, and long-term diet management.
I. Introduction to Diverticulosis
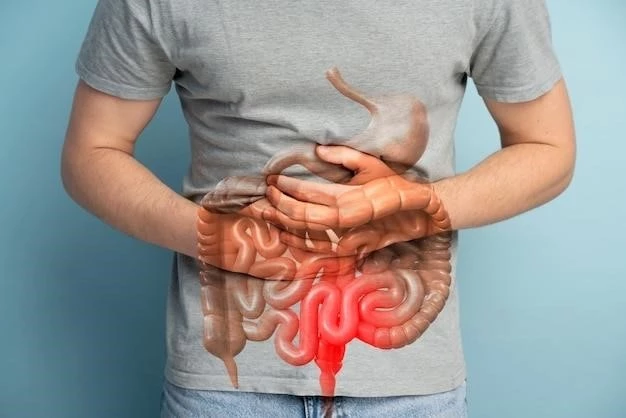
Diverticulosis is a common condition characterized by the presence of small, bulging pouches called diverticula in the lining of the colon or large intestine. These pouches can develop over time, particularly in areas where the colon is weakest. While diverticulosis itself is usually harmless, it can lead to complications such as diverticulitis if the pouches become inflamed or infected.
As individuals age, the likelihood of developing diverticulosis increases. Factors such as a low-fiber diet, obesity, lack of exercise, and smoking may contribute to its development. While not always symptomatic, diverticulosis can cause discomfort and often goes unnoticed until complications arise.
Understanding diverticulosis begins with knowledge of the digestive system and how these pouches can impact its function. By recognizing the risk factors and potential consequences of this condition, individuals can take proactive steps to manage their digestive health and prevent the progression to diverticulitis and other more serious complications.
II. The Colon and Intestine
The colon, also known as the large intestine, plays a crucial role in the digestive process. It is responsible for absorbing water and electrolytes from the indigestible food matter that passes through it. The colon is divided into several sections, including the ascending, transverse, descending, and sigmoid colon, each with specific functions.
Adjacent to the colon is the small intestine, where most of the digestion and nutrient absorption occurs. The small intestine is composed of the duodenum, jejunum, and ileum. Once digested food particles reach the large intestine, any remaining water is absorbed, and waste material is formed into stool for elimination.
In diverticulosis, the presence of diverticula ⸺ small, bulging pouches that develop in weak spots of the colon or intestine ⸺ can disrupt the normal digestive process. While diverticulosis itself may not cause issues, inflammation or infection of these pouches, known as diverticulitis, can lead to symptoms such as abdominal pain, constipation, diarrhea, bloating, and cramps.
III. Causes of Inflammation
The primary cause of inflammation in diverticulosis is the trapping of fecal material within the diverticula, leading to bacterial overgrowth and irritation of the intestinal wall. When the diverticula become inflamed or infected, the condition progresses to diverticulitis. Risk factors for diverticulitis include a low-fiber diet, which can result in harder stools that are more challenging to pass.
Inflammation can also be triggered by fecal matter getting trapped in the diverticula, causing an immune reaction. As the immune system responds to the bacterial presence, inflammation occurs, resulting in symptoms such as abdominal pain, fever, and changes in bowel habits. In severe cases, complications like abscess formation or perforation of the intestine can occur, necessitating immediate medical attention.
Other factors contributing to the development of diverticulitis include obesity, lack of physical activity, smoking, and genetic predisposition. Maintaining a diet rich in fiber, staying hydrated, exercising regularly, and avoiding tobacco use are essential preventive measures to reduce the risk of inflammation and complications associated with diverticulosis.
IV. Symptoms of Diverticulosis
Diverticulosis, in its initial stages, is often asymptomatic. Many individuals may have diverticula in their colon or intestine without experiencing any noticeable signs. However, as the condition progresses or if complications arise, various symptoms may manifest. Common symptoms of diverticulosis include⁚
- Abdominal pain, usually in the lower left side, that can be persistent or intermittent
- Changes in bowel habits, such as constipation or diarrhea
- Bloating or excessive gas
- Cramping or tenderness in the abdominal region
- Occasional rectal bleeding, typically bright red in color
If diverticula become inflamed or infected, these symptoms may worsen and be accompanied by fever, nausea, vomiting, and more intense abdominal pain. It is essential to monitor any changes in symptoms and seek medical evaluation if concerned about the possibility of diverticulitis or other complications related to diverticulosis.
