Histidinuria Renal Tubular Defect Syndrome
This article aims to provide an in-depth exploration of the rare genetic disorder‚ Histidinuria Renal Tubular Defect Syndrome. It will cover various aspects including symptoms‚ renal function‚ complications‚ treatment options‚ genetic basis‚ preventive measures‚ prognosis‚ and future research directions.
Introduction
Histidinuria Renal Tubular Defect Syndrome is a rare inherited disorder characterized by a deficiency in histidase enzyme activity‚ leading to the impaired metabolism of the amino acid histidine. This genetic anomaly results in the accumulation of histidine in the blood‚ leading to elevated levels excreted in the urine. The kidneys play a crucial role in excreting excess histidine‚ hence the renal tubular defect component of the syndrome.
The disorder is typically diagnosed through urine tests that reveal high levels of histidine. Symptoms may vary but can include developmental delays‚ behavioral issues‚ and neurological problems. Monitoring renal function is essential due to the impact of histidinuria on kidney health.
Complications of Histidinuria can arise if the condition is not managed effectively. Treatment often involves dietary adjustments and sometimes supplementation with vitamin B6 to aid in histidine breakdown. Preventive measures focus on early detection and intervention to prevent long-term complications.
Understanding the genetic basis of Histidinuria is crucial for proper management. Prognosis varies but with early diagnosis and appropriate treatment‚ outcomes can be favorable. Research in this field aims to improve diagnostic techniques‚ treatment options‚ and enhance our understanding of the disorder’s underlying mechanisms.
This article delves into the complexities of Histidinuria Renal Tubular Defect Syndrome‚ shedding light on various aspects of the condition to provide a comprehensive overview for healthcare professionals and individuals affected by this rare genetic disorder.
Understanding Histidinuria
Histidinuria is a rare genetic disorder characterized by a deficiency in histidase enzyme‚ essential for histidine metabolism. Histidine is an amino acid vital for protein synthesis and neurotransmitter function. In individuals with Histidinuria‚ the impaired breakdown of histidine leads to its accumulation in the blood and subsequent excretion in high levels through the urine.
Individuals with Histidinuria may present with a range of symptoms including developmental delays‚ intellectual disability‚ hyperactivity‚ and behavioral problems. The neurological manifestations of the disorder can result from the accumulation of histidine and its by-products affecting the central nervous system.
Diagnosis of Histidinuria is typically confirmed through urine tests that reveal elevated levels of histidine. Genetic testing may further identify mutations in the gene responsible for histidase production‚ elucidating the inherited nature of the disorder.
Understanding the intricacies of Histidinuria is crucial for effective management of the condition. By comprehending the underlying genetic basis and metabolic processes involved‚ healthcare professionals can tailor treatment strategies to address the specific needs of individuals with Histidinuria. Timely intervention and close monitoring are paramount in preventing complications and optimizing outcomes for patients with this rare inherited disorder.
Symptoms and Diagnosis
Symptoms of Histidinuria renal tubular defect syndrome can vary but commonly include developmental delays‚ behavioral issues‚ intellectual disability‚ and neurological manifestations such as seizures and hyperactivity. These symptoms stem from the accumulation of histidine due to the enzyme deficiency‚ impacting various physiological processes.
Diagnosis of Histidinuria involves urine tests that detect elevated levels of histidine and imidazoleacetic acid. Genetic testing may reveal mutations in the histidase gene‚ confirming the inherited nature of the disorder. Additionally‚ individuals with Histidinuria may exhibit distinctive features on imaging studies‚ such as renal tubular defects and changes in kidney structure.
Early detection of Histidinuria is key to initiating prompt intervention and preventing potential complications associated with the disorder. Healthcare providers must maintain a high index of suspicion for Histidinuria in patients presenting with developmental delays or unexplained neurological symptoms. A comprehensive diagnostic approach‚ including biochemical‚ genetic‚ and imaging studies‚ is essential for accurate identification of Histidinuria.
By recognizing the hallmark symptoms and employing appropriate diagnostic techniques‚ healthcare professionals can efficiently diagnose Histidinuria renal tubular defect syndrome‚ enabling timely initiation of targeted interventions to manage the condition effectively and improve the long-term outcomes for individuals affected by this rare genetic disorder.
