Understanding Medullary Cystic Kidney Disease
Medullary Cystic Kidney Disease is a rare genetic disorder impacting kidney function. It manifests through proteinuria, hematuria, urinary tract infections, leading to renal failure. Understanding the causes and genetic basis of this condition is essential for diagnosis and treatment.
Early symptoms may include anemia, fatigue, and high blood pressure. Diagnosis involves blood and urine tests, imaging studies, and genetic testing. If left untreated, the disease progresses, ultimately requiring dialysis or a renal transplant for survival.
Exploring the relationship between Medullary Cystic Kidney Disease and Nephronophthisis is crucial for a comprehensive grasp of these conditions. While some cases are autosomal dominant, others are autosomal recessive, affecting individuals differently.
Consulting with a nephrologist if you suspect symptoms related to kidney function is paramount. By understanding the disease’s progression and available treatment options like dialysis or renal transplants, patients can make informed decisions regarding their health.
Overview of Medullary Cystic Kidney Disease
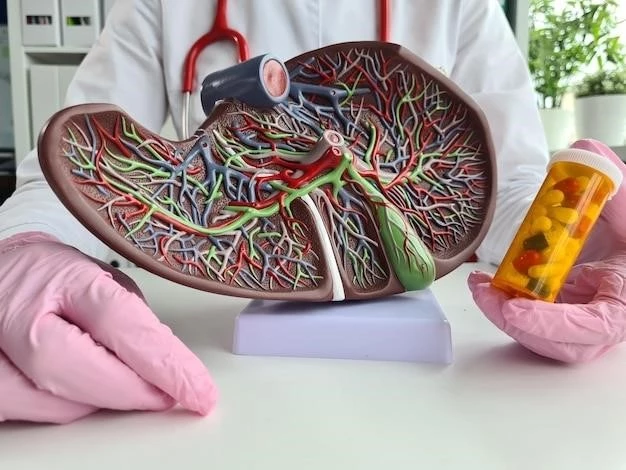
Medullary Cystic Kidney Disease (MCKD) is a rare genetic disorder that affects the kidneys. It is characterized by the formation of cysts in the medulla, the inner part of the kidney. These cysts gradually replace normal kidney tissue, leading to impaired kidney function over time.
MCKD can present in two forms⁚ autosomal dominant MCKD and autosomal recessive MCKD. Autosomal dominant MCKD typically affects adults and progresses slowly, while autosomal recessive MCKD is more severe and usually presents in childhood or adolescence.
Individuals with MCKD may experience symptoms such as proteinuria (the presence of excess protein in the urine), hematuria (blood in the urine), urinary tract infections, and hypertension. These symptoms can vary in severity and may worsen as the disease progresses.
Diagnosis of MCKD involves a thorough medical history, physical examination, blood tests, urine tests, imaging studies (such as ultrasound or MRI), and genetic testing. Early detection of MCKD is essential for implementing appropriate treatment and management strategies.
It is important for individuals with MCKD to monitor their kidney function regularly and follow the treatment plan outlined by their healthcare provider. Treatment options for MCKD may include medications to control blood pressure, manage proteinuria, and treat urinary tract infections.
In advanced stages of MCKD where kidney function is significantly impaired, individuals may require dialysis to perform the kidney’s filtration functions artificially. In some cases, a renal transplant may be necessary to replace a failed kidney with a healthy donor kidney.
Living with MCKD can be challenging, but with proper medical care, lifestyle modifications, and support from healthcare professionals, individuals can manage the disease and maintain a good quality of life. It is essential to stay informed about MCKD, adhere to treatment recommendations, and seek help when needed.
Causes and Genetic Basis
The causes of Medullary Cystic Kidney Disease (MCKD) lie in genetic mutations that affect the normal functioning of the kidneys. In autosomal dominant MCKD, a mutation in a single copy of the responsible gene is sufficient to cause the disease. Autosomal recessive MCKD, on the other hand, requires mutations in both copies of the gene.
Genetic studies have identified several genes associated with MCKD, including UMOD, MUC1, and REN. Mutations in these genes disrupt the kidney’s ability to regulate fluid and electrolyte balance properly, leading to cyst formation and progressive kidney damage.
Individuals with a family history of MCKD are at a higher risk of inheriting the genetic mutation and developing the disease. Genetic counseling can help assess the risk of passing the gene mutation to future generations and provide information on family planning options.
