Disease ⸺ Hypogonadism Hypogonadotropic Due to Mutations in GR Hormone
Hypogonadism hypogonadotropic is a genetic disorder in the endocrine system affecting reproductive health. Mutations in the GR hormone lead to testosterone deficiency, impacting growth and development. Proper medical treatment and hormone replacement therapy are essential for managing this condition.
I. Introduction to Hypogonadism Hypogonadotropic Disorder
Hypogonadism hypogonadotropic is an endocrine disorder characterized by insufficient activity of the reproductive system due to decreased levels of sex hormones. In this condition, the gonads produce little to no hormones, affecting fertility and sexual development. Mutations in genes such as the GR hormone can disrupt the hormonal balance, leading to hypogonadism. This disorder can manifest at different stages of life, impacting both males and females.
Individuals with hypogonadotropic disorder may experience delayed puberty, infertility, decreased libido, and various physical and emotional symptoms. It is essential to diagnose this condition early to prevent complications and provide appropriate medical care. Understanding the genetic basis of hypogonadism is crucial in developing effective treatment strategies. As research continues to explore the mechanisms behind this disorder, advancements in diagnosis and therapy offer hope for individuals affected by hypogonadotropic hypogonadism.
II. Understanding Hypogonadism
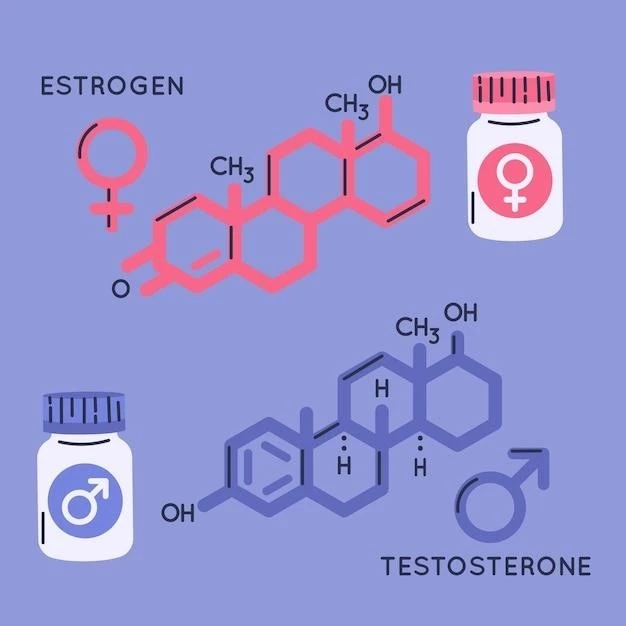
Hypogonadism is a medical condition characterized by the body’s inability to produce adequate amounts of sex hormones, such as testosterone in males and estrogen in females. In the case of hypogonadotropic hypogonadism, the underlying cause is often related to issues within the endocrine system, specifically affecting the hypothalamus and pituitary glands.
Individuals with hypogonadism may experience a range of symptoms, including reduced sex drive, erectile dysfunction, fatigue, and infertility. The impact of hypogonadism extends beyond reproductive health, affecting metabolic processes, bone density, and overall well-being. Understanding the mechanisms that lead to hormone deficiency is essential in diagnosing and managing this condition effectively.
III. Hypogonadotropic vs. Hypergonadotropic Disorders
Hypogonadotropic and hypergonadotropic disorders are two categories of conditions that affect the reproductive system. In hypogonadotropic disorders like hypogonadotropic hypogonadism, there is a deficiency in the production of sex hormones due to impaired signaling from the hypothalamus and pituitary glands.
On the other hand, hypergonadotropic disorders are characterized by elevated levels of gonadotropins (hormones that stimulate the gonads) in response to low sex hormone levels. These disorders often result from a primary dysfunction of the testes or ovaries, leading to decreased production of sex hormones despite increased gonadotropin levels.
Understanding the distinction between hypogonadotropic and hypergonadotropic disorders is essential in determining the appropriate diagnostic tests and treatment strategies; While hypogonadotropic disorders require interventions to stimulate hormone production, hypergonadotropic disorders may necessitate addressing the underlying issues causing gonadal dysfunction;
IV. The Role of Mutations in GR Hormone
Mutations in the GR hormone, also known as the gonadotropin-releasing hormone, play a critical role in the development of hypogonadotropic hypogonadism. The GR hormone is responsible for signaling the pituitary gland to release gonadotropins, which then stimulate the production of sex hormones in the gonads.
When mutations occur in the gene encoding the GR hormone or its receptors, disruptions in this signaling pathway can lead to inadequate production of sex hormones. These mutations can impact the hypothalamic-pituitary-gonadal axis, causing imbalances that result in hypogonadotropic disorders.
Understanding the specific genetic alterations that affect the GR hormone is crucial in diagnosing and treating hypogonadotropic hypogonadism. Research into the mechanisms of these mutations can help develop targeted therapies that restore hormone production and reproductive function in individuals affected by this disorder.
