Symptoms of Acute Articular Rheumatism
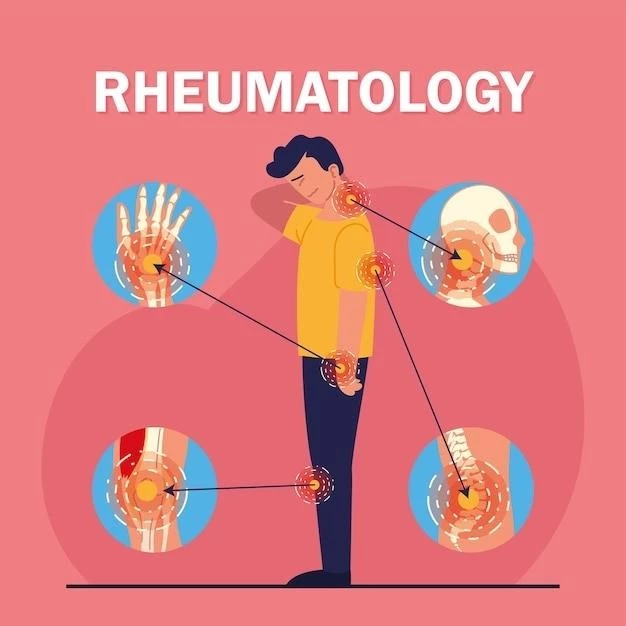
Acute articular rheumatism presents through joint pain,
swelling, fever, chills, fatigue, and weakness.
Joint Pain and Swelling
One of the hallmark symptoms of acute articular rheumatism is severe joint pain accompanied by swelling. The affected joints may feel warm to the touch and appear red due to inflammation.
Fever and Chills
In acute articular rheumatism, patients often experience fever and chills as the body responds to the inflammatory processes affecting the joints. These systemic symptoms accompany the localized joint pain and swelling.
Fatigue and Weakness
Patients with acute articular rheumatism commonly report feelings of fatigue and weakness, which can be debilitating. These symptoms may result from the body’s immune response to the inflammation in the joints.
Causes of Acute Articular Rheumatism
Bacterial infection, genetic predisposition, and autoimmune response.
Bacterial Infection (Typically Streptococcus)
An acute articular rheumatism may be triggered by a bacterial infection, with Streptococcus being a common culprit. The body’s immune response to the infection can lead to joint inflammation and the onset of symptoms.
Genetic Predisposition
Individuals with a genetic predisposition may be more susceptible to developing acute articular rheumatism. Certain gene variations can influence the immune response and increase the risk of inflammatory joint conditions.
Autoimmune Response
Acute articular rheumatism can result from an autoimmune response, where the immune system mistakenly attacks the joints, causing inflammation and pain. This inappropriate immune reaction contributes to the development of the condition.
Treatment Options for Acute Articular Rheumatism
Antibiotics, NSAIDs, and corticosteroids.
Antibiotics
Antibiotics are commonly prescribed to treat acute articular rheumatism caused by bacterial infections, such as Streptococcus. They help eradicate the underlying infection and prevent further joint damage and complications.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are often recommended to manage pain and reduce inflammation in acute articular rheumatism. These medications help alleviate symptoms by targeting the inflammatory processes in the joints, improving comfort and mobility for patients.
Corticosteroids
Corticosteroids are prescribed in cases where NSAIDs alone are not effective in managing acute articular rheumatism. These powerful anti-inflammatory drugs help reduce joint swelling and pain, improving the overall symptoms and quality of life for patients.
Diagnosis of Acute Articular Rheumatism
Physical Examination, Medical History Review, Laboratory Tests.
Physical Examination
A thorough physical exam is crucial in diagnosing acute articular rheumatism; Healthcare providers assess joint tenderness, swelling, and range of motion to identify signs of inflammation. This evaluation aids in determining the appropriate treatment and management plan for the condition.
Medical History Review
Reviewing the patient’s medical history is essential in diagnosing acute articular rheumatism. Important factors such as previous infections, family history of autoimmune disorders, and overall health help healthcare providers understand the context of the condition and tailor the treatment approach accordingly.
