Encephalopathy Subacute Spongiform, Gerstmann-Straussler-Scheinker (GSS) Syndrome
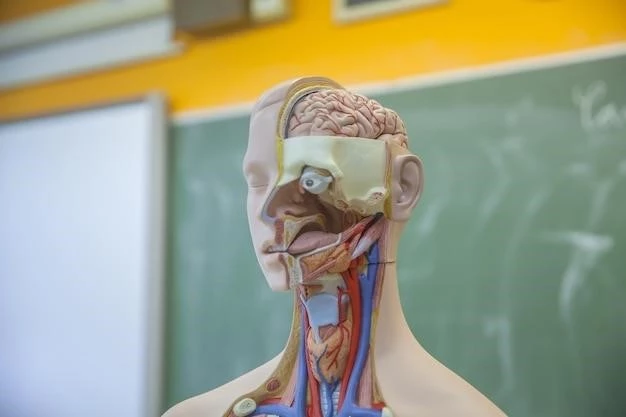
I. Introduction to Encephalopathy Subacute Spongiform
Encephalopathy subacute spongiform is a rare brain disorder characterized by prion diseases such as Gerstmann-Straussler-Scheinker (GSS) syndrome. It manifests with cognitive impairment, memory loss, muscle twitching, coordination problems, speech difficulties, and other neurological symptoms. The disease is caused by genetic mutations leading to protein misfolding and neuropathological changes, including cerebellar ataxia and amyloid plaques. Understanding its symptoms, causes, and diagnostic approaches is crucial for effective management and treatment.
– Definition of Encephalopathy Subacute Spongiform
Encephalopathy subacute spongiform is a prion disease associated with cognitive impairment, memory loss, muscle twitching, coordination problems, speech difficulties, and other neurological symptoms. It is caused by a genetic mutation leading to protein misfolding in the brain, resulting in neuropathological changes such as cerebellar ataxia and the formation of amyloid plaques. Early diagnosis and understanding of this disorder are crucial for implementing appropriate treatment strategies and improving patient outcomes.
– Overview of Gerstmann-Straussler-Scheinker (GSS) Syndrome
Gerstmann-Straussler-Scheinker (GSS) syndrome is a rare prion disease that falls under the spectrum of encephalopathy subacute spongiform. It is characterized by progressive cognitive impairment, memory loss, muscle twitching, coordination problems, and speech difficulties. This syndrome is linked to genetic mutations causing abnormal protein folding in the brain, leading to the development of neurological symptoms. Understanding the distinct features of GSS is essential for accurate diagnosis and tailored treatment interventions.
II. Understanding Prion Diseases
Prion diseases are neurological disorders caused by the misfolding of normal cellular proteins into abnormal forms known as prions. These prions can induce other proteins to misfold, leading to a cascade effect within the brain. This protein misfolding results in severe neuropathological changes and the formation of amyloid plaques. Prion diseases, including encephalopathy subacute spongiform and Gerstmann-Straussler-Scheinker (GSS) syndrome, present unique challenges in diagnosis and management due to their complex nature and progressive neurological manifestations.
– Explanation of Prion Diseases
Prion diseases are a group of rare and fatal brain disorders caused by misfolded proteins, known as prions. These abnormal proteins can induce the misfolding of normal proteins in the brain, leading to the accumulation of prion aggregates. This process results in the formation of amyloid plaques and neurodegeneration. Prion diseases such as encephalopathy subacute spongiform and Gerstmann-Straussler-Scheinker (GSS) syndrome are challenging to treat due to their unique pathophysiology involving protein misfolding and neurological damage.
– Characteristics of Prion Diseases
Prion diseases are unique due to the self-propagation of misfolded proteins, leading to progressive neurological damage. These disorders exhibit long incubation periods, varied clinical presentations, and are typically fatal. The presence of amyloid plaques in the brain, along with cognitive decline, muscle twitching, coordination issues, and speech impairments, distinguishes prion diseases like encephalopathy subacute spongiform and Gerstmann-Straussler-Scheinker (GSS) syndrome from other neurodegenerative conditions. Comprehensive understanding of these distinct features is vital for effective management strategies.