Understanding the genetic basis of MCKD is crucial for accurate diagnosis and personalized treatment strategies. Genetic testing can confirm the presence of gene mutations associated with MCKD and guide healthcare providers in developing tailored management plans.
While genetic mutations play a significant role in the development of MCKD, environmental factors and lifestyle choices can also impact disease progression. Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption, can help support kidney health in individuals at risk of MCKD.
Research into the genetic basis of MCKD continues to advance our understanding of the disease and may lead to future targeted therapies aimed at correcting genetic defects and preventing kidney damage. Participation in clinical trials and genetic research studies can contribute to ongoing efforts to unravel the complexities of MCKD and improve treatment outcomes for affected individuals.
Consulting with a genetic counselor or healthcare provider knowledgeable about MCKD can provide valuable insights into the genetic basis of the disease and empower individuals with the information needed to make informed decisions about their health and well-being.
Symptoms and Diagnosis
Recognizing the symptoms of Medullary Cystic Kidney Disease (MCKD) is crucial for early diagnosis and treatment. Common symptoms of MCKD include proteinuria, hematuria, hypertension, urinary tract infections, and progressive kidney dysfunction. These symptoms may vary in severity and can have a significant impact on an individual’s quality of life.
If you experience persistent symptoms such as blood in the urine, foamy urine, frequent urinary tract infections, or unexplained fatigue, it is important to seek medical attention promptly. A healthcare provider can perform a series of tests to evaluate kidney function and determine the underlying cause of your symptoms.
Diagnosing MCKD typically involves a comprehensive approach that includes a thorough medical history, physical examination, blood tests, urine tests, and imaging studies. Blood tests may reveal abnormalities in kidney function, while urine tests can detect the presence of protein and blood, indicative of kidney damage.
Imaging studies such as ultrasound, CT scans, or MRI scans may be used to visualize the structure of the kidneys and identify any cysts or abnormalities present. Genetic testing may also be recommended to determine if a specific gene mutation is responsible for MCKD in an individual or their family.
Early diagnosis of MCKD is essential for implementing appropriate treatment strategies and slowing the progression of kidney damage. If you have a family history of kidney disease or suspect that you may be experiencing symptoms of MCKD, do not hesitate to discuss your concerns with a healthcare provider.
Regular monitoring of kidney function through blood tests, urine tests, and imaging studies can help track the progression of MCKD and guide treatment decisions. It is important to advocate for your health and work closely with your healthcare team to manage MCKD effectively.
By being proactive about monitoring your symptoms and seeking timely medical care, you can take control of your health and well-being. Remember that early detection and intervention are key to managing MCKD and preserving kidney function for as long as possible.
Progression of the Disease
Understanding the progression of Medullary Cystic Kidney Disease (MCKD) is essential for individuals and healthcare providers to make informed decisions about treatment and management strategies. MCKD is a progressive condition that can lead to a gradual decline in kidney function over time.
In the early stages of MCKD, individuals may experience mild symptoms such as proteinuria, hematuria, or hypertension. As the disease progresses, the kidney’s ability to filter waste and regulate fluid balance becomes compromised, leading to more severe symptoms and complications.

Cysts that form in the medulla of the kidney can impair normal kidney function by replacing healthy tissue and disrupting the nephrons, the filtering units of the kidney. This can result in a decrease in the glomerular filtration rate (GFR), which measures how well the kidneys are filtering waste from the blood.
As kidney function declines further, individuals with MCKD may develop complications such as electrolyte imbalances, fluid retention, anemia, and bone disorders. These complications can impact overall health and quality of life, necessitating close monitoring and intervention from healthcare providers.
In advanced stages of MCKD, when kidney function is significantly impaired, individuals may require renal replacement therapy such as dialysis or a kidney transplant. Dialysis helps perform the kidney’s filtration function artificially, removing waste products and excess fluid from the blood.
A kidney transplant may be considered for individuals with end-stage renal disease due to MCKD. During a kidney transplant, a healthy donor kidney is surgically placed in the recipient’s body to replace the failed kidney. This procedure offers the possibility of improved kidney function and quality of life.
It is important for individuals with MCKD to work closely with their healthcare team to monitor the progression of the disease, optimize treatment strategies, and address any complications that may arise. Regular follow-up appointments, blood tests, and imaging studies can help track changes in kidney function and guide treatment decisions.
