Diaphragmatic Hernia, Exomphalos, Corpus Callosum Agenesis
This article explores the complex conditions of diaphragmatic hernia, exomphalos, and corpus callosum agenesis․ It delves into the medical aspects of each, from birth defects to genetic factors, and discusses the prognosis and long-term care involved․
Introduction
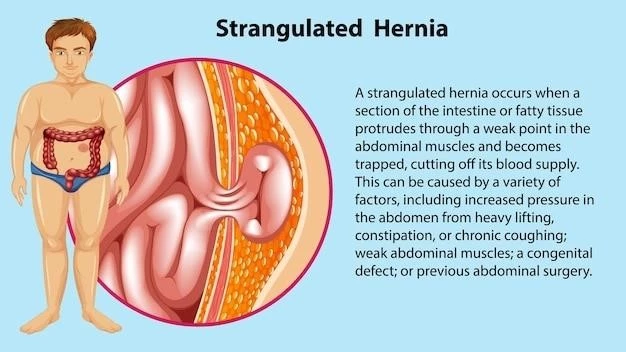
Diaphragmatic hernia, exomphalos, and corpus callosum agenesis are serious congenital anomalies that impact different areas of the body․ Diaphragmatic hernia involves an abdominal wall defect leading to respiratory distress, exomphalos is characterized by the protrusion of abdominal organs, and corpus callosum agenesis refers to a brain malformation affecting cognitive and motor functions․
These conditions can be caused by genetic factors and pose significant challenges for patients and caregivers․ The coexistence of these conditions can complicate medical management and require multidisciplinary care approaches․ Prognosis and long-term care for individuals with these disorders vary based on the severity of symptoms and any associated complications․
Understanding the underlying genetic disorders and medical conditions associated with diaphragmatic hernia, exomphalos, and corpus callosum agenesis is crucial for providing appropriate treatment and support․ Surgical repair may be necessary for addressing abdominal wall defects and other physical abnormalities․ Developmental delays and other long-term consequences may necessitate ongoing medical intervention and therapies to optimize outcomes for affected individuals․
Diaphragmatic Hernia
Diaphragmatic hernia is a birth defect characterized by an abnormal opening in the diaphragm, allowing abdominal organs to move into the chest cavity․ This condition can lead to respiratory distress in newborns due to the compression of the lungs․ The severity of diaphragmatic hernia varies, with some cases being identified prenatally through ultrasound screening․
Medical intervention is often required to stabilize the infant’s condition after birth․ Surgical repair is typically necessary to close the opening in the diaphragm and reposition the abdominal organs properly․ Despite advancements in surgical techniques, infants with diaphragmatic hernia may still face respiratory challenges and require neonatal intensive care․
Long-term care for individuals with diaphragmatic hernia may involve monitoring respiratory function and addressing any developmental delays that could arise․ Genetic factors play a role in the development of diaphragmatic hernia, highlighting the importance of genetic counseling for families affected by this condition․
Managing diaphragmatic hernia requires a collaborative approach involving neonatologists, pediatric surgeons, respiratory therapists, and other healthcare professionals․ The prognosis for individuals with diaphragmatic hernia depends on the severity of the defect, the presence of associated anomalies, and the effectiveness of the treatment provided․
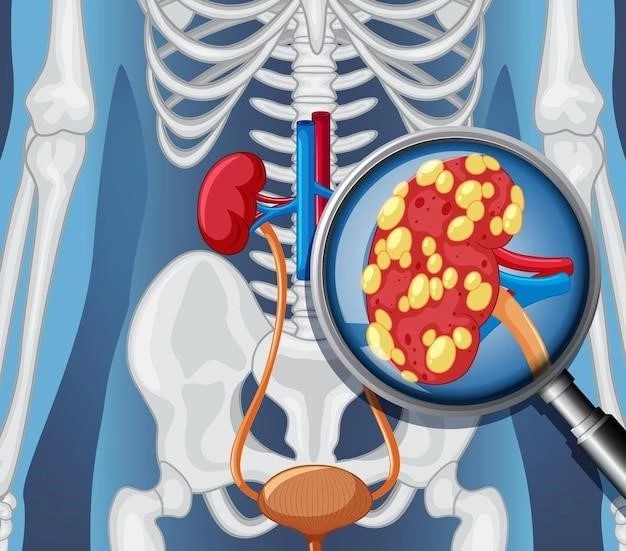
Exomphalos (Abdominal Wall Defect)
Exomphalos, also known as omphalocele, is a congenital anomaly characterized by a defect in the abdominal wall through which abdominal organs protrude․ This condition typically presents as a visible sac at the base of the umbilical cord containing the intestines, liver, or other organs․
Diagnosis of exomphalos can often be made during prenatal ultrasounds․ Newborns with exomphalos may experience feeding difficulties, respiratory challenges, and an increased risk of infection․ Surgical intervention is commonly required to repair the abdominal wall defect and position the organs back into the abdominal cavity․
Genetic factors play a role in the development of exomphalos, and affected individuals may require genetic testing and counseling․ Long-term care for individuals with exomphalos may involve monitoring for abdominal infections, ensuring proper growth and nutrition, and addressing any associated developmental delays․
The prognosis for individuals with exomphalos depends on the size of the abdominal wall defect, the extent of organ involvement, and any additional anomalies present․ close monitoring and follow-up care are essential to manage any potential complications and optimize outcomes for affected individuals․
Corpus Callosum Agenesis (Brain Malformation)
Corpus callosum agenesis is a rare brain malformation where the structure that connects the brain’s two hemispheres, the corpus callosum, is partially or completely absent․ This condition can lead to a range of neurological issues, including developmental delays, cognitive impairments, and motor function challenges․
Individuals with corpus callosum agenesis may exhibit symptoms such as seizures, intellectual disabilities, and difficulties with coordination and social interactions․ Diagnosis of this condition is often based on imaging studies such as MRI scans that can visualize the absence or underdevelopment of the corpus callosum․