V. Common Symptoms
Diverticulosis can present with a variety of symptoms, ranging from mild discomfort to more severe complications. The most common symptoms experienced by individuals with diverticulosis include⁚
- Abdominal pain or tenderness, especially in the lower left side
- Changes in bowel habits, such as constipation or diarrhea
- Bloating and increased gas production
- Cramping or spasms in the abdominal area
- Occasional rectal bleeding, typically bright red in color
While some individuals may have diverticulosis without any symptoms, these manifestations can become more pronounced if the diverticula become inflamed or infected, leading to diverticulitis. Monitoring changes in symptoms and seeking medical advice if any concerning signs occur is crucial in managing diverticulosis and preventing complications.
VI. Impact on Digestive Health
Diverticulosis can have a significant impact on digestive health, particularly when complications such as diverticulitis arise. The presence of diverticula in the colon or intestine can lead to disturbances in normal bowel function and may cause discomfort and pain. When the diverticula become inflamed, symptoms can worsen and affect the overall digestive process.
Individuals with diverticulosis may experience changes in bowel habits, including constipation or diarrhea, which can disrupt regular digestion. Bloating and increased gas production are common issues associated with diverticulosis, contributing to abdominal discomfort. Cramping and spasms in the abdominal region can also occur, further impacting digestive well-being.
It is essential to understand how diverticulosis can influence digestive health to effectively manage the condition and reduce the risk of complications. By maintaining a high-fiber diet, staying hydrated, and adopting a healthy lifestyle, individuals can support their digestive system and minimize the impact of diverticular disease on overall gastrointestinal function.
VII. Diagnosis and Treatment Options
Diagnosing diverticulosis often involves a combination of medical history review, physical examination, and diagnostic tests. Imaging studies such as a colonoscopy or a CT scan may be used to confirm the presence of diverticula in the colon or intestine. Additionally, blood tests can help assess inflammation levels and rule out other conditions.
For individuals with mild diverticulosis and no significant symptoms, treatment may focus on lifestyle modifications to prevent complications. Increasing dietary fiber intake, staying hydrated, and exercising regularly can help promote healthy digestion and reduce the risk of diverticulitis. Over-the-counter pain medications may be used to manage discomfort.
In cases where diverticulosis progresses to diverticulitis or presents with severe symptoms, medical treatment is necessary. Antibiotics are often prescribed to treat infection and inflammation. In more severe or recurrent cases, hospitalization and intravenous antibiotics may be required. Pain management and symptom relief are essential components of diverticulitis treatment.
Surgical interventions may be considered for individuals with recurrent diverticulitis, complications such as abscesses or perforations, or other severe issues. Surgery may involve removing the affected portion of the colon or intestine to prevent further inflammation and reduce the risk of future complications. The decision to pursue surgery is made based on individual circumstances and the recommendations of healthcare providers.
VIII. Importance of Fiber in the Diet
Dietary fiber plays a crucial role in the management of diverticulosis and the prevention of complications such as diverticulitis. Adequate fiber intake helps maintain healthy digestion by promoting regular bowel movements and preventing constipation, a common risk factor for diverticular inflammation.
Fiber, found in fruits, vegetables, whole grains, legumes, and nuts, adds bulk to the stool, making it easier to pass through the intestines. This can help prevent fecal matter from becoming trapped in diverticula, reducing the risk of bacterial overgrowth and inflammation. Soluble fiber, in particular, can be beneficial in softening stools and easing bowel movements.
Individuals with diverticulosis are often advised to increase their fiber consumption gradually to avoid bloating or gas. The recommended daily fiber intake for adults is around 25 to 30 grams, but this may vary depending on individual dietary needs. Fiber supplements or fiber-rich foods can be incorporated into meals to reach these goals.
By prioritizing a high-fiber diet, individuals with diverticulosis can promote intestinal health, regulate bowel function, and potentially prevent the progression to diverticulitis. Alongside hydration and other lifestyle adjustments, fiber intake is a cornerstone of managing diverticular disease and supporting overall gastrointestinal wellness.
IX. Managing Constipation and Diarrhea
For individuals with diverticulosis, managing constipation and diarrhea is essential to promote regular bowel function and prevent complications. Constipation, characterized by infrequent or difficult bowel movements, can contribute to diverticular inflammation by increasing pressure in the colon. Diarrhea, on the other hand, can exacerbate symptoms and disrupt intestinal balance.