By staying informed about the progression of MCKD and participating in proactive management of the disease, individuals can maximize their kidney health and quality of life. It is crucial to be proactive in managing MCKD to delay disease progression and maintain optimal kidney function for as long as possible.
Treatment Options
Managing Medullary Cystic Kidney Disease (MCKD) involves a combination of treatment strategies aimed at controlling symptoms, slowing disease progression, and preserving kidney function. Treatment options for MCKD focus on addressing complications, managing symptoms, and supporting overall kidney health.
One key aspect of MCKD treatment is the control of hypertension and proteinuria, which can help minimize kidney damage and delay disease progression. Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are commonly prescribed to manage blood pressure and reduce proteinuria.
Regular monitoring of kidney function through blood tests, urine tests, and imaging studies is essential to track disease progression and adjust treatment plans accordingly. Healthcare providers may recommend lifestyle modifications such as a low-salt diet, regular exercise, and avoiding nephrotoxic substances to support kidney health.
In cases where MCKD has led to significant kidney damage and impaired function, renal replacement therapy may be necessary. Dialysis is a treatment option that helps remove waste products and excess fluid from the blood when the kidneys are no longer able to perform these functions effectively.
Kidney transplant is another treatment option for individuals with end-stage renal disease due to MCKD. A kidney transplant involves surgically replacing a failed kidney with a healthy donor kidney, offering the potential for improved kidney function and quality of life.
It is essential for individuals with MCKD to work closely with a multidisciplinary healthcare team, including nephrologists, genetic counselors, and transplant specialists, to develop a comprehensive treatment plan tailored to their specific needs. Regular follow-up visits and monitoring are critical to assess treatment effectiveness and adjust interventions as needed.
Adhering to prescribed medications, following dietary recommendations, maintaining a healthy lifestyle, and attending scheduled appointments are crucial components of managing MCKD effectively. By actively participating in their care and staying informed about the latest advancements in MCKD treatment, individuals can optimize their quality of life and kidney health.
Support groups and resources for individuals with MCKD and their families can provide valuable emotional support, education, and empowerment. Seeking information from reputable sources and engaging with healthcare providers can help individuals make informed decisions about their treatment and overall well-being.
Nephronophthisis and its Relationship to Medullary Cystic Kidney Disease
Nephronophthisis (NPHP) is a rare genetic disorder that primarily affects the kidneys, leading to the development of medullary cysts and progressive kidney damage. NPHP shares similarities with Medullary Cystic Kidney Disease (MCKD) in terms of symptoms, genetic basis, and disease progression, highlighting a close relationship between the two conditions.
Both NPHP and MCKD are characterized by the formation of cysts in the kidney tissue, particularly in the medulla. These cysts can impair kidney function by disrupting the structure of the nephrons, the functional units of the kidney responsible for filtering waste products from the blood.
Genetic studies have identified overlapping genes associated with NPHP and MCKD, suggesting a shared genetic basis between these disorders. Mutations in genes such as NPHP1, NPHP4, and UMOD have been linked to the development of both NPHP and MCKD, underscoring the genetic complexity of these conditions.
Individuals with a family history of NPHP or MCKD may be at an increased risk of inheriting genetic mutations associated with these disorders. Genetic counseling and testing can help assess the risk of passing on gene mutations to future generations and guide family planning decisions.
Diagnosing NPHP and MCKD often involves a combination of clinical evaluation, genetic testing, imaging studies, and monitoring of kidney function. Early detection of these disorders is essential for implementing appropriate treatment strategies and improving outcomes for affected individuals.
Although NPHP and MCKD are distinct conditions, their shared characteristics underscore the importance of understanding their relationship and the potential implications for diagnosis, treatment, and genetic counseling. Healthcare providers knowledgeable about both disorders can provide valuable insights and guidance for individuals and families affected by NPHP and MCKD.
Research into the genetic basis of NPHP and MCKD continues to advance our understanding of these disorders and may lead to innovative treatment approaches in the future. Participation in clinical studies and genetic research can contribute to ongoing efforts to unravel the complexities of NPHP, MCKD, and related kidney diseases.
By staying informed about the relationship between NPHP and MCKD, individuals can empower themselves to advocate for their health, seek appropriate medical care, and make informed decisions about genetic testing, treatment options, and family planning. Collaboration with healthcare providers and specialists in nephrology and medical genetics is key to managing these complex kidney disorders effectively.