Genetic factors are implicated in corpus callosum agenesis, and some cases may be associated with specific genetic disorders․ Early intervention and multidisciplinary care involving neurologists, developmental specialists, and therapists are crucial for optimizing outcomes for individuals with this brain malformation․
Long-term management of corpus callosum agenesis may focus on addressing the individual’s cognitive and motor challenges, providing appropriate educational support, and managing any associated medical conditions․ Prognosis for individuals with corpus callosum agenesis varies based on the severity of neurological deficits and the presence of any underlying genetic disorders․
Coexistence of Conditions
The coexistence of diaphragmatic hernia, exomphalos, and corpus callosum agenesis in the same individual can present complex medical challenges․ The combination of these congenital anomalies requires thorough evaluation and tailored treatment plans to address the diverse needs of the patient․
Managing the coexistence of these conditions may involve a multidisciplinary team of healthcare professionals, including neonatologists, geneticists, pediatric surgeons, neurologists, and developmental specialists․ Coordination among specialists is essential to provide comprehensive care that addresses the respiratory, surgical, and neurological aspects of these disorders․
Genetic factors play a significant role in the development of these conditions, and genetic testing may be recommended to identify underlying genetic disorders that contribute to the coexistence of diaphragmatic hernia, exomphalos, and corpus callosum agenesis․ Counseling and support for families coping with multiple congenital anomalies are essential for navigating the complexities of treatment and long-term care;
The prognosis for individuals with the coexistence of these conditions depends on a variety of factors, including the severity of each anomaly, the presence of associated complications, and the effectiveness of treatment interventions․ Close monitoring, early interventions, and ongoing support are critical for promoting the best possible outcomes for individuals affected by this complex combination of congenital anomalies․
Genetic Factors and Congenital Anomalies
Genetic factors play a critical role in the development of diaphragmatic hernia, exomphalos, and corpus callosum agenesis․ These congenital anomalies are often associated with gene mutations or chromosomal abnormalities that disrupt normal fetal development, leading to structural and functional abnormalities in multiple organ systems․
Studies have shown that certain genetic disorders increase the risk of these congenital anomalies, highlighting the importance of genetic testing and counseling for affected individuals and their families․ Understanding the genetic underpinnings of these conditions can aid in early detection, intervention, and personalized management approaches․
In some cases, the coexistence of diaphragmatic hernia, exomphalos, and corpus callosum agenesis may be linked to specific genetic syndromes or chromosomal abnormalities․ Identifying the genetic etiology of these conditions can inform prognosis, recurrence risk, and potential treatment options for affected individuals․
Advances in genetic testing technologies have improved the ability to detect genetic factors contributing to congenital anomalies, allowing healthcare providers to offer more targeted and individualized care․ Collaborative efforts between geneticists, pediatric specialists, and other healthcare professionals are essential for comprehensive management and support of individuals with these complex genetic disorders․
Prognosis and Long-Term Care
The prognosis for individuals with diaphragmatic hernia, exomphalos, and corpus callosum agenesis varies based on the severity of their conditions, the presence of associated complications, and the effectiveness of initial interventions․ Early detection, prompt medical management, and ongoing monitoring are crucial for optimizing outcomes and quality of life․
Long-term care for individuals with these congenital anomalies may involve a multidisciplinary team of healthcare professionals, including pediatricians, surgeons, genetic counselors, neurologists, and therapists․ This collaborative approach aims to address the diverse medical, developmental, and social needs of the individual throughout their lifespan․
Individualized care plans tailored to the specific challenges and requirements of each condition are essential for supporting optimal growth, development, and well-being․ Regular follow-up appointments, developmental assessments, and therapeutic interventions are integral components of long-term care for individuals with diaphragmatic hernia, exomphalos, and corpus callosum agenesis․
Families of individuals with these congenital anomalies may benefit from support groups, counseling services, and educational resources to help them navigate the complexities of caregiving and advocate for their loved one’s needs․ Building a strong support network and staying informed about advancements in medical care can empower families to provide the best possible care for their child with these challenging conditions․