Article Plan⁚ Disease ⎼ Organophosphate Poisoning
Introduction to Organophosphate Poisoning
Organophosphate poisoning is a serious health concern caused by exposure to pesticides, herbicides, and nerve agents. It remains a frequent reason for hospital admissions, particularly in developing countries. This poisoning leads to diverse symptoms due to its effects on different receptors in the body, such as muscarinic, nicotinic, and central nervous system receptors.
Self-poisoning with organophosphorus pesticides is a significant issue, resulting in a high number of fatalities annually, especially in rural regions of developing countries. Swift medical management is crucial, with case fatality rates often exceeding 15%, emphasizing the importance of timely intervention and treatment.
Organophosphate compounds, found in insecticides, medications, and nerve agents, inhibit acetylcholinesterase, resulting in symptoms like increased saliva, vomiting, muscle tremors, and confusion. It is imperative to recognize the early signs of poisoning to prevent severe complications and ensure the timely administration of appropriate treatments.
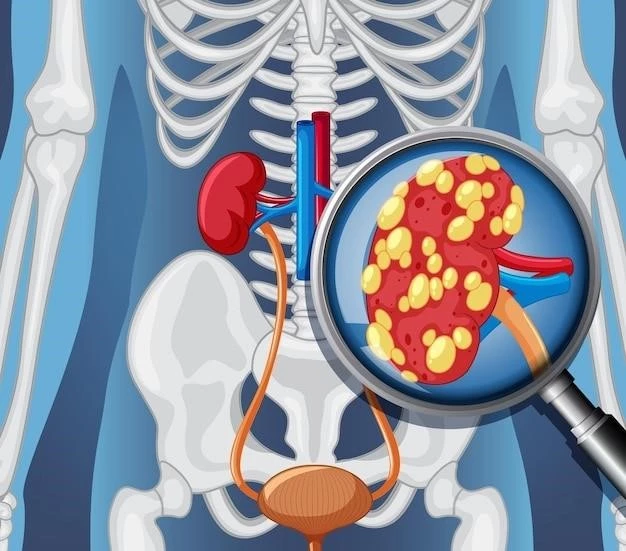
Diagnosis of organophosphate poisoning involves measuring cholinesterase activity, and treatment typically begins with decontamination and airway control. The incidence of organophosphate poisoning is significant, with millions of people exposed globally. Awareness of preventive measures and early management strategies is crucial to reduce the impact of this poisoning worldwide.
The research on promising treatments, including catalytic bioscavengers, shows potential for improved outcomes in cases of organophosphate poisoning. With millions exposed to these toxic agents annually, understanding the causes, symptoms, diagnosis, and treatment options for organophosphate poisoning is essential for medical professionals and the general public alike.
Causes and Risk Factors
Organophosphate poisoning is primarily caused by exposure to organophosphate pesticides, herbicides, and nerve agents either through dermal contact, inhalation, or ingestion. These toxic compounds inhibit acetylcholinesterase, leading to the accumulation of acetylcholine at nerve synapses and overstimulation of cholinergic receptors.
Individuals at higher risk of organophosphate poisoning include agricultural workers who handle pesticides, individuals living in areas where organophosphate pesticides are heavily used, and those with intentional exposure due to self-harm. It’s essential to handle these chemicals with great caution and follow safety protocols to minimize the risk of poisoning.
Common organophosphate compounds like malathion, parathion, chlorpyrifos, and others are widely used in agriculture, pest control, and industrial settings, increasing the likelihood of accidental exposure. Additionally, nerve agents such as sarin and tabun pose a severe risk in situations of deliberate chemical warfare or terrorism.
Preventive measures like using protective gear when handling organophosphate compounds, proper storage of pesticides, and implementing safety protocols in pesticide use can significantly reduce the risk of poisoning. Education on the dangers of organophosphate exposure and promoting safe handling practices are essential in preventing incidents of poisoning.
Symptoms and Clinical Manifestations
Organophosphate poisoning manifests with a range of symptoms stemming from the overstimulation of cholinergic receptors due to acetylcholinesterase inhibition. Early signs often include increased saliva, sweaty skin, and small pupils. As toxicity progresses, individuals may experience muscle tremors, respiratory distress, vomiting, diarrhea, confusion, and even seizures.