III. Symptoms of Encephalopathy Subacute Spongiform
Encephalopathy subacute spongiform presents with cognitive impairment affecting memory and reasoning abilities. Patients may experience muscle twitching, coordination problems leading to unsteadiness, and speech difficulties. Other neurological symptoms include vision changes, involuntary movements, and personality alterations. Recognizing these diverse manifestations is crucial for timely diagnosis and appropriate management of this complex brain disorder. Understanding these symptoms can help healthcare professionals provide tailored care and support to individuals affected by the disease.
– Cognitive Impairment

Cognitive impairment is a hallmark symptom of encephalopathy subacute spongiform, affecting memory, attention, and decision-making processes. Patients may struggle with learning new information, solving problems, and maintaining focus. As the disease progresses, individuals may experience confusion, disorientation, and difficulties in communicating effectively. Early recognition of cognitive changes is essential for initiating appropriate interventions to support cognitive function and quality of life for those affected by this debilitating neurological condition.
– Memory Loss
Memory loss is a common symptom in encephalopathy subacute spongiform, where patients experience difficulties in recalling information, forming new memories, and recognizing familiar faces or places. Short-term memory deficits often progress to affect long-term memory functions. Individuals may struggle with maintaining daily routines, remembering recent events, and recalling past experiences. Addressing memory loss early in the disease course is vital for implementing memory aids, cognitive exercises, and supportive strategies to enhance quality of life and functional independence.
– Muscle Twitching
Muscle twitching, known as fasciculations, is a characteristic symptom of encephalopathy subacute spongiform. Patients may experience involuntary contractions of muscle fibers, leading to visible or subtle movements under the skin. These twitching episodes can affect various muscle groups, causing discomfort and interference with motor functions. Recognizing and addressing muscle twitching early is crucial to managing any associated discomfort or functional limitations, as part of the comprehensive care approach for individuals with this progressive brain disorder.
– Coordination Problems
Coordination problems are prevalent in encephalopathy subacute spongiform, leading to challenges in fine motor skills, balance, and gait control. Individuals may exhibit unsteadiness, difficulty with precise movements, and impaired ability to perform coordinated tasks. Coordination issues can impact daily activities, increase the risk of falls, and affect overall mobility. Early recognition and intervention to address coordination problems through physical therapy, assistive devices, and safety measures are essential in improving quality of life and minimizing functional limitations for individuals with this neurological condition.
– Speech Difficulties
Speech difficulties, such as dysarthria and language impairment, are common manifestations of encephalopathy subacute spongiform. Patients may struggle with articulation, fluency, and voice modulation, impacting their ability to communicate effectively. Speech difficulties can result in misunderstandings, frustration, and social isolation. Speech therapy, augmentative communication strategies, and assistive technologies play a key role in improving communication skills and maintaining social connections for individuals with this neurodegenerative condition.
– Other Neurological Symptoms
Encephalopathy subacute spongiform may present with various additional neurological symptoms beyond cognitive and motor impairments. These can include vision disturbances, sensory abnormalities, emotional changes, and sleep disturbances. Individuals may also experience involuntary movements, seizures, and worsening neurological deficits as the disease progresses. Recognizing and addressing these diverse neurological symptoms through comprehensive evaluation and symptom management is essential in providing holistic care and improving quality of life for individuals affected by this complex brain disorder.
IV. Causes of Encephalopathy Subacute Spongiform
The underlying causes of encephalopathy subacute spongiform primarily stem from genetic mutations impacting prion protein folding. These mutations result in the misfolding of normal cellular proteins and the accumulation of dysfunctional prions in the brain. The abnormal prions trigger a cascade of neuropathological changes, contributing to the characteristic symptoms of the disease. Understanding the genetic basis and protein misfolding mechanisms involved in encephalopathy subacute spongiform is crucial for advancing diagnostic methods and developing targeted therapeutic strategies to address this rare and complex neurological disorder effectively.
