Overview of Polyarteritis Nodosa
Cutaneous polyarteritis nodosa (PAN) is a rare form of vasculitis involving small and medium-sized arteries of the skin and subcutaneous tissue. It is often triggered by infections, especially Group A streptococcus, hepatitis B, hepatitis C, and human immunodeficiency virus. It has different clinical features from systemic PAN, which involves multiple organs. Treatment includes corticosteroids, colchicine, cyclophosphamide, and immunoglobulin.
Definition and Classification
Polyarteritis nodosa (PAN) is a form of vasculitis characterized by inflammation of medium-sized arteries, impacting various organs. It is classified as a systemic necrotizing vasculitis affecting muscular arteries, leading to tissue ischemia. With a prevalence of 2-33 cases/million, the exact cause remains unknown. Symptoms range from fever and fatigue to organ-specific manifestations such as neuropathy, renal failure, and skin ulcers. Diagnosis involves biopsy or arteriography, with treatment primarily consisting of corticosteroids and immunosuppressants.
Etiology and Triggers
Polyarteritis nodosa (PAN) has an unclear etiology, with triggers ranging from infections like hepatitis B and C to genetic predisposition and autoimmune processes. The disease mechanism involves the immune system mistakenly attacking the body’s blood vessels, leading to inflammation and subsequent organ damage. Environmental factors and certain medications may also play a role in triggering PAN.
Clinical Manifestations
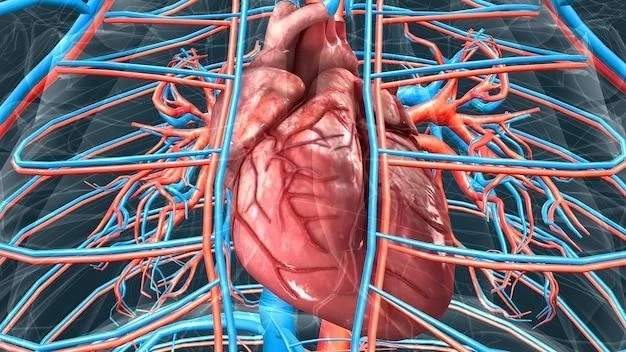
Clinical manifestations of polyarteritis nodosa (PAN) vary widely based on the organ systems affected. Common symptoms include fever, skin ulcers, nerve damage, gastrointestinal issues, and kidney involvement. The disease can present acutely or develop gradually, affecting different organs such as the heart, joints, and eyes. Diagnosis involves a thorough assessment of symptoms and may require various tests for confirmation.
Cutaneous Polyarteritis Nodosa vs. Systemic Polyarteritis Nodosa
Cutaneous polyarteritis nodosa (PAN) primarily involves small and medium-sized arteries of the skin and subcutaneous tissue, often triggered by infections like hepatitis B and C; On the other hand, systemic PAN affects various internal organs and muscular arteries. Clinical features and treatment options differ between the two forms of the disease.
Common Symptoms and Organ Involvement
The symptoms of polyarteritis nodosa (PAN) vary depending on the affected organs but commonly include fever, skin ulcers, nerve damage, gastrointestinal problems, kidney dysfunction, and joint pain. Organ involvement can include the skin, kidneys, nerves, gastrointestinal tract, heart, eyes, and genitals. Prompt diagnosis and treatment are crucial to manage the disease effectively.
Diagnosis of polyarteritis nodosa (PAN) often involves conducting a biopsy of affected tissue to observe characteristic inflammatory changes in medium-sized blood vessels. In addition, arteriography may be performed to visualize and assess the extent of arterial damage and microaneurysms associated with the condition.
Biopsy and Arteriography
Polyarteritis nodosa (PAN) diagnosis often involves biopsy to observe arterial inflammation and arteriography to assess arterial damage and microaneurysms. These procedures help confirm the presence of medium-sized artery inflammation characteristic of PAN.
Laboratory Tests
Laboratory tests play a critical role in diagnosing polyarteritis nodosa (PAN); They may include blood tests to assess markers of inflammation, organ function, and autoantibodies. Elevated levels of inflammatory markers like C-reactive protein and erythrocyte sedimentation rate, along with specific autoantibodies, can aid in confirming the diagnosis of PAN.
Pathophysiology of Polyarteritis Nodosa
Polyarteritis nodosa (PAN) involves inflammation of medium-sized arteries, leading to tissue damage and organ dysfunction. The disease is characterized by the formation of microaneurysms along the affected vessels, contributing to tissue ischemia and potential complications. Understanding the pathophysiological mechanisms of PAN is crucial for effective management and treatment.
Inflammation of Medium-Sized Arteries
Polyarteritis nodosa (PAN) is characterized by the inflammation of medium-sized arteries, particularly affecting muscular arteries and causing tissue ischemia. The disease manifests as necrotizing lesions impacting various organs, with microaneurysms forming along vascular structures. This vascular damage leads to compromised blood flow and potential ischemic events throughout the body.