To manage constipation, increasing dietary fiber intake is key. Fiber-rich foods like fruits, vegetables, whole grains, and legumes can soften stools and facilitate bowel movements. Adequate hydration is also crucial to maintain stool consistency and support digestion. Regular physical activity can help stimulate bowel motility and alleviate constipation.
On the other hand, managing diarrhea involves identifying and addressing potential triggers. Monitoring food choices and avoiding known irritants can help regulate stool consistency. Probiotics and a balanced diet that includes soluble fibers may aid in restoring gut health and reducing diarrhea episodes. In some cases, medication or dietary modifications may be necessary.
Individuals with diverticulosis should work closely with healthcare providers to develop personalized strategies for managing constipation and diarrhea. Lifestyle adjustments, dietary changes, and medical interventions, if needed, can play a significant role in promoting digestive comfort and reducing the risk of complications associated with diverticular disease.
X. Dealing with Bloating and Cramps
Bloating and cramps are common symptoms that individuals with diverticulosis may experience. Bloating, which involves feeling full or swollen in the abdomen, can result from gas accumulation in the digestive system. Cramps, characterized by sharp pains or spasms in the abdominal region, can be discomforting and disruptive to daily activities.
To manage bloating associated with diverticulosis, individuals can adopt several strategies. Avoiding gas-producing foods like beans, cabbage, and carbonated drinks can help reduce bloating. Eating smaller, more frequent meals and chewing food thoroughly can aid digestion and minimize the sensation of fullness. Physical activity, such as walking or gentle yoga, may alleviate bloating by stimulating bowel movement.
Coping with cramps involves similar approaches. Maintaining a balanced diet rich in fiber and low in irritants can prevent cramping episodes. Warm compresses or gentle abdominal massages may provide relief from cramps. Stress management techniques like deep breathing exercises or meditation can help reduce muscle tension and alleviate abdominal discomfort.
Individuals with diverticulosis should consult healthcare providers if bloating and cramps persist or worsen, as these symptoms can sometimes indicate underlying issues. By addressing bloating and cramps proactively and implementing lifestyle modifications, individuals can enhance their comfort and quality of life while managing diverticular disease.
XI. Medical Treatment for Diverticulosis
Medical treatment for diverticulosis aims to manage symptoms, prevent complications, and improve overall digestive health. In cases where diverticulosis is asymptomatic or mild, lifestyle modifications are often the first line of therapy. This includes increasing dietary fiber intake, maintaining hydration, and engaging in regular physical activity to support healthy bowel function.
If diverticulitis occurs or if symptoms are severe, medical interventions may be necessary. Antibiotics are commonly prescribed to treat bacterial infections and reduce inflammation in the diverticula. Pain medications can help manage discomfort, while antispasmodic drugs may be used to alleviate cramping. Rest and dietary adjustments are typically recommended during acute episodes of diverticulitis.
In some instances, hospitalization may be required for individuals with severe diverticulitis or complications such as abscesses or perforations. Intravenous antibiotics and close monitoring by healthcare providers may be necessary to ensure effective treatment and prevent further issues. In rare cases of complications, surgery may be considered to remove affected portions of the colon or intestine.
Medical treatment for diverticulosis is individualized based on the severity of symptoms, the presence of complications, and the patient’s overall health status. Regular follow-up appointments with healthcare providers are essential to monitor the condition, adjust treatment as needed, and promote optimal digestive wellness in individuals with diverticular disease.
XII. Potential Complications
Diverticulosis can lead to various complications, with diverticulitis being the most common and significant. In diverticulitis, the diverticula become inflamed or infected, causing symptoms such as severe abdominal pain, fever, nausea, and changes in bowel habits. Left untreated, diverticulitis can progress to more severe complications.
Complications of diverticulitis may include the formation of abscesses, which are localized collections of pus that require drainage and antibiotic therapy. In some cases, perforations of the intestinal wall can occur, leading to peritonitis, a severe infection of the abdominal cavity requiring immediate medical intervention. Fistulas, abnormal connections between organs, may also develop in rare instances.
In addition to these acute complications, chronic issues like strictures or bowel obstructions can arise from recurrent episodes of diverticulitis. Strictures are narrowings of the intestinal passage, while obstructions prevent the normal flow of stool. These complications may necessitate surgical interventions to restore proper bowel function and alleviate symptoms.
It is crucial for individuals with diverticulosis to be aware of these potential complications and seek prompt medical attention if symptoms worsen or new signs develop. Early diagnosis and appropriate management can help prevent complications from diverticular disease and improve outcomes for individuals at risk of severe diverticulitis-related issues.
