Article Plan⁚ Disease ー Xeroderma Talipes Enamel Defects
Introduction to Xeroderma Talipes Enamel Defects
Xeroderma Talipes Enamel Defects, often referred to as XTE syndrome, is a condition that affects enamel development and can lead to various dental issues. Enamel formation in humans involves a complex process regulated by numerous genes. The condition is closely related to Xeroderma Pigmentosum, a rare genetic disorder that affects the skin’s reaction to sunlight.
Individuals with XTE syndrome may present with enamel defects, which can cause challenges in oral health. These defects are sometimes associated with other syndromes, highlighting the complexity of genetic conditions affecting dental structures. Understanding the diagnostic criteria for Xeroderma Talipes Enamel Defects is essential for accurate identification and management.
Managing and treating XTE syndrome involves addressing the specific dental complications associated with enamel defects. These complications can impact oral health significantly, necessitating tailored treatment approaches for affected individuals. Research advances in enamel defects treatment offer hope for improved management strategies in the future.
Exploring the genetic basis of XTE syndrome provides insights into the inheritance patterns and mechanisms underlying this condition. Recognizing complications associated with Xeroderma Talipes Enamel Defects is crucial for comprehensive care and early intervention to prevent further oral health issues.
Enamel defects resulting from disturbances during tooth formation can have lasting effects on dental health. These defects can manifest as changes in enamel thickness or mineralization, affecting the integrity of the tooth structure. Understanding the impact of enamel defects on oral health is vital for promoting effective preventive measures and treatment strategies.
As ongoing research continues to advance our understanding of enamel defects and associated syndromes, future directions in managing Xeroderma Talipes Enamel Defects hold promise for improved outcomes and quality of life for individuals affected by this condition.
Understanding Enamel Development
Human enamel formation is a sophisticated process governed by the activity of numerous genes and intricate molecular mechanisms. This process involves cell differentiation, the production of a unique extracellular matrix, and the regulation of various cellular functions at different stages of enamel development.
Defects in enamel development, such as those seen in Xeroderma Talipes Enamel Defects, can arise from disturbances during tooth formation. These defects may manifest as quantitative issues like hypoplasia, which affects enamel thickness, or qualitative problems like hypomineralization, leading to opacity in the enamel structure.
The genetic basis of enamel defects, like XTE syndrome, sheds light on the inheritance patterns and genetic variations contributing to these conditions. Understanding the molecular pathways involved in enamel formation is crucial for identifying the underlying mechanisms responsible for enamel abnormalities.
Enamel defects are classified into various types, including demarcated opacity, diffuse opacity, and hypoplasia. These defects can impact the translucency and mineralization of enamel, resulting in structural abnormalities that affect dental health.
Recognizing the complexities of enamel development and the factors influencing enamel defects is essential for implementing preventive measures and treatment strategies. By staying informed about the latest research and advancements in this field, dental professionals can enhance their approach to managing enamel defects effectively.
Overview of Xeroderma Pigmentosum
Xeroderma Pigmentosum (XP) is a rare autosomal recessive genodermatosis characterized by extreme photosensitivity, skin pigmentary changes, malignant tumor development, and sometimes progressive neurologic degeneration. This condition results from mutations in nucleotide excision repair mechanisms, impacting the skin’s reaction to sunlight.
Individuals with XP have a significantly heightened sensitivity to sunlight exposure, leading to severe sunburn, alterations in skin pigmentation, and a substantially increased risk of developing various types of skin cancers. The disease affects approximately 1 in a million individuals in the United States, emphasizing its rarity and the need for proper management strategies.
The incidence of Xeroderma Pigmentosum underscores the importance of sun protection and vigilant skin care practices for affected individuals to mitigate the risk of skin damage and malignancies. Understanding the genetic basis of XP is crucial for providing accurate diagnoses and tailored treatment plans to improve patient outcomes and quality of life.
As a complex genetic disorder, Xeroderma Pigmentosum requires comprehensive medical attention to address both the dermatologic manifestations and potential neurological complications associated with the condition. Collaborative care involving dermatologists, oncologists, and neurologists is vital for managing XP effectively and minimizing its impact on overall health.
Advances in genetic research and precision medicine offer promising avenues for the diagnosis and treatment of Xeroderma Pigmentosum, highlighting the ongoing efforts to improve patient care and enhance our understanding of this rare and challenging condition.
Literature Review on Enamel Defects
A comprehensive literature review reveals a focus on conditions associated with defects in enamel, highlighting the complexity of dental abnormalities in various syndromes. Studies have investigated the genetic underpinnings of enamel defects like those observed in XTE syndrome, emphasizing the importance of understanding the intricate molecular mechanisms involved in enamel formation.