Renal Function in Histidinuria
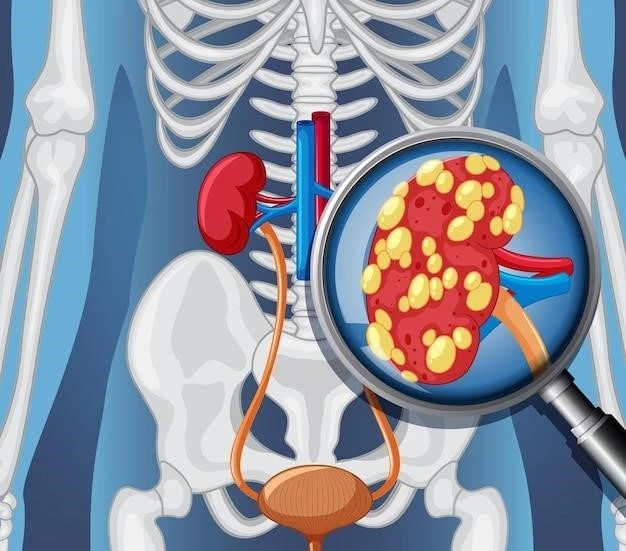
Renal function plays a critical role in Histidinuria renal tubular defect syndrome due to the disorder’s impact on the kidneys. Individuals with Histidinuria exhibit impaired histidine metabolism‚ leading to the accumulation of histidine in the blood‚ which is subsequently excreted in high concentrations through the urine.
The excessive excretion of histidine places a burden on the renal tubules‚ affecting their ability to reabsorb essential nutrients and regulate electrolyte balance efficiently. This renal tubular defect component of Histidinuria underscores the importance of monitoring kidney function in individuals with the condition.
Over time‚ the chronic accumulation of histidine and its by-products in the kidneys can result in renal complications‚ such as tubular dysfunction and structural changes within the kidney tissue. Regular assessment of renal function through laboratory tests and imaging studies is essential to detect early signs of kidney involvement and initiate appropriate interventions.
Healthcare professionals must closely monitor renal function in individuals with Histidinuria to prevent progressive kidney damage and preserve renal health. By assessing renal function regularly and addressing any abnormalities promptly‚ healthcare providers can mitigate the impact of Histidinuria on renal function and optimize outcomes for patients affected by this rare genetic disorder.
Complications of Histidinuria
Histidinuria‚ while rare‚ can lead to various complications if not managed effectively; The accumulation of histidine in individuals with Histidinuria can impact multiple organ systems‚ including the kidneys‚ central nervous system‚ and metabolic pathways. One of the primary complications of Histidinuria is related to renal function.
Prolonged exposure of the kidneys to elevated levels of histidine can result in renal tubular dysfunction‚ impairing the organ’s ability to maintain fluid and electrolyte balance effectively. This dysfunction may lead to the development of kidney stones‚ urinary tract infections‚ and other renal complications over time if left unchecked.
Furthermore‚ the neurological complications of Histidinuria‚ stemming from histidine accumulation in the central nervous system‚ can manifest as developmental delays‚ intellectual disability‚ and behavioral issues. Seizures and motor disturbances may also occur‚ impacting the individual’s quality of life.
Metabolically‚ Histidinuria can disrupt the balance of amino acids and neurotransmitters in the body‚ potentially affecting various physiological processes. These metabolic imbalances can contribute to additional complications such as metabolic acidosis‚ growth disturbances‚ and immune system dysregulation.
Effective management and close monitoring of individuals with Histidinuria are essential to mitigate the risk of complications and optimize long-term outcomes. By addressing the renal‚ neurological‚ and metabolic aspects of the disorder through targeted interventions‚ healthcare providers can help prevent or minimize the impact of complications associated with Histidinuria‚ improving the quality of life for affected individuals.
Treatment and Management
The treatment and management of Histidinuria renal tubular defect syndrome focus on mitigating the impact of histidine accumulation and addressing associated complications. Dietary modifications play a key role in managing Histidinuria‚ with a focus on limiting histidine-rich foods to reduce the burden on histidine metabolism.
In some cases‚ supplementation with vitamin B6‚ a cofactor for the histidase enzyme‚ may be recommended to aid in histidine breakdown. Vitamin B6 therapy can help normalize histidine levels in the blood and urine‚ potentially alleviating symptoms associated with Histidinuria.
Additionally‚ close monitoring of renal function is essential to detect any early signs of kidney involvement and prevent progressive renal damage. Regular follow-up appointments with healthcare providers‚ including urine tests and kidney function assessments‚ can help in assessing the effectiveness of treatment and managing potential complications.
Behavioral interventions and supportive therapies may be recommended to address the neurological symptoms associated with Histidinuria‚ such as developmental delays and behavioral issues. Early intervention and multidisciplinary care involving specialists in genetics‚ nephrology‚ and neurology can optimize outcomes for individuals with Histidinuria.
Overall‚ a comprehensive and individualized treatment approach is essential in managing Histidinuria effectively. By implementing a combination of dietary management‚ vitamin supplementation‚ renal function monitoring‚ and neurological support‚ healthcare providers can help individuals with Histidinuria lead healthier lives and minimize the impact of this rare genetic disorder on their overall well-being.