XIII. Surgical Interventions
Surgical interventions may be necessary for individuals with diverticulosis who experience recurrent diverticulitis, complications that do not respond to medical treatment, or severe symptoms impacting quality of life. Surgery aims to remove the affected portion of the colon or intestine, known as a colectomy, to prevent further inflammation and reduce the risk of complications.
One common surgical procedure for diverticulosis is a laparoscopic sigmoid colectomy, where the portion of the sigmoid colon containing diverticula is removed. This minimally invasive approach involves small incisions and the use of specialized tools to access and remove the affected tissue. Open colectomy may be required for more complex cases or if laparoscopic surgery is not feasible.
In some instances, a temporary colostomy may be created as part of the surgical treatment. A colostomy involves diverting stool through an opening in the abdominal wall to allow the affected portion of the colon to heal. This temporary measure may be reversed in a second surgical procedure once the inflammation has resolved.
Surgical interventions for diverticulosis are typically considered after conservative treatments have been attempted without adequate results. The decision to proceed with surgery is made collaboratively between the individual and the healthcare team based on the severity of symptoms, risk of complications, and overall health status. Post-operative care and monitoring are essential for optimal recovery and long-term management.
XIV. Preventing Infection
Preventing infection is a key aspect of managing diverticulosis and reducing the risk of complications like diverticulitis. Individuals with diverticulosis can take several measures to help prevent infections in the diverticular pouches, which can lead to inflammation and more severe issues.
One essential strategy for preventing infection is maintaining a high-fiber diet. Fiber helps regulate bowel movements and prevents constipation, reducing the likelihood of fecal matter becoming trapped in the diverticula and leading to bacterial overgrowth. Adequate hydration is also crucial for softening stools and promoting regular bowel function.
Another preventive measure is avoiding known irritants that can exacerbate diverticular inflammation. This includes limiting the intake of processed foods, red meat, and foods high in saturated fats. Smoking cessation and moderation of alcohol consumption can also support overall gastrointestinal health and reduce the risk of infection in diverticular pouches.
Engaging in regular physical activity can aid in promoting healthy digestion and preventing complications associated with diverticulosis. Exercise helps maintain bowel regularity, supports immune function, and contributes to overall well-being. Stress management techniques such as yoga, meditation, or deep breathing exercises may also help reduce inflammation and support digestive health.
XV. Long-Term Diet Management
Long-term diet management plays a crucial role in the overall management of diverticulosis and prevention of complications. Individuals with diverticulosis can benefit from adopting dietary habits that support digestive health, reduce symptoms, and decrease the risk of diverticular inflammation.
A cornerstone of long-term diet management for diverticulosis is maintaining adequate fiber intake. High-fiber foods like fruits, vegetables, whole grains, and legumes can help soften stools, promote regular bowel movements, and prevent constipation. Gradually increasing fiber consumption and staying hydrated are key factors in achieving optimal digestive wellness.
Alongside fiber, individuals with diverticulosis should focus on maintaining a balanced diet rich in nutrients and low in processed and high-fat foods. Consuming lean proteins, healthy fats, and a variety of vitamins and minerals can support overall health and reduce the risk of aggravating diverticular symptoms. Portion control and mindful eating can also aid in digestion.
Some individuals may benefit from keeping a food diary to track how different foods affect their digestive symptoms. By identifying trigger foods that worsen bloating, cramps, or other discomfort, individuals can customize their diet to suit their needs and minimize diverticulosis-related issues. Working with a healthcare provider or dietitian can provide guidance on developing a personalized long-term dietary plan.
XVI. Conclusion⁚ Living with Diverticulosis
Living with diverticulosis necessitates a proactive approach to managing digestive health and reducing the risk of complications. By adopting lifestyle modifications such as a high-fiber diet, adequate hydration, regular exercise, and stress management techniques, individuals with diverticulosis can support their well-being and improve quality of life.
It is crucial for individuals with diverticulosis to be aware of potential symptoms, contribute to preventing infection, and seek timely medical attention if concerns arise. Long-term dietary management, focusing on fiber-rich foods and nutrient-dense choices, plays a fundamental role in mitigating symptoms and promoting gastrointestinal function.
Regular follow-up with healthcare providers is essential for monitoring the condition, adjusting treatment as needed, and addressing any changes in symptoms. By working collaboratively with a healthcare team, individuals can develop personalized strategies to manage diverticulosis effectively and lead a fulfilling lifestyle while minimizing the impact of this gastrointestinal condition.