– Genetic Mutation
Genetic mutations play a fundamental role in the development of encephalopathy subacute spongiform, altering the structure of prion proteins. These mutations lead to the abnormal folding of prions in the brain, initiating a chain reaction that results in neuropathological changes and neurological symptoms. Understanding the specific genetic alterations associated with this disease is essential for genetic counseling, early detection, and personalized management. Research into genetic mutations continues to shed light on the intricate mechanisms underlying the pathogenesis of this rare neurodegenerative disorder.
– Protein Misfolding
Protein misfolding is a central pathological process in encephalopathy subacute spongiform, where normal prion proteins undergo conformational changes leading to the formation of misfolded prions. These abnormal proteins aggregate in the brain, disrupting cellular processes and causing neuronal damage. The phenomenon of protein misfolding serves as a key mechanism in the pathogenesis of this prion disease, highlighting the importance of unraveling the intricate molecular events involved in misfolding and aggregation for advancing therapeutic interventions and disease management.
V. Neuropathological Changes in Encephalopathy Subacute Spongiform
Encephalopathy subacute spongiform is characterized by distinct neuropathological changes in the brain, including cerebellar ataxia and the deposition of amyloid plaques. Cerebellar ataxia manifests as coordination difficulties and impaired voluntary movements due to cerebellar dysfunction. The formation of amyloid plaques, composed of misfolded prion proteins, contributes to neurodegeneration. Understanding these neuropathological alterations is crucial for elucidating the disease mechanisms and developing targeted therapeutic approaches to address the underlying pathology effectively.
– Cerebellar Ataxia
Cerebellar ataxia is a prominent feature of encephalopathy subacute spongiform, characterized by progressive coordination problems, unsteadiness, and difficulties in controlling movements. The dysfunction of the cerebellum, a brain region essential for motor coordination, leads to impaired balance and gait disturbances. Cerebellar ataxia significantly impacts daily activities and mobility. Recognizing and addressing this symptom early in the disease course is crucial for implementing interventions such as physical therapy and assistive devices to enhance motor function and quality of life for affected individuals.
– Formation of Amyloid Plaques
Encephalopathy subacute spongiform is marked by the accumulation of misfolded prion proteins that form amyloid plaques in the brain. These plaques disrupt normal brain function, contributing to neurodegeneration and clinical manifestations of the disease. The aggregation of amyloid proteins is a key neuropathological hallmark, indicative of the underlying protein misfolding processes. Understanding the formation and implications of amyloid plaques is crucial for unraveling the disease mechanisms and developing targeted interventions aimed at mitigating their impact on neurological function.
VI. Diagnosis of Encephalopathy Subacute Spongiform
Diagnosing encephalopathy subacute spongiform involves a comprehensive approach, including clinical evaluation, imaging studies such as MRI or PET scans to assess brain abnormalities, and genetic testing to identify relevant mutations. Combining these diagnostic modalities allows healthcare professionals to establish a definitive diagnosis and differentiate the disease from other neurological conditions presenting similar symptoms. Early and accurate diagnosis is essential for timely intervention and the initiation of appropriate management strategies tailored to the individual’s specific needs.
– Clinical Evaluation
Clinical evaluation plays a critical role in diagnosing encephalopathy subacute spongiform, involving a detailed assessment of the patient’s medical history, neurological examination, and cognitive function tests. Healthcare providers rely on clinical observations to identify characteristic symptoms such as cognitive impairment, motor deficits, and speech difficulties. The information gathered during the clinical evaluation guides further diagnostic procedures and informs the treatment plan for individuals suspected of having this rare and complex neurodegenerative disorder.
– Imaging Studies
Imaging studies play a crucial role in the diagnostic workup of encephalopathy subacute spongiform, offering insights into brain structures and identifying abnormalities. Techniques such as magnetic resonance imaging (MRI) and positron emission tomography (PET) scans allow for the visualization of structural changes, patterns of brain dysfunction, and the presence of characteristic lesions. These imaging modalities aid clinicians in confirming the diagnosis, monitoring disease progression, and informing treatment decisions for individuals affected by this complex neurodegenerative condition.
– Genetic Testing
Genetic testing is a key component of diagnosing encephalopathy subacute spongiform, aiming to identify specific mutations associated with the disease. This test helps determine the presence of genetic abnormalities linked to protein misfolding and prion diseases. By analyzing the individual’s genetic makeup, healthcare providers can confirm a genetic predisposition to the condition, offer genetic counseling to affected individuals and their families, and tailor treatment strategies based on the underlying genetic factors contributing to the neuropathology of this rare neurological disorder.
