Pulmonary alveolar proteinosis (PAP) is a rare disease involving the accumulation of surfactant in the alveoli due to various causes like genetic mutations, auto-immune reactions, or toxic inhalation. Diagnosis requires bronchoalveolar lavage and CT scans, with treatments including lung lavage and anti-GM-CSF antibodies.
Definition and Causes
Pulmonary Alveolar Proteinosis (PAP) is a rare lung disorder characterized by the abnormal accumulation of surfactant in the alveoli and alveolar macrophages due to disrupted surfactant clearance mechanisms. The causes of PAP can include genetic mutations, autoimmune reactions targeting GM-CSF antibodies, toxic inhalation, and certain hematological disorders. It is essential to diagnose PAP accurately through bronchoalveolar lavage and high-resolution CT scans, allowing for tailored treatment strategies.
Symptoms and Diagnosis
No information is provided regarding symptoms and diagnosis. For detailed guidance on symptoms and diagnosis of pulmonary alveolar proteinosis, please consult reliable medical sources or healthcare professionals.
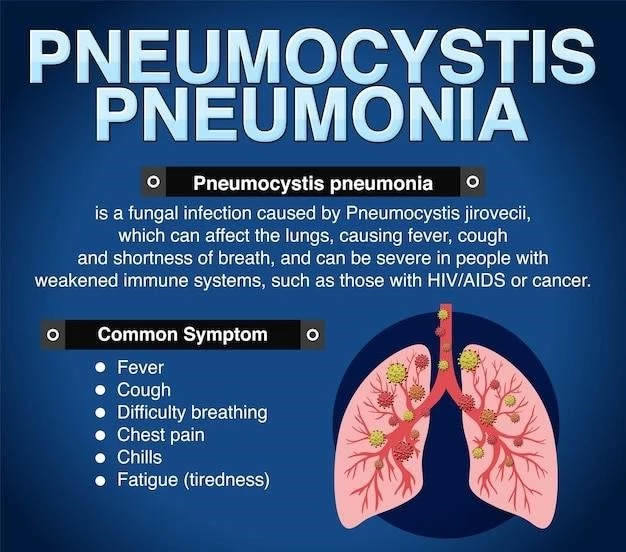
Common Symptoms
Some common symptoms of pulmonary alveolar proteinosis (PAP) include dyspnea, cough, fatigue, fever, cyanosis, and weight loss. It is essential to consult a healthcare professional for an accurate diagnosis if you experience these symptoms.
Diagnostic Methods
Diagnosing pulmonary alveolar proteinosis (PAP) typically involves bronchoalveolar lavage (BAL) to analyze the accumulation of lipoproteinaceous material in the alveoli. High-resolution CT scans are also utilized to visualize characteristic findings. Consult a healthcare provider for proper evaluation and diagnosis if you suspect PAP based on symptoms.
Treatment Options
For detailed guidance on treatment options for pulmonary alveolar proteinosis (PAP), consult healthcare professionals or reliable medical sources. Treatments may include whole lung lavage and anti-GM-CSF antibodies based on individual cases.
Whole Lung Lavage
Whole lung lavage is a crucial treatment option for pulmonary alveolar proteinosis (PAP) that involves the flushing of one lung at a time with a saline solution while the other lung is ventilated. This procedure helps remove the accumulated surfactant from the alveoli and can improve respiratory function. It is essential to consult healthcare professionals for guidance on the appropriateness and risks associated with whole lung lavage for treating PAP.
Anti-GM-CSF Antibodies
Anti-GM-CSF antibodies play a significant role in the pathogenesis of pulmonary alveolar proteinosis (PAP) by disrupting the normal clearance of surfactant in the alveoli. In certain cases, treatment options may involve targeting these antibodies to restore proper surfactant metabolism. It is crucial to consult healthcare professionals for personalized advice regarding the use of anti-GM-CSF antibodies in managing PAP.
Types of PAP
To explore the different types of pulmonary alveolar proteinosis (PAP), consult reliable medical sources or healthcare professionals. Understanding the distinctions between primary PAP, secondary PAP, and congenital PAP can aid in tailored treatment approaches.
