Morphea scleroderma is an idiopathic inflammatory disorder that causes sclerotic changes in the skin. It is crucial to understand its activity, depth, involvement, and treatment options.
Morphea, also known as localized scleroderma, is an autoimmune connective tissue disorder that primarily affects the skin and subcutaneous tissue. It presents as patchy or banded thickening of the skin, with varying clinical presentations depending on the subtype. Understanding the progression, diagnosis, and potential complications of Morphea is essential for effective management and treatment strategies.
Morphea Definition and Characteristics
Morphea, also known as localized scleroderma, is an autoimmune connective tissue disorder primarily affecting the skin. Understanding its presentation and progression is key to effective management.
Morphea, characterized by an annual incidence of 0.4-2.7 cases per 100٫000٫ predominantly affects children aged 2-14 years٫ showing a higher occurrence in females. Understanding the demographic patterns and incidence rates is crucial for early detection and tailored treatment approaches.
Morphea has an annual incidence of 0.4-2.7 cases per 100,000, affecting mostly children aged 2-14 years with a higher prevalence in females. Understanding these demographics is crucial for early detection and personalized care.
Autoimmune Nature and Triggers
Morphea scleroderma is an autoimmune condition where the immune system mistakenly attacks the body’s tissues, leading to scar-like changes in the skin. Understanding the autoimmune nature and potential triggers of morphea is crucial for disease management and preventive strategies to minimize flare-ups and complications.
Incidence and Demographics
Morphea, characterized by an annual incidence of 0.4-2.7 cases per 100٫000٫ predominantly affects children aged 2-14 years٫ showing a higher occurrence in females. Understanding the demographic patterns and incidence rates is crucial for early detection and tailored treatment approaches.
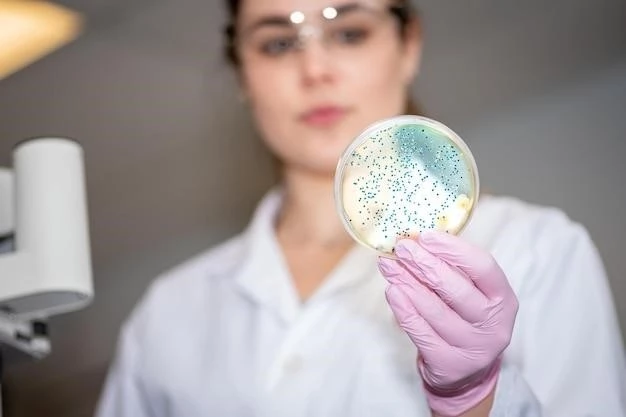
Diagnosing Morphea scleroderma involves visual examination, medical history review, and often a skin biopsy to confirm the presence of characteristic changes in the skin’s different layers. Skin biopsy aids in identifying the specific characteristics of Morphea, assisting in accurate diagnosis and treatment planning.
Diagnostic Procedures and Skin Biopsy
Diagnosing Morphea scleroderma often involves physical examination, medical history review, and skin biopsy. A skin biopsy can confirm the presence of characteristic changes in the skin’s layers, aiding in accurate diagnosis and treatment planning.
When dealing with Morphea scleroderma, a variety of treatment options are available, including systemic therapy, phototherapy, occupational therapy, and physical therapy. These approaches aim to manage symptoms, reduce inflammation, and improve skin condition. Understanding the therapeutic options and developing a comprehensive management strategy tailored to individual needs can enhance the patient’s quality of life and potentially slow disease progression.
Therapeutic Approaches and Management Strategies
When dealing with Morphea scleroderma, various therapeutic approaches like systemic therapy, phototherapy, occupational therapy, and physical therapy play key roles in managing symptoms, reducing inflammation, and improving skin condition. Developing a personalized management strategy based on these therapeutic options can significantly impact the patient’s quality of life and potentially slow down the disease progression. It is important to discuss these treatment modalities with healthcare providers to formulate the most effective plan tailored to individual needs.
Long-Term Outlook and Potential Risks
Understanding the long-term outlook for Morphea scleroderma and potential risks associated with the condition is crucial for managing the disease effectively. Prognosis may vary depending on the subtype and extent of skin involvement. By staying informed about the potential risks, individuals can work closely with healthcare providers to monitor and address any complications that may arise over time, ensuring comprehensive care and optimized quality of life.

