Introduction
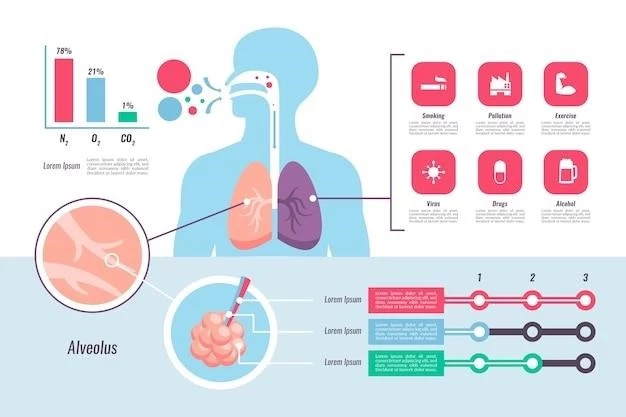
Pulmonary alveolar proteinosis (PAP) is a rare lung disease characterized by surfactant accumulation in the alveoli, leading to impaired gas exchange.
Pulmonary alveolar proteinosis (PAP) is a rare lung disease characterized by the abnormal accumulation of surfactant within the alveoli. In the congenital form, this condition may present from birth or at various ages due to genetic mutations affecting surfactant metabolism. The build-up of lipoproteinaceous material in the alveoli impairs gas exchange, leading to symptoms like dyspnea and hypoxemia. Understanding the role of genetic mutations in surfactant metabolism is crucial in managing congenital PAP.
Epidemiology
Pulmonary alveolar proteinosis is rare and typically presents in young to middle-aged adults, with a higher prevalence in smokers and a male predilection. Onset before age 1 may be associated with certain conditions.
Pulmonary alveolar proteinosis commonly affects young to middle-aged adults, with a higher prevalence in smokers, showing a male predilection in smoking-related cases. The disease may also occur in infants and children, with various presentations across different age groups.
Age and Gender Distribution
Pulmonary alveolar proteinosis usually presents in young and middle-aged adults, with a male predilection in smoking-related cases. The disease can also occur in children with variable clinical courses.
Symptoms and Signs
Clinical manifestations of congenital pulmonary alveolar proteinosis include respiratory distress, cough, and failure to thrive, with chest X-rays revealing diffuse symmetric airspace opacities. Additionally, affected infants may present with cyanosis, digital clubbing, and crackles on auscultation due to impaired gas exchange and abnormal surfactant accumulation.
Diagnosis
The diagnosis of congenital pulmonary alveolar proteinosis involves clinical evaluation, imaging studies like chest X-rays, and confirmatory tests such as bronchoalveolar lavage to identify characteristic surfactant accumulation.
Diagnostic Methods
Diagnosis of congenital pulmonary alveolar proteinosis involves a comprehensive approach including clinical evaluation, imaging studies like chest X-rays, and confirmatory tests such as bronchoalveolar lavage. Identification of characteristic surfactant accumulation in alveoli is crucial for confirming the diagnosis of this rare lung disease.
Therapeutic approaches for congenital pulmonary alveolar proteinosis include lung lavage, which helps remove the accumulated surfactant material and improve gas exchange for better respiratory function.
Management
Therapeutic approaches for congenital pulmonary alveolar proteinosis include lung lavage to remove accumulated surfactant material, enhancing respiratory function and alleviating symptoms to improve the overall quality of life for affected individuals.
Prognosis
Outcomes and long-term effects of congenital pulmonary alveolar proteinosis vary, with favorable prognosis seen in individuals undergoing effective treatment modalities aimed at surfactant removal from the alveoli.
Outcome and Long-term Effects
The outcome and long-term effects of congenital pulmonary alveolar proteinosis can vary, with proper treatment modalities targeting surfactant accumulation playing a crucial role in improving the prognosis and quality of life for patients affected by this rare lung condition.
Genetic mutations affecting surfactant metabolism or critical receptors like GM-CSF may lead to congenital pulmonary alveolar proteinosis, impacting lung function and respiratory health.
Role of Genetic Mutations
Congenital pulmonary alveolar proteinosis can result from mutations impacting surfactant proteins or GM-CSF receptor genes, leading to the abnormal accumulation of surfactant in the alveoli and affecting lung function.
Genetics
Certain genetic mutations affecting surfactant proteins or GM-CSF receptor genes may play a crucial role in the development of congenital pulmonary alveolar proteinosis.
Mechanism of Surfactant Accumulation
In congenital pulmonary alveolar proteinosis, the mechanism involves impaired surfactant clearance due to genetic mutations in surfactant proteins or GM-CSF receptor genes, leading to the abnormal accumulation of surfactant-rich material within the alveoli and impacting lung function.
Pathophysiology
Congenital Pulmonary Alveolar Proteinosis results from mutations affecting surfactant proteins or GM-CSF receptor genes, leading to abnormal surfactant accumulation impacting lung function.
Classification of Pulmonary Alveolar Proteinosis
Pulmonary alveolar proteinosis can be classified into primary (autoimmune and hereditary), secondary, congenital, and unclassifiable types based on underlying pathogenesis, highlighting the diverse etiologies contributing to this rare lung disorder.
Research
Recent advances in research have provided significant insights into the molecular mechanisms underlying congenital and acquired forms of pulmonary alveolar proteinosis.
Advancements in Understanding the Disease
Significant advancements in research have shed light on the molecular mechanisms underlying both congenital and acquired forms of pulmonary alveolar proteinosis, offering valuable insights into the pathogenesis and potential targeted treatment strategies for this rare lung disorder.
Animal Models
Animal models have played a crucial role in unravelling the underlying mechanisms of pulmonary alveolar proteinosis, aiding in the discovery of novel insights into the pathogenesis of this challenging lung disorder.
Animal models have significantly contributed to the understanding of pulmonary alveolar proteinosis, offering valuable insights into the pathophysiology and potential therapeutic targets for both congenital and acquired forms of the disease.
Disease Progression
Understanding the disease progression of congenital pulmonary alveolar proteinosis is crucial due to its variable clinical course, impacting respiratory health and treatment approaches.
Variable Clinical Course
Congenital pulmonary alveolar proteinosis manifests with variable clinical courses, impacting respiratory health differently among individuals and requiring tailored treatment approaches.
Therapeutic Options
Current treatment modalities for congenital pulmonary alveolar proteinosis include lung lavage and supportive care, with potential lung transplantation in severe cases.
Significance of Animal Studies
Animal models have significantly contributed to the understanding of pulmonary alveolar proteinosis, offering valuable insights into the pathophysiology and potential therapeutic targets for both congenital and acquired forms of the disease.
Complications
Pulmonary alveolar proteinosis, congenital, may lead to respiratory failure, compromised lung function, and a predisposition to lung infections due to the interference with gas exchange caused by surfactant accumulation in the alveoli.
Potential Risks and Associated Conditions
Complications of congenital pulmonary alveolar proteinosis include respiratory failure, compromised lung function, and an increased susceptibility to lung infections due to the accumulation of surfactant-rich material in the alveoli affecting gas exchange. These risks emphasize the importance of timely diagnosis and appropriate management strategies to mitigate long-term effects.