V. Genetic Basis of Hypogonadism
The genetic basis of hypogonadism, particularly hypogonadotropic hypogonadism, involves mutations that disrupt the synthesis or function of key hormones involved in reproductive health. Mutations in genes encoding gonadotropin-releasing hormone (GRH) or its receptors, as well as other genes along the hypothalamic-pituitary-gonadal axis, can lead to this disorder.
These genetic mutations interfere with the intricate hormonal signaling cascade necessary for normal development and function of the reproductive system. Variations in genes controlling the production and release of sex hormones can result in disrupted pubertal development, infertility, and other symptoms associated with hypogonadotropic hypogonadism.
Advances in genetic testing and molecular analysis have enabled healthcare providers to identify specific mutations associated with hypogonadism, allowing for personalized approaches to treatment. Understanding the genetic underpinnings of hypogonadotropic disorders is essential for accurate diagnosis, genetic counseling, and the development of targeted therapies to address the root cause of the condition.
VI. Diagnosis and Symptoms of Hypogonadotropic Disorder
Diagnosing hypogonadotropic disorder involves a comprehensive evaluation of symptoms, medical history, and laboratory tests to assess hormone levels. Common symptoms of this disorder include delayed puberty, lack of secondary sexual characteristics, infertility, and sexual dysfunction. In males, symptoms may include decreased muscle mass, reduced facial hair growth, and fatigue.
Diagnostic tests for hypogonadotropic disorder may include blood tests to measure hormone levels, genetic testing to identify mutations in key genes such as the GR hormone, and imaging studies to evaluate the structure of the pituitary gland. Early detection of hypogonadotropic disorder is crucial for implementing timely interventions to address hormone deficiencies and improve quality of life.
Healthcare providers may also consider the impact of hypogonadism on mental health and overall well-being when developing a treatment plan. By recognizing the symptoms and diagnosing hypogonadotropic disorder promptly, individuals can receive appropriate medical care to manage the condition effectively and minimize potential complications.
VII. Effects of Hypogonadism on Growth and Development
Hypogonadism, particularly hypogonadotropic hypogonadism, can have significant effects on growth and development due to hormone imbalances affecting the body’s maturation processes. In children and adolescents, low levels of sex hormones can delay the onset of puberty, resulting in stunted growth and delayed skeletal maturation.
Moreover, hypogonadism can impact the development of secondary sexual characteristics, such as the growth of body hair, breast tissue in females, and voice deepening in males. Hormone deficiencies can also affect bone density, potentially leading to osteoporosis and an increased risk of fractures over time.
Managing hypogonadism early on is crucial in promoting healthy growth and development in individuals affected by this condition. Hormone replacement therapy can help restore hormone levels to appropriate ranges, supporting optimal growth, bone health, and overall well-being throughout various life stages.
VIII. Medical Complications of Testosterone Deficiency
Testosterone deficiency, a common consequence of hypogonadism, can lead to various medical complications impacting multiple body systems. In males, low testosterone levels may contribute to erectile dysfunction, decreased muscle mass and strength, and changes in mood and cognition.
Additionally, testosterone plays a crucial role in maintaining bone density and red blood cell production. Therefore, a deficiency in this hormone can increase the risk of osteoporosis and anemia. In adolescents with hypogonadism, testosterone deficiency can hinder pubertal development and affect physical and emotional well-being.
Managing the medical complications associated with testosterone deficiency involves hormone replacement therapy to restore testosterone levels to within the normal range. By addressing hormone imbalances early on, healthcare providers can help mitigate the risk of long-term complications related to hypogonadism and improve the quality of life for individuals affected by this condition.
IX; Treatment Options for Hypogonadotropic Disorder
The treatment of hypogonadotropic disorder aims to address hormone deficiencies and improve reproductive and overall health outcomes. Hormone replacement therapy (HRT) is a common approach to managing this condition, involving the administration of synthetic hormones to restore normal hormone levels.
For individuals with hypogonadotropic hypogonadism, HRT can include testosterone replacement in males or estrogen and progesterone replacement in females. By replenishing deficient hormones, HRT can help alleviate symptoms such as infertility, sexual dysfunction, and menstrual irregularities.
Other treatment options for hypogonadotropic disorder may involve the use of medications to stimulate hormone production, fertility treatments for individuals seeking to conceive, and lifestyle modifications to support overall hormonal balance. In cases where genetic mutations in the GR hormone are identified, targeted therapies may be developed to address the underlying cause of the disorder.
X. Hormone Replacement Therapy for Hypogonadism
Hormone replacement therapy (HRT) is a cornerstone in managing hypogonadism, especially in cases of hypogonadotropic hypogonadism resulting from mutations in the GR hormone. HRT involves administering synthetic hormones to compensate for deficiencies and restore hormonal balance in the body.
In males with hypogonadism, testosterone replacement therapy is commonly used to address symptoms such as reduced libido, fatigue, and erectile dysfunction. By supplementing testosterone levels, HRT can improve muscle mass, bone density, and overall well-being in affected individuals. For females with hypogonadotropic disorder, estrogen and progesterone replacement therapy may be prescribed to regulate menstrual cycles and alleviate symptoms related to hormone deficiencies.