Monitoring and Follow-Up
Monitoring and follow-up care are crucial components of managing Histidinuria renal tubular defect syndrome to ensure optimal outcomes for affected individuals. Regular monitoring allows healthcare providers to track the progression of the disorder‚ assess treatment effectiveness‚ and detect any emerging complications in a timely manner.
Individuals diagnosed with Histidinuria require ongoing monitoring of renal function through periodic laboratory tests that evaluate kidney health‚ electrolyte balance‚ and histidine levels in the urine. Monitoring renal function is essential to identify any signs of renal damage early on and intervene promptly to prevent further complications.
In addition to renal function assessments‚ regular follow-up appointments with a multidisciplinary healthcare team are recommended to monitor the progression of neurological symptoms‚ assess developmental milestones‚ and address any behavioral concerns. Neurological evaluations and developmental screenings can help guide intervention strategies to support optimal cognitive and behavioral development.
Diagnostic imaging studies‚ such as kidney ultrasounds‚ may be performed during follow-up visits to evaluate the structural integrity of the kidneys and monitor for any changes indicative of renal complications. These imaging studies provide valuable information for assessing the impact of Histidinuria on renal health and guiding treatment decisions.
Through consistent monitoring and follow-up care‚ healthcare providers can tailor treatment approaches‚ adjust management strategies as needed‚ and provide ongoing support to individuals with Histidinuria. By implementing a comprehensive monitoring plan and ensuring regular follow-up visits‚ healthcare teams can optimize outcomes and improve the overall quality of life for individuals living with Histidinuria renal tubular defect syndrome.
Genetic Basis of Histidinuria
Histidinuria renal tubular defect syndrome is attributed to genetic mutations affecting the histidase enzyme‚ encoded by the HAL gene. Histidase is essential for the breakdown of histidine‚ a process critical for maintaining amino acid balance in the body. Mutations in the HAL gene lead to reduced or absent histidase activity‚ resulting in histidine accumulation and impaired metabolism.
The inheritance pattern of Histidinuria is typically autosomal recessive‚ meaning that individuals must inherit two copies of the mutated gene – one from each parent – to manifest the disorder. Carriers of a single mutated gene are usually asymptomatic but can pass the genetic anomaly to their offspring.
Genetic testing plays a pivotal role in diagnosing Histidinuria and identifying specific mutations in the HAL gene. By sequencing the individual’s DNA‚ healthcare providers can pinpoint the genetic alterations responsible for histidase deficiency‚ confirming the diagnosis of Histidinuria and elucidating the inherited nature of the disorder.
Understanding the genetic basis of Histidinuria is fundamental for personalized treatment approaches and genetic counseling. By uncovering the specific genetic mutations present in affected individuals‚ healthcare providers can tailor management strategies to address the underlying cause of the disorder and provide targeted interventions to mitigate symptoms and complications.
Advancements in genetic research hold promise for enhancing our understanding of Histidinuria at the molecular level‚ paving the way for innovative therapeutic approaches and precision medicine strategies aimed at correcting genetic defects and optimizing outcomes for individuals affected by this rare genetic disorder.
Preventive Measures
Preventive measures for Histidinuria renal tubular defect syndrome focus on early detection‚ genetic counseling‚ and lifestyle modifications to manage the disorder and reduce the risk of complications. Genetic counseling is essential for individuals with a family history of Histidinuria to assess the risk of passing the genetic mutation to their offspring.
Early diagnosis of Histidinuria through newborn screening programs allows for prompt intervention and management of the condition. Screening tests can detect elevated levels of histidine in the blood or urine‚ enabling healthcare providers to initiate treatment strategies early in life‚ potentially mitigating the impact of histidine accumulation on organ systems.
Educating individuals with Histidinuria and their families on dietary modifications to limit histidine intake can help reduce the burden on histidine metabolism and minimize the accumulation of histidine in the body. Monitoring renal function regularly and adhering to recommended treatment plans are essential preventive measures to safeguard kidney health and overall well-being.
Genetic testing for family members of individuals diagnosed with Histidinuria can identify carriers of the mutated gene‚ enabling informed family planning decisions and genetic counseling. By identifying carriers and at-risk individuals‚ healthcare providers can offer guidance on preventive measures and early intervention strategies to manage the risk of passing on the genetic mutation.
By implementing a comprehensive approach that includes genetic counseling‚ early detection‚ dietary modifications‚ and regular monitoring‚ healthcare providers can effectively prevent complications associated with Histidinuria and improve the long-term outcomes for affected individuals. Preventive measures play a crucial role in managing Histidinuria renal tubular defect syndrome and promoting the well-being of individuals living with this rare genetic disorder.