Laboratory Tests (Blood tests, Joint fluid analysis)
Diagnostic laboratory tests, including blood tests to assess inflammatory markers and joint fluid analysis to detect signs of infection or inflammation, play a vital role in confirming the presence of acute articular rheumatism and guiding treatment decisions based on the specific findings.
Management of Acute Articular Rheumatism
Rest and Joint Protection, Physical Therapy, Occupational Therapy.
Rest and Joint Protection
Rest and proper joint protection are essential in managing acute articular rheumatism. Adequate rest helps reduce inflammation and pain, while protecting the affected joints from excessive strain and injury promotes healing and prevents further damage to the joint structures.
Physical Therapy
Physical therapy plays a crucial role in the management of acute articular rheumatism. Tailored exercises and interventions help improve joint flexibility, strength, and function. Physical therapists assist patients in regaining mobility, reducing pain, and enhancing their overall quality of life.
Occupational Therapy
Occupational therapy is beneficial in managing acute articular rheumatism by focusing on optimizing the performance of daily activities. Therapists provide strategies and assistive devices to help individuals with joint pain maintain independence and functionality in their personal and work-related tasks.
Lifestyle Changes for Acute Articular Rheumatism
Healthy Diet and Weight Management, Regular Exercise, Stress Management Techniques.
Healthy Diet and Weight Management
A nutritious diet and weight management are vital for managing acute articular rheumatism. Maintaining a healthy weight reduces stress on the joints, while a balanced diet rich in anti-inflammatory foods can help reduce inflammation and improve overall joint health.
Regular Exercise
Engaging in regular exercise is beneficial for individuals with acute articular rheumatism. Low-impact activities, such as swimming or tai chi, can help improve joint flexibility, strengthen muscles, and reduce pain. Customized exercise regimens are designed to enhance mobility and overall well-being.
Stress Management Techniques
Effective stress management techniques play a crucial role in the management of acute articular rheumatism. Strategies such as mindfulness, meditation, and relaxation exercises can help reduce stress levels, which in turn may alleviate pain and improve the overall quality of life for individuals with this condition.
Complications of Acute Articular Rheumatism
Joint Deformities, Heart Inflammation, Neurological Issues.
Joint Deformities
Acute articular rheumatism can lead to severe joint deformities if left untreated. Inflammation and damage to the joint structures may cause joint misalignment and functional impairment, impacting the individual’s mobility and quality of life.
Heart Inflammation (Endocarditis)
In some cases, acute articular rheumatism can lead to heart inflammation, specifically endocarditis. The inflammation affects the heart’s inner lining, potentially causing complications such as heart valve damage and affecting cardiac function. Monitoring and prompt treatment are crucial to prevent serious cardiac issues.
Neurological Issues
Acute articular rheumatism may result in neurological complications. Inflammation in the joints can trigger nerve irritation or compression, leading to symptoms such as pain, numbness, or weakness in the affected areas. Timely intervention and appropriate management are crucial to address potential neurological issues associated with the condition.
Research and Developments in Acute Articular Rheumatism
New Antibiotics and Treatment Approaches, Advances in Understanding Autoimmune Mechanisms, Exploration of Novel Therapeutic Targets.
New Antibiotics and Treatment Approaches
Ongoing research focuses on developing new antibiotics and innovative treatment approaches for acute articular rheumatism. These advancements aim to enhance the efficacy of antibiotic therapy and introduce novel strategies to target the underlying causes of the condition effectively.
Advances in Understanding Autoimmune Mechanisms
Current research is making progress in elucidating the complex autoimmune mechanisms involved in acute articular rheumatism. Enhanced understanding of how the immune system reacts inappropriately to joint tissues is crucial for developing targeted therapies to modulate the immune response and alleviate symptoms effectively.
Exploration of Novel Therapeutic Targets
Researchers are exploring novel therapeutic targets for treating acute articular rheumatism. This exploration involves identifying specific molecules and pathways that can be targeted with new medications to improve outcomes and provide more effective and personalized treatment options for patients with this condition.