It is essential for individuals undergoing hormone replacement therapy to receive regular monitoring by healthcare providers to adjust hormone dosages as needed and assess treatment effectiveness. Through tailored HRT regimens, individuals with hypogonadism can manage their condition effectively and improve their quality of life.
XI. Managing Hypogonadism in Reproductive Health
Effective management of hypogonadism in the context of reproductive health requires a multifaceted approach to address hormonal imbalances and optimize fertility outcomes. For individuals with hypogonadotropic hypogonadism resulting from mutations in the GR hormone, targeted interventions are essential to support reproductive function.
Healthcare providers may recommend hormone replacement therapy to restore normal hormone levels, improve fertility, and regulate menstrual cycles in females. In males, testosterone replacement therapy can enhance sperm production and facilitate natural conception. Fertility treatments, such as in vitro fertilization (IVF) or intrauterine insemination (IUI), may be explored in cases where natural conception is challenging.
Genetic counseling can play a vital role in managing hypogonadism in reproductive health, offering insight into the hereditary nature of the disorder and its implications for family planning. By combining medical treatments with reproductive assistance and genetic guidance, individuals with hypogonadotropic disorder can navigate the complexities of fertility and reproductive health with the support of a knowledgeable healthcare team.
XII. Living with Hypogonadism⁚ Coping Strategies
Living with hypogonadism, particularly hypogonadotropic hypogonadism due to mutations in the GR hormone, can present unique challenges that impact physical, emotional, and social well-being. Coping strategies play a crucial role in helping individuals navigate the complexities of this condition and enhance their quality of life.
Engaging in regular exercise and maintaining a balanced diet can promote overall health and well-being in individuals with hypogonadism. Seek support from healthcare professionals, support groups, or mental health resources to address emotional challenges and coping mechanisms related to the condition.
Open communication with loved ones and healthcare providers is key to managing hypogonadism effectively. Establishing a reliable support network and staying informed about the latest research and treatment options can empower individuals living with this condition to take an active role in their health and well-being.
XIII. Research and Future Prospects in Hypogonadism Treatment
Ongoing research in hypogonadotropic hypogonadism, specifically focusing on mutations in the GR hormone, holds promise for advancing treatment options and improving outcomes for individuals with this condition. Scientists are investigating novel therapeutic approaches, including targeted gene therapies and hormone replacement strategies tailored to individual genetic profiles.
Advancements in genetic testing technologies have enhanced the identification of specific mutations associated with hypogonadotropic disorder, paving the way for personalized treatment plans based on an individual’s genetic makeup. Researchers are also exploring the potential of gene editing techniques such as CRISPR-Cas9 to correct genetic mutations underlying hypogonadism.
Future prospects in hypogonadism treatment aim to not only address hormonal imbalances but also improve fertility outcomes, enhance quality of life, and mitigate long-term complications associated with the disorder. Collaborative efforts between researchers, healthcare providers, and advocacy groups are critical in driving innovation and improving the management of hypogonadotropic hypogonadism.
XIV. Conclusion
In conclusion, hypogonadism hypogonadotropic due to mutations in the GR hormone is a complex genetic disorder that affects reproductive health and overall well-being. Understanding the genetic basis of hypogonadotropic disorder is essential for accurate diagnosis and personalized treatment strategies.
The role of mutations in the GR hormone underscores the importance of genetic testing and targeted therapies in managing this condition effectively. Hormone replacement therapy plays a pivotal role in restoring hormonal balance and improving quality of life for individuals with hypogonadism.
Looking ahead, ongoing research and advancements in treatment options offer hope for enhanced outcomes and better management of hypogonadotropic hypogonadism. By combining medical interventions, reproductive health support, and genetic counseling, individuals living with this condition can navigate the complexities of hypogonadism with comprehensive care and personalized solutions.
XV. References
- Chan JL, Seminara SB. How to Treat Hypogonadism. J Clin Endocrinol Metab. 2021;106(5)⁚1248-1263. doi⁚10.1210/clinem/dgab175
- Meachem SJ, Nieschlag E, Simoni M. Genetic causes of male infertility. J Endocrinol; 2001;168(3)⁚401-415. doi⁚10.1677/joe.0.1680401
- Stamou MI, Cox KH, Crowley WF Jr. Discovering Genes Essential to the Hypothalamic Regulation of Human Reproduction Using a Human Disease Model⁚ Adjusting to Life in the ″-omics″ Era. Endocr Rev. 2016;37(5)⁚364-411. doi⁚10.1210/er.2016-1016
- Tarif N, Shah J, Kotlyar M. Gonadotropin-Releasing Hormone Deficiency. In⁚ StatPearls. Treasure Island (FL)⁚ StatPearls Publishing; 2022. Available from⁚ https://www.ncbi.nlm.nih.gov/books/NBK554484/
- Wierman ME, Arlt W, Basson R, et al. Androgen therapy in women⁚ a reappraisal⁚ an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(10)⁚3489-3510. doi⁚10.1210/jc.2014-2262