Prognosis and Outcome
The prognosis for individuals with Histidinuria renal tubular defect syndrome varies depending on the severity of the condition‚ early detection‚ and the effectiveness of management strategies employed. With timely diagnosis and appropriate treatment‚ many individuals with Histidinuria can lead relatively healthy lives with minimized symptoms and complications.
Early intervention plays a critical role in improving the long-term outcomes for individuals with Histidinuria. Initiating dietary modifications‚ vitamin B6 supplementation‚ and regular monitoring of renal function can help prevent the progression of renal complications and neurological manifestations associated with the disorder.
Proper management of Histidinuria can significantly impact the overall prognosis and quality of life for affected individuals. By carefully monitoring renal function‚ addressing behavioral and developmental concerns‚ and ensuring adherence to treatment plans‚ healthcare providers can optimize outcomes and promote the well-being of individuals living with Histidinuria.
While Histidinuria is a lifelong condition‚ proactive medical care and ongoing support can help individuals effectively manage the disorder and reduce the risk of complications over time. With advancements in genetic research and personalized medicine‚ the outlook for individuals with Histidinuria continues to improve‚ offering hope for enhanced management strategies and better long-term outcomes.
By providing comprehensive care‚ genetic counseling‚ and access to specialized medical services‚ healthcare providers can empower individuals with Histidinuria to navigate their condition effectively‚ optimize their health outcomes‚ and live fulfilling lives despite the challenges posed by this rare genetic disorder.
Research and Future Directions
Ongoing research endeavors in the field of Histidinuria renal tubular defect syndrome aim to deepen our understanding of the genetic‚ metabolic‚ and clinical aspects of the disorder. Researchers are exploring novel diagnostic techniques‚ treatment modalities‚ and preventive strategies to enhance the management of Histidinuria and improve outcomes for affected individuals.
Genetic studies focused on identifying additional mutations in the HAL gene responsible for histidase deficiency are essential for expanding our knowledge of the genetic basis of Histidinuria. Understanding the diverse genetic landscape of the disorder can guide the development of targeted therapies and personalized treatment approaches.
Metabolic studies investigating the impact of histidine accumulation on various organ systems and metabolic pathways are key to elucidating the disease mechanisms underlying Histidinuria. By unraveling the metabolic alterations associated with the disorder‚ researchers can identify new therapeutic targets and innovative interventions to address the metabolic imbalances linked to Histidinuria.
Clinical trials evaluating the efficacy of new treatment options‚ such as novel pharmaceutical agents or gene therapy approaches‚ hold promise for revolutionizing the management of Histidinuria. Advancements in precision medicine and personalized treatment regimens are paving the way for more tailored and effective interventions for individuals with Histidinuria.
Future directions in Histidinuria research include the exploration of gene editing technologies‚ the development of biomarkers for disease monitoring‚ and the expansion of newborn screening programs to facilitate early detection and intervention. By fostering collaboration among researchers‚ healthcare providers‚ and affected individuals‚ the field of Histidinuria research is poised to drive innovation and improve the outlook for individuals living with this rare genetic disorder.
In conclusion‚ Histidinuria renal tubular defect syndrome is a rare genetic disorder characterized by histidase enzyme deficiency‚ leading to the impaired metabolism of histidine and its accumulation in the blood and urine. The complex interplay between genetic mutations‚ metabolic abnormalities‚ and renal dysfunction underscores the multifaceted nature of this condition.
Effective management of Histidinuria necessitates a holistic approach that includes early detection‚ genetic counseling‚ dietary modifications‚ vitamin supplementation‚ and regular monitoring of renal function. By addressing the underlying genetic anomalies and metabolic imbalances associated with Histidinuria‚ healthcare providers can mitigate the risk of complications and optimize outcomes for affected individuals.
Research efforts in Histidinuria are pivotal for advancing our knowledge of the disorder‚ improving diagnostic techniques‚ and exploring innovative treatment strategies. The ongoing exploration of genetic‚ metabolic‚ and clinical aspects of Histidinuria holds promise for enhancing therapeutic approaches and ultimately enhancing the quality of life for individuals with this rare genetic disorder.
By fostering collaboration between researchers‚ healthcare professionals‚ and individuals living with Histidinuria‚ we can drive progress in the field‚ refine management protocols‚ and pave the way for a brighter outlook for those affected by this condition. Through continued research‚ clinical advancements‚ and personalized care‚ we can strive towards better outcomes and improved well-being for individuals facing the challenges of Histidinuria renal tubular defect syndrome.