Researchers have explored the classification of enamel defects into different types, including demarcated opacity, diffuse opacity, and hypoplasia, each contributing to structural abnormalities in dental enamel. Studies by Witkop, Rao, Moynahan, and others have provided valuable insights into the clinical manifestations and genetic basis of enamel abnormalities.
Notable research by Hoff, Van Grunsven, Tonglebloed, and Gravenmade has examined enamel defects associated with specific syndromes like tuberous sclerosis, further elucidating the diverse etiologies of enamel abnormalities in various genetic conditions. Understanding the distinct presentations of enamel defects is essential for accurate diagnosis and tailored treatment approaches.
Case studies focusing on conditions such as XTE syndrome have contributed to the characterization of enamel defects in the context of broader genetic syndromes, highlighting the interplay between genetic variations and dental manifestations. The literature underscores the significance of early identification and management of enamel defects to mitigate their impact on oral health.
Advancements in genetic research and syndromic evaluations have expanded our knowledge of enamel defects, paving the way for personalized treatment strategies and improved patient outcomes. By synthesizing findings from diverse literature sources, healthcare providers can enhance their understanding of enamel abnormalities and refine management approaches for individuals with complex dental conditions.
Specific Case Studies on XTE Syndrome
Case studies on XTE syndrome, also known as Xeroderma Talipes Enamel Defects, provide valuable insights into the clinical manifestations and genetic basis of this condition. Moynahan’s research in 1970 described XTE syndrome as a heredo-familial condition characterized by xeroderma٫ talipes٫ and enamel defects. Investigations into XTE syndrome have revealed homozygous inheritance of a dominant gene in affected individuals.
Studies by Witkop, Rao, and Sauk reviewed conditions related to enamel defects but did not find XTE syndrome mentioned, indicating the rarity and distinctive nature of this syndrome. However, Moynahan’s work highlighted two cases of XTE syndrome, emphasizing the need for further research and understanding of this genetic disorder.
Researchers have linked XTE syndrome to clubfoot, demonstrating a unique combination of symptoms that distinguish it from other syndromes. By examining specific cases and genetic inheritance patterns, healthcare professionals can better diagnose and manage individuals with XTE syndrome, improving overall patient care and outcomes.
The clinical presentation of XTE syndrome involves a complex interplay of genetic factors influencing the development of enamel defects, showcasing the intricate nature of this condition. Understanding the distinct features and genetic implications of XTE syndrome is crucial for accurate diagnosis, personalized treatment plans, and effective management of individuals affected by this rare genetic disorder.
Association of Enamel Defects with Other Syndromes
Enamel defects are often linked to various genetic syndromes, showcasing the intricate interplay between molecular pathways and dental abnormalities. Research by Moynahan in 1970 highlighted the unique XTE syndrome, which combines xeroderma, talipes, and enamel defects, emphasizing the need for further exploration of this hereditary condition.
Studies by Witkop, Rao, Sauk, Hoff, Van Grunsven, and Tonglebloed have delved into enamel abnormalities in syndromes like tuberous sclerosis, shedding light on the diverse etiologies of enamel defects in different genetic conditions. Understanding the association between specific syndromes and enamel defects is crucial for accurate diagnosis and tailored treatment strategies.
The correlation between XTE syndrome and clubfoot further demonstrates the complexity of symptoms in genetic disorders involving enamel defects. By investigating specific case studies and genetic inheritance patterns, healthcare providers can enhance their ability to recognize and manage syndromes characterized by enamel abnormalities, improving patient care outcomes.
Exploring genetic syndromes such as XTE syndrome and understanding their association with enamel defects is essential for comprehensive patient care and effective treatment planning. By staying informed about the latest research and advancements in enamel abnormalities linked to syndromes, healthcare professionals can enhance their approach to diagnosing and managing these complex genetic conditions.
Diagnostic Criteria for Xeroderma Talipes Enamel Defects
Diagnosing Xeroderma Talipes Enamel Defects involves a comprehensive assessment of clinical manifestations, genetic history, and dental abnormalities. Physicians typically look for a combination of xeroderma (extreme dry skin), talipes (clubfoot deformity), and distinct enamel defects in affected individuals. The presence of these characteristic features, along with a detailed family history, can aid in the accurate diagnosis of XTE syndrome.