The acute cholinergic syndrome characterizes the initial phase of organophosphate poisoning, typically presenting within hours of exposure. Symptoms like excessive salivation, lacrimation, and gastrointestinal distress are common. Intermediate syndrome, appearing days later, may involve weakness, respiratory struggles, and elevated heart rate. Delayed neuropathy is a potential long-term complication post-exposure.
Quick recognition of symptoms, especially in cases of intentional ingestion or occupational exposure, is crucial for prompt medical intervention. Seeking immediate medical attention upon suspicion of organophosphate poisoning can prevent severe complications and improve outcomes. Understanding the diverse clinical manifestations of this poisoning is vital for both healthcare professionals and the general population.
Organophosphate toxicity necessitates specialized care and treatment to address its systemic impact. With millions globally exposed to organophosphates yearly, recognizing the signs and symptoms of poisoning can facilitate early diagnosis and timely treatment, leading to better patient prognosis and reducing the burden of this toxic condition on healthcare systems.
Diagnosis and Confirmation
Diagnosing organophosphate poisoning involves clinical assessment combined with confirming cholinesterase activity levels. Typically, laboratory tests measure cholinesterase activity, although these results may not be immediately available. The diagnostic process plays a critical role in initiating appropriate treatment promptly, enhancing patient outcomes.
Confirmation of organophosphate poisoning can be challenging due to the nonspecific nature of symptoms and the need for specialized testing. Early recognition of clinical signs, such as excessive salivation, muscle tremors, and respiratory distress, coupled with a history of exposure to organophosphate compounds, aids in the diagnosis.
Timely diagnosis is essential in cases of suspected organophosphate poisoning to prevent further complications and tailor treatment strategies effectively. Once diagnosis is confirmed, interventions like decontamination, airway management, and pharmacological therapy can be initiated to address the toxic effects of organophosphate exposure.
Healthcare professionals are advised to maintain a high index of suspicion for organophosphate poisoning, especially in cases of intentional ingestion or occupational exposure. Rapid identification and confirmation of the condition enable clinicians to implement appropriate measures promptly, reducing the risk of adverse outcomes associated with organophosphate toxicity.
Treatment Options
Treating organophosphate poisoning involves a multi-faceted approach aimed at addressing the toxic effects of the compounds. Initially, decontamination procedures are vital to prevent further exposure through dermal contact, inhalation, or ingestion. Prompt airway management and ensuring adequate oxygenation are crucial in stabilizing patients presenting with respiratory distress.
Pharmacological therapy plays a central role in the treatment of organophosphate toxicity. Atropine, an anti-muscarinic agent, is commonly used to counteract the muscarinic effects induced by acetylcholinesterase inhibition. Pralidoxime, an oxime compound, is employed to reactivate inhibited acetylcholinesterase, aiding in restoring normal neuromuscular function.
Activated charcoal may be administered to limit the absorption of ingested organophosphates in cases of oral exposure. Supportive care, including the management of seizures and maintaining fluid balance, is essential to ensure optimal patient outcomes. Close monitoring of vital signs and neurological status is critical throughout the treatment process.
For severe cases of organophosphate poisoning, especially those resulting from intentional ingestion or occupational exposure, intensive care management may be necessary. Specialized facilities equipped to provide ventilatory support, continuous monitoring, and advanced pharmacological interventions can significantly improve patient prognosis.
Educating individuals at risk of organophosphate exposure on preventive measures and the importance of prompt medical attention in case of suspected poisoning is fundamental in reducing morbidity and mortality associated with these toxic compounds. Collaborative efforts between healthcare providers, poison control centers, and emergency responders are essential in managing and treating cases of organophosphate poisoning effectively.
Management of Acute Cholinergic Syndrome
Effective management of acute cholinergic syndrome resulting from organophosphate poisoning is crucial in mitigating potentially life-threatening consequences. Early recognition of symptoms, such as excessive salivation, sweating, muscle tremors, and respiratory distress, is paramount for prompt intervention. Healthcare providers should act swiftly to initiate appropriate treatment measures.
The cornerstone of managing acute cholinergic syndrome involves the administration of atropine, an anti-muscarinic agent that counteracts the muscarinic effects caused by acetylcholinesterase inhibition. Atropine helps alleviate symptoms like increased secretions and smooth muscle hyperactivity, restoring a more stable physiological state in affected individuals.
In addition to atropine, the utilization of oxime compounds, such as pralidoxime, aims to reactivate inhibited acetylcholinesterase, facilitating the breakdown of acetylcholine and reducing the overstimulation of cholinergic receptors. This dual-pronged pharmacological approach targets the underlying pathophysiology of organophosphate toxicity, assisting in symptom resolution.