Primary PAP
Primary pulmonary alveolar proteinosis (PAP) is a rare lung disorder primarily caused by autoantibodies targeting GM-CSF, leading to impaired surfactant clearance. This can result in breathing difficulties and respiratory failure. Consulting healthcare providers for accurate diagnosis and personalized treatment plans is crucial for managing primary PAP effectively.
Secondary PAP
Secondary pulmonary alveolar proteinosis (PAP) occurs as a result of underlying conditions such as lung infections, immune disorders, cancers, or environmental exposures that disrupt surfactant metabolism. It is essential to address the primary cause of secondary PAP in the treatment plan to manage the condition effectively. Seeking medical advice for comprehensive evaluation and individualized therapy is advisable in cases of secondary PAP.
Congenital PAP
Congenital pulmonary alveolar proteinosis (PAP) is a rare form of the disease that is present from birth and can be caused by genetic factors affecting surfactant metabolism. Individuals with congenital PAP may experience breathing difficulties early in life. Seek medical advice for proper diagnosis and management of congenital PAP for optimal outcomes.
Pathophysiology of PAP
Pulmonary alveolar proteinosis (PAP) is a rare lung disorder characterized by the abnormal accumulation of surfactant in the alveoli due to disrupted surfactant clearance mechanisms. This accumulation leads to impaired gas exchange and lung function, resulting in symptoms like shortness of breath and coughing. Understanding the pathophysiology of PAP is crucial for effective diagnosis and treatment planning. Consult healthcare professionals for personalized guidance on managing PAP based on its underlying pathophysiology.
Prognosis and Complications
Understanding the prognosis and potential complications of pulmonary alveolar proteinosis (PAP) is essential for managing the condition effectively. Prognosis can vary depending on the type of PAP and underlying causes, with some cases responding well to treatment while others may have more challenges. Complications of PAP can include respiratory failure, infections, and progression to pulmonary fibrosis. Consulting healthcare professionals for personalized care and regular monitoring can help mitigate complications and improve long-term outcomes for individuals with PAP.
Research and Advancements
Stay informed about the latest research and advancements in the field of pulmonary alveolar proteinosis (PAP) by consulting reputable medical sources or healthcare professionals. Ongoing studies explore the pathophysiology, treatment modalities, and potential breakthroughs in managing PAP. Engage with healthcare providers to access cutting-edge advancements and participate in clinical trials if suitable for personalized care.
PAP Foundation and Patient Support
For individuals affected by pulmonary alveolar proteinosis (PAP), seeking support from organizations like the PAP Foundation can provide valuable resources, information, and community connections for patients and caregivers. The PAP Foundation is a non-profit entity dedicated to advancing research, promoting awareness, and supporting individuals impacted by PAP. Engaging with patient support groups and advocacy organizations can offer emotional support and access to the latest information on managing PAP.
Autoimmune Pulmonary Alveolar Proteinosis (aPAP)
Autoimmune pulmonary alveolar proteinosis (aPAP) is the most common form of pulmonary alveolar proteinosis characterized by the accumulation of surfactant within the alveoli due to disrupted immune function. Some individuals may not exhibit symptoms, while others may experience progressive difficulty breathing. Seeking medical evaluation and appropriate management are vital for individuals with aPAP to improve respiratory function and overall well-being.
Case Studies and Clinical Trials
Exploring case studies and ongoing clinical trials related to pulmonary alveolar proteinosis (PAP) can provide valuable insights into the management and treatment of this rare lung disorder. By examining real-life cases and participating in clinical trials, individuals and healthcare providers can contribute to the advancement of knowledge and potential treatment options for PAP. Engaging with case studies and clinical trials can offer hope for new therapeutic approaches and improved outcomes for individuals living with PAP.

Conclusion and Prevention Strategies
In conclusion, pulmonary alveolar proteinosis (PAP) is a rare lung disorder that requires careful diagnosis and personalized treatment to manage symptoms effectively and improve outcomes. With advancements in research and ongoing clinical trials, there is hope for innovative therapies that can enhance the quality of life for individuals with PAP. To prevent complications associated with PAP, early detection, appropriate medical interventions, and regular follow-ups are crucial. By staying informed and seeking support from healthcare providers and patient advocacy groups, individuals with PAP can navigate their journey with greater resilience and understanding.