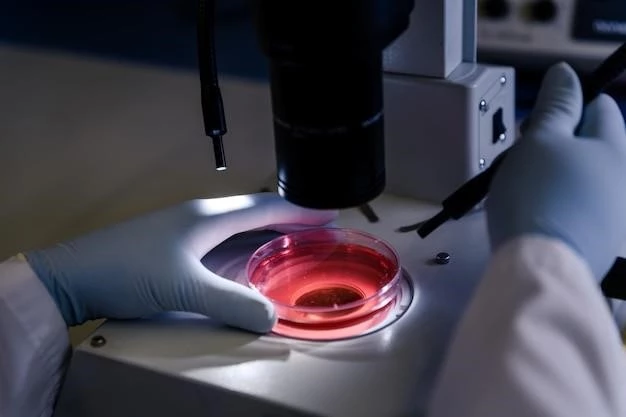
Genetic testing plays a significant role in confirming the diagnosis of Xeroderma Talipes Enamel Defects, as identifying specific gene mutations associated with the condition is crucial for definitive diagnosis and genetic counseling. Additionally, assessing dental X-rays for enamel abnormalities, conducting thorough physical examinations, and collaborating with dental specialists can contribute to a comprehensive diagnostic evaluation.
Given the rarity of XTE syndrome, healthcare providers must maintain a high index of suspicion when encountering individuals with suggestive symptoms. Consultation with geneticists and dermatologists can further support the diagnostic process by integrating multidisciplinary expertise and advanced genetic testing methodologies.
Continuous monitoring of individuals diagnosed with Xeroderma Talipes Enamel Defects is essential to track disease progression, assess dental health, and implement appropriate management strategies. Regular follow-up visits, genetic counseling, and dental interventions can help optimize patient care and improve long-term outcomes for individuals affected by this uncommon genetic disorder.
Management and Treatment Approaches
Managing Xeroderma Talipes Enamel Defects requires a multidisciplinary approach involving dermatologists, geneticists, and dental specialists to address the diverse manifestations of this rare genetic disorder. Treatment strategies focus on minimizing sun exposure to reduce skin damage, regular skin examinations to detect early malignancies, and neurologic evaluations for potential degenerative complications.
Dental care for enamel defects in XTE syndrome involves customized approaches such as fluoride treatments, dental fillings, and enamel sealing to enhance enamel integrity and prevent dental caries. Regular dental check-ups are essential to monitor enamel health and address emerging issues promptly.
Genetic counseling plays a crucial role in managing Xeroderma Talipes Enamel Defects by providing families with information on inheritance patterns, genetic testing options, and potential risks for future generations. Educating patients on sun protection measures and skin surveillance practices is vital for early detection of skin cancers.
Individualized treatment plans for XTE syndrome may include skin protection strategies like sunscreen use, protective clothing, and regular screenings for skin malignancies. Neurological assessments and supportive therapies are essential for addressing potential neurologic complications in affected individuals.
Ongoing research into Xeroderma Talipes Enamel Defects aims to explore novel treatment modalities, genetic therapies, and precision medicine approaches to improve patient outcomes and enhance quality of life. Collaborative efforts between healthcare professionals and researchers are essential for advancing knowledge and developing innovative management strategies for this complex genetic condition.
Genetic Basis of XTE Syndrome
XTE syndrome, formally known as Xeroderma Talipes Enamel Defects, is a rare genetic disorder characterized by the co-occurrence of xeroderma, talipes (clubfoot deformity), and enamel defects. This heredo-familial syndrome involves homozygous inheritance of a dominant gene, contributing to the distinctive combination of clinical features observed in affected individuals.
The intricate molecular mechanisms governing human enamel formation involve the activity of numerous genes responsible for cell differentiation, extracellular matrix production, and cellular function modulation during enamel development. Mutations in these genes can disrupt the intricate processes, leading to enamel defects like those seen in XTE syndrome.
Studies by Moynahan in 1970 first described XTE syndrome, highlighting the need for further research and understanding of this unique genetic condition. The rarity of XTE syndrome underscores the importance of genetic testing to confirm the diagnosis and identify specific gene mutations associated with the disorder.
Genetic research plays a pivotal role in unraveling the underlying mechanisms of XTE syndrome and elucidating the genetic basis of this complex condition. By advancing our understanding of the genetic factors contributing to Xeroderma Talipes Enamel Defects, researchers aim to enhance diagnostic accuracy, genetic counseling, and personalized treatment strategies for individuals affected by this rare syndrome.
Complications Associated with Xeroderma Talipes Enamel Defects
Individuals with Xeroderma Talipes Enamel Defects may experience a range of complications related to this rare genetic disorder. The condition, characterized by xeroderma, talipes, and enamel defects, poses challenges that warrant comprehensive management strategies.