Close monitoring of vital signs, neurological status, and respiratory function is imperative during the management of acute cholinergic syndrome. Intensive care settings may be necessary for severe cases requiring ventilatory support and continuous observation. Collaboration among healthcare team members is vital to ensuring a coordinated and effective management strategy.
Educating individuals on the signs of acute cholinergic syndrome and the importance of seeking immediate medical attention upon suspicion of organophosphate poisoning is essential in enhancing treatment outcomes. By promptly addressing the cholinergic manifestations of organophosphate toxicity, healthcare providers can significantly improve patient prognosis and reduce the associated morbidity and mortality.
Prevention Strategies

Implementing effective prevention strategies is essential to reduce the risks associated with organophosphate poisoning. Proper handling and storage of organophosphate compounds, such as pesticides and nerve agents, are crucial in minimizing accidental exposures. Individuals working with these chemicals should adhere to safety protocols and wear appropriate protective clothing to mitigate dermal contact.
Educating agricultural workers, pest control professionals, and individuals working in industrial settings on the potential hazards of organophosphates is key to fostering awareness and promoting safe practices. Training programs focusing on the correct use of personal protective equipment and adherence to safety guidelines can significantly lower the likelihood of poisoning incidents.
Promoting the safe application of organophosphate pesticides, including following recommended dosages and application methods, can help prevent overexposure and minimize the environmental impact of these chemicals. Implementing integrated pest management practices that incorporate biological control methods can reduce reliance on chemical pesticides, further decreasing the risk of poisoning.
Regular monitoring and maintenance of pesticide equipment, along with appropriate disposal of unused or expired products, contribute to a safer working environment and community; Establishing emergency response protocols and providing training on handling accidental exposures are vital components of prevention efforts to ensure swift and effective responses in case of poisonings. By prioritizing preventive measures, individuals and industries can significantly reduce the incidence of organophosphate poisoning.
Global Impact and Statistics
Organophosphate poisoning has a significant global impact, particularly in developing countries where exposure to pesticides and nerve agents remains prevalent. Self-poisoning with organophosphorus compounds, a common issue in rural areas, results in a substantial number of fatalities annually, emphasizing the urgent need for preventive measures and effective management strategies.
Annually, an estimated 200٫000 individuals succumb to organophosphate pesticide self-poisoning٫ highlighting the severity of this health concern٫ especially in regions like South East Asia٫ China٫ and Africa. Additionally٫ millions are exposed to toxic levels of organophosphates globally٫ leading to numerous hospitalizations and significant healthcare burdens.
The acute cholinergic syndrome resulting from organophosphate toxicity poses a critical health risk, with symptoms manifesting within hours of exposure. Immediate medical attention is crucial to address the diverse clinical manifestations of organophosphate poisoning, ranging from excessive secretions to respiratory distress and neurological complications.
With up to 300٫000 fatalities attributed to organophosphate and carbamate agents each year worldwide٫ the importance of awareness٫ early diagnosis٫ and appropriate treatment cannot be overstated. Collaborative efforts between healthcare systems٫ poison control centers٫ and public health initiatives are essential to combat the impact of organophosphate poisoning on a global scale.
Research and Promising Treatments
Current research on organophosphate poisoning is advancing promising treatments, focusing on innovative strategies to improve patient outcomes. Studies exploring catalytic bioscavengers, including paraoxonase and other organophosphate hydrolases, show potential in effectively neutralizing toxic organophosphates in the body.
Bioscavengers like stoichiometric, catalytic, and pseudocatalytic agents offer different approaches to counteracting organophosphate toxicity. The development of catalytic bioscavengers represents a significant advancement in the field, with these enzymes demonstrating the ability to rapidly hydrolyze and detoxify organophosphates, enhancing treatment efficacy.
Novel therapeutic approaches aim to enhance the body’s ability to degrade organophosphates, reducing their toxic effects and preventing severe complications. By targeting the specific mechanisms of organophosphate poisoning, researchers are seeking to provide more tailored and effective treatments for individuals exposed to these hazardous compounds.
Efforts in pharmacological research are focused on identifying compounds that can efficiently counteract the neurotoxic effects of organophosphates, restoring normal neuromuscular function and minimizing the impact of poisoning. Collaborative initiatives between research institutions, pharmaceutical companies, and healthcare providers are essential in driving forward promising treatments for organophosphate poisoning.