Introduction
Pancreatic islet cell tumors are rare hormone-producing tumors that form in the pancreas. These tumors can be benign or cancerous, arising from the islet cells that produce hormones in the body.
Pancreatic islet cell tumors, also known as pancreatic neuroendocrine tumors, are rare hormone-producing tumors that originate from the islet cells within the pancreas. These tumors can be benign or malignant, and they have the potential to produce various hormones, leading to specific symptoms based on the hormone type. Understanding the terminology related to these tumors, such as islet cell tumors or pancreatic NETs, is crucial in diagnosing and treating them effectively.
While pancreatic neuroendocrine tumors are less common than exocrine pancreatic tumors, they play a significant role in affecting endocrine functions in the body. Factors that increase the risk of developing these tumors include genetic mutations and certain syndromes. Early diagnosis and management of pancreatic islet cell tumors are essential in improving patient outcomes and quality of life.
Types and Characteristics
VIPoma, also known as Verner-Morrison syndrome, is a type of pancreatic islet cell tumor that causes excessive secretion of vasoactive intestinal peptide (VIP). VIPoma can lead to severe diarrhea, dehydration, and electrolyte imbalances.
Overview of Pancreatic Islet Cell Tumors
Pancreatic islet cell tumors, also known as pancreatic neuroendocrine tumors, are rare hormone-producing tumors that originate in the islet cells of the pancreas. These tumors can be benign or malignant, with the potential to produce various hormones leading to distinct symptoms. Understanding the terminology, risk factors, and genetic associations related to pancreatic islet cell tumors is crucial in diagnosis and treatment decisions.
Neuroendocrine Origin of Islet Cell Tumors
Islet cell tumors, also known as pancreatic neuroendocrine tumors, arise from the specialized islet cells within the pancreas. These tumors can be benign or malignant and have the potential to produce various hormones, leading to distinct symptoms based on the hormone secretion. Understanding the neuroendocrine origin of these tumors is crucial for accurate diagnosis and management.
Clinical Aspects
Pancreatic islet cell tumors’ clinical presentations vary based on the hormones produced, with symptoms such as hypoglycemia, flushing, diarrhea, and peptic ulcers. Diagnosis involves imaging studies, hormone level tests, and biopsy confirmation.
VIPoma (Verner-Morrison syndrome)
VIPoma, also known as Verner-Morrison syndrome, is a rare type of pancreatic islet cell tumor that causes excessive production of vasoactive intestinal peptide (VIP). This condition can lead to symptoms like severe diarrhea, electrolyte imbalances, and dehydration due to the hormonal effects of VIP. Diagnosis involves assessing hormone levels and imaging studies to locate and characterize the tumor in the pancreas.
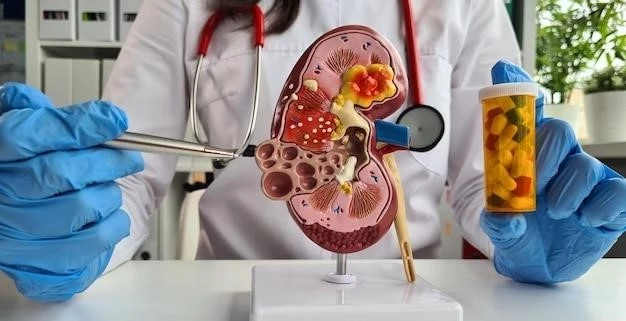
Treatment Options
Treatment for pancreatic islet cell tumors may involve surgery, hormone therapy, radiation therapy, and chemotherapy. Surgical removal of the tumor is a common approach, especially for localized tumors. Hormone therapy aims to manage symptoms related to hormone production by the tumor. Radiation therapy and chemotherapy may be used in cases where surgery alone is not sufficient to control the tumor growth or spread.
Epidemiology
Pancreatic islet cell tumors are rare, accounting for less than 5% of all pancreatic neoplasms. These tumors occur most commonly in adults aged 30 to 60 years, with a slight female predominance. Understanding the prevalence and incidence rates of pancreatic islet cell tumors is essential for effective management strategies.
Prevalence of Pancreatic Islet Cell Tumors
Pancreatic islet cell tumors are rare, comprising less than 5% of all pancreatic neoplasms. These tumors predominantly affect adults aged 30 to 60 years٫ with a slightly higher incidence in females. Understanding the prevalence of pancreatic islet cell tumors is vital for appropriate management and treatment strategies.
Pancreatic islet cell tumors can be associated with genetic conditions like multiple endocrine neoplasia type 1 (MEN1)٫ highlighting the role of genetic factors in tumor development. Understanding these links is crucial for assessing the risk of developing these tumors.
Genetic Factors
Genetic associations play a significant role in pancreatic islet cell tumors, with conditions like multiple endocrine neoplasia type 1 (MEN1) being linked to tumor development.
Pathophysiology
Understanding the mechanisms of tumor development in pancreatic islet cell tumors is crucial for effective treatment strategies and patient outcomes. These tumors arise from the specialized islet cells within the pancreas, with factors like genetic mutations playing a significant role in their pathogenesis.
Risk Factors and Genetic Associations
Genetic conditions like multiple endocrine neoplasia type 1 (MEN1) are associated with an increased risk of developing pancreatic islet cell tumors. Understanding these genetic links can help in identifying individuals at higher risk and implementing appropriate screening or preventive measures.
Prognostic indicators for pancreatic islet cell tumors are important for treatment decisions and assessing survival rates. Effective management includes a multidisciplinary approach involving surgery, hormone therapy, radiation, and chemotherapy to improve patient outcomes.
Prognosis and Management
Prognostic indicators and survival rates are essential for guiding the management of pancreatic islet cell tumors. Effective treatment strategies involve a multidisciplinary approach comprising surgery, hormone therapy, radiation, and chemotherapy to enhance patient outcomes and quality of life.
Research and Developments
Continued research aims to explore novel treatment modalities that target specific molecular pathways involved in pancreatic islet cell tumor development, enhancing therapeutic outcomes and patient prognosis.
Advancements in Treatment Modalities
Ongoing research is focused on developing novel therapeutic approaches targeting specific molecular pathways involved in the development of pancreatic islet cell tumors. These advancements aim to enhance treatment outcomes and improve overall patient prognosis through personalized and effective interventions.

In conclusion, advancements in understanding genetic factors, treatment modalities, and prognosis of pancreatic islet cell tumors are enhancing patient outcomes and guiding personalized care approaches.
Summary of Pancreatic Islet Cell Tumors
Pancreatic islet cell tumors, rare neuroendocrine tumors originating in the pancreas, present a range of hormone-producing capabilities affecting various bodily functions. With advances in genetic understanding and treatment modalities, personalized care approaches have improved patient outcomes and management strategies.