Common complications include extreme photosensitivity due to xeroderma, requiring strict sun protection measures to prevent sunburn and reduce the risk of skin malignancies. Enamel defects associated with XTE syndrome can lead to dental caries, enamel hypoplasia, and aesthetic concerns, necessitating specialized dental care.
In some cases, Xeroderma Talipes Enamel Defects may be accompanied by neurological degeneration, highlighting the complexity of this genetic condition. Neurologic complications can manifest progressively and affect motor function, cognition, and sensory processing, emphasizing the need for thorough monitoring and intervention.
Managing the complications of XTE syndrome involves a multidisciplinary approach, including dermatologists, dental professionals, neurologists, and geneticists. Collaborative care aims to address the diverse challenges associated with Xeroderma Talipes Enamel Defects comprehensively, enhancing quality of life and minimizing the impact of complications on individuals affected by this rare syndrome.
Impact of Enamel Defects on Oral Health
Enamel defects, such as those observed in Xeroderma Talipes Enamel Defects, can have a significant impact on oral health. These defects, resulting from disturbances in tooth development, may lead to structural abnormalities affecting the integrity of the enamel. Understanding the implications of enamel defects is crucial for promoting optimal dental care.
The presence of enamel defects can increase the risk of dental caries, as the compromised enamel may be more susceptible to decay. Individuals with XTE syndrome may experience challenges in maintaining proper oral hygiene and addressing dental issues effectively, underscoring the importance of specialized dental management.
Enamel defects can also affect the aesthetic appearance of the teeth, causing changes in enamel thickness, translucency, or mineralization. These alterations may impact self-esteem and confidence, highlighting the psychosocial impact of dental abnormalities associated with Xeroderma Talipes Enamel Defects.
Regular dental examinations, preventive measures like fluoride treatments, and targeted interventions can help mitigate the consequences of enamel defects on oral health. By addressing enamel abnormalities promptly and implementing tailored dental care strategies, individuals with XTE syndrome can maintain better oral health outcomes and overall well-being.
Research Advances in Enamel Defects Treatment
Recent research has focused on advancing treatment strategies for enamel defects like those observed in Xeroderma Talipes Enamel Defects. By exploring novel approaches, researchers aim to enhance the management of dental abnormalities associated with this rare genetic condition.
Innovations in enamel defect treatment include customized dental interventions such as fluoride therapies, dental fillings, and enamel sealing to improve enamel resilience and prevent decay. These tailored approaches address the specific needs of individuals with XTE syndrome, promoting better oral health outcomes.
Genetic therapies and precision medicine have emerged as promising avenues for the treatment of enamel defects linked to genetic conditions like XTE syndrome. By targeting specific genetic mutations and molecular pathways involved in enamel formation, researchers seek to develop personalized treatment modalities for affected individuals.
Collaborative efforts between healthcare professionals, geneticists, and researchers are essential for translating research findings into effective clinical interventions for enamel defects. Ongoing studies aim to refine treatment protocols, enhance diagnostic accuracy, and optimize dental care approaches for individuals with complex genetic conditions affecting enamel development.
By staying informed about the latest research advances in enamel defect treatment, healthcare providers can improve their management strategies, offer better outcomes for patients with Xeroderma Talipes Enamel Defects, and contribute to the ongoing progress in addressing the dental challenges associated with this rare genetic disorder.
Future Directions in Managing Xeroderma Talipes Enamel Defects
Future directions in managing Xeroderma Talipes Enamel Defects aim to integrate cutting-edge research findings into clinical practice for enhanced patient care. By leveraging genetic therapies, precision medicine, and innovative treatment modalities, healthcare providers can tailor interventions to the specific needs of individuals with XTE syndrome.
Advancements in genetic testing methodologies will enable precise identification of gene mutations associated with Xeroderma Talipes Enamel Defects, facilitating early diagnosis and personalized treatment approaches. Genetic counseling services will play an integral role in providing families with comprehensive information on inheritance patterns and genetic risk factors.
Collaborative efforts among physicians, geneticists, dental specialists, and researchers will drive interdisciplinary approaches to managing XTE syndrome, improving diagnostic accuracy and therapeutic outcomes. Continuous monitoring and follow-up care will be vital for tracking disease progression and ensuring timely interventions.
Research endeavors will focus on refining enamel defect treatment protocols, optimizing preventive measures, and exploring novel therapeutic targets to address the complexities of this rare genetic disorder. By staying at the forefront of research advances, healthcare professionals can enhance their ability to deliver comprehensive care and support to individuals affected by Xeroderma Talipes Enamel Defects.