VII. Treatment Options for Encephalopathy Subacute Spongiform
Managing encephalopathy subacute spongiform involves symptomatic management to address cognitive, motor, and speech impairments. Experimental therapies, such as immunotherapies and targeted drug interventions, aim to modify disease progression. Supportive care for daily activities and quality of life enhancement is essential. Collaborative efforts between healthcare professionals, patients, and caregivers are crucial in implementing a multi-disciplinary approach to alleviate symptoms and enhance the overall well-being of individuals affected by this challenging neurodegenerative disorder.
– Symptomatic Management
Symptomatic management of encephalopathy subacute spongiform focuses on alleviating cognitive impairment, motor dysfunction, and speech difficulties through supportive interventions. Therapeutic strategies aim to enhance quality of life, improve daily functioning, and address specific symptoms experienced by individuals with the disease. Symptomatic management may involve cognitive exercises, physical therapy, speech therapy, and assistive devices to optimize patient comfort and maintain overall well-being in the face of the progressive neurological changes associated with this complex neurodegenerative condition.
– Experimental Therapies
Experimental therapies for encephalopathy subacute spongiform explore innovative approaches such as immunotherapies and pharmacological interventions targeting prion propagation and protein misfolding. These experimental treatments aim to slow disease progression and alleviate symptoms by modifying the underlying pathology. Research into novel therapeutic strategies offers promising avenues for developing targeted interventions to address the complex neurodegenerative mechanisms involved in this rare brain disorder. Continued exploration of experimental therapies is vital for advancing treatment options and improving outcomes for individuals affected by this challenging condition.
– Supportive Care
Supportive care plays a crucial role in managing encephalopathy subacute spongiform, providing comprehensive assistance to individuals with cognitive, motor, and communication challenges. Supportive care measures encompass physical assistance, emotional support, and assistance with daily activities to improve quality of life. This holistic approach involves optimizing comfort, promoting independence, and addressing the diverse needs of patients with this progressive neurodegenerative disorder. Implementing a personalized supportive care plan enhances the overall well-being and functional capacity of individuals living with the complexities of this debilitating brain disorder.
VIII. Research and Developments in GSS Syndrome
Ongoing research in Gerstmann-Straussler-Scheinker (GSS) syndrome focuses on understanding the genetic basis, protein misfolding mechanisms, and neuropathological changes associated with this rare prion disease. Recent studies explore potential therapeutic targets, novel treatment approaches, and biomarkers for early detection. Advances in GSS research aim to improve diagnostic accuracy, develop disease-modifying therapies, and enhance patient care strategies. The evolving landscape of GSS research underscores the importance of continued scientific exploration to advance knowledge and future treatment options for individuals affected by this challenging neurodegenerative condition.
– Recent Studies
Recent studies on Gerstmann-Straussler-Scheinker (GSS) syndrome have delved into genetic mutations, protein aggregation pathways, and potential therapeutic interventions. Research has explored the role of prion propagation, neuroinflammation, and synaptic dysfunction in disease pathogenesis. Novel imaging techniques and biomarkers are being investigated for early diagnosis and disease monitoring. Clinical trials testing experimental treatments show promise in modifying disease progression. The findings from recent studies offer hope for advancing the understanding and management of GSS syndrome, paving the way for innovative approaches in addressing this complex prion disorder.
– Importance of Early Detection and Management
Early detection and management of encephalopathy subacute spongiform and Gerstmann-Straussler-Scheinker (GSS) syndrome are paramount in improving patient outcomes and quality of life. Timely diagnosis allows for early intervention, symptom relief, and implementation of supportive care measures. Effective disease management strategies, including experimental therapies and symptomatic treatments, can help delay disease progression and preserve cognitive and motor function. Heightened awareness among healthcare professionals and timely genetic testing are essential for identifying at-risk individuals and initiating proactive management approaches to mitigate the impact of these challenging neurodegenerative conditions.