Formation of Microaneurysms
In polyarteritis nodosa (PAN), the disease process involves the formation of microaneurysms along affected blood vessels. These microaneurysms are a hallmark feature of PAN, contributing to tissue ischemia and potential organ damage. By understanding the formation of these microaneurysms, healthcare providers can better grasp the pathophysiology of PAN and tailor treatment strategies accordingly.

Historical Background
Polyarteritis nodosa (PAN) was first described in 1866 by Adolph Kussmaul and Rudolph Maier. It typically affects medium-sized arterial vessels, leading to necrotizing inflammation. Over the years, understanding of the disease and its treatment has evolved, improving the management of this systemic vasculitis.
Discovery and Description by Kussmaul and Maier
Polyarteritis nodosa (PAN) was first described in 1866 by Adolph Kussmaul and Rudolph Maier. This systemic necrotizing vasculitis primarily affects medium-sized arterial vessels, distinguishing it from other types of vasculitis. The initial description laid the foundation for understanding and managing this complex disease.
Evolution of Understanding and Treatment
Since its initial description in 1866٫ the understanding and treatment of polyarteritis nodosa (PAN) have evolved significantly. Advances in diagnostic techniques٫ such as biopsy and arteriography٫ have improved accuracy. Treatment approaches have also progressed٫ with a focus on corticosteroids and immunosuppressants to manage inflammation and reduce the risk of organ damage.
Epidemiology and Risk Factors
Polyarteritis nodosa (PAN) is a rare vasculitis affecting medium-sized muscular arteries with an unknown etiology. It presents with a range of symptoms and can be triggered by infections like hepatitis B and C. The disease’s prevalence ranges from 2 to 33 cases per million, and understanding its epidemiology and risk factors is essential for effective management.
Prevalence and Incidence Rates
Polyarteritis nodosa (PAN) is considered a rare disease, with a prevalence ranging from 2 to 33 cases per million individuals. The disease primarily affects medium-sized muscular arteries and can lead to organ ischemia and damage. Understanding the epidemiological data regarding PAN is crucial for appropriate management and treatment strategies.
Association with Hepatitis B and Other Infections
Polyarteritis nodosa (PAN) has been associated with infections such as hepatitis B and C. These infections can trigger the onset of PAN or exacerbate the disease. Understanding the link between PAN and infectious agents is crucial for effective management and targeted treatment strategies.

Treatment Approaches
Treatment of polyarteritis nodosa (PAN) typically involves medications such as corticosteroids, immunosuppressants like cyclophosphamide, and other drugs to address inflammation and suppress the immune response. Management may also include therapies targeting specific triggers like antiviral medications in cases associated with hepatitis B or other infections.
Medications⁚ Corticosteroids, Immunosuppressants
The primary treatment approach for polyarteritis nodosa (PAN) involves the use of corticosteroids and immunosuppressants. Corticosteroids help reduce inflammation, while immunosuppressants work to suppress the overactive immune response that leads to arterial inflammation. These medications are crucial in managing PAN and preventing disease progression.
Role of Antiviral Therapy in Hepatitis B-Associated PAN
For cases of polyarteritis nodosa (PAN) associated with hepatitis B, antiviral therapy plays a crucial role in managing the disease. By addressing the underlying viral infection, antiviral medications can help improve outcomes and reduce disease activity in patients with PAN triggered by hepatitis B.
Prognosis and Complications
Polyarteritis nodosa (PAN) can lead to severe complications if left untreated, such as progressive renal failure and gastrointestinal issues. Prompt intervention with corticosteroids and immunosuppressants can help achieve remission in up to 90% of patients, mitigating the risks associated with untreated PAN and providing long-term management strategies.
Risks of Untreated PAN
Untreated polyarteritis nodosa (PAN) can lead to severe complications such as progressive renal failure, gastrointestinal issues, damage to the nervous system, and heart problems. It is crucial to initiate prompt treatment with corticosteroids and immunosuppressants to prevent these risks and achieve disease remission.
Achieving Remission and Long-Term Management
Proper treatment of polyarteritis nodosa (PAN) can lead to disease remission in up to 90% of patients, reducing the risks associated with the condition. Long-term management involves continued medication, regular follow-up visits, and monitoring for any signs of disease activity to ensure optimal health outcomes.
Ongoing Research and Future Directions
Ongoing research in polyarteritis nodosa (PAN) focuses on developing novel therapies and treatment strategies to improve outcomes for patients. Additionally, genetic studies are shedding light on the underlying mechanisms of PAN, potentially leading to more targeted and personalized approaches in the future for managing this complex vasculitis.
Novel Therapies and Treatment Strategies
Current research in polyarteritis nodosa (PAN) focuses on developing innovative therapies and treatment strategies to enhance patient outcomes. By exploring new approaches, such as targeted drug interventions or immunomodulatory therapies, researchers aim to improve the efficacy and safety of treatments for PAN in the future.
Impact of Genetic Studies on Understanding PAN
Genetic studies play a significant role in enhancing our understanding of polyarteritis nodosa (PAN) by unraveling the underlying genetic mechanisms contributing to the disease. Through genetic research, scientists aim to identify potential genetic markers, risk factors, and personalized treatment approaches, ultimately paving the way for more tailored and effective management strategies for PAN.