Understanding Dermatofibroma
When it comes to understanding dermatofibroma, it’s crucial to delve into the characteristics, histopathology, types, diagnosis, symptoms, treatment options, and prevention strategies. Stay informed to make informed decisions about your skin health.
Introduction to Dermatofibroma
Welcome to the insightful journey of understanding dermatofibroma. This benign fibrous growth, often referred to as a dermal tumor, manifests in the skin’s dermal layer composed of collagen. Dermatofibromas present as nodular or scar-like lesions, commonly pigmented. Exploration through dermoscopy, biopsy, and excision can shed light on their nature. Let’s delve deeper into this intriguing skin condition to enhance your knowledge for informed decision-making regarding your skin health.
Characteristics of Dermatofibroma
Dermatofibromas are benign fibrous growths that typically arise in the skin’s dermal layer. These growths are composed of collagen and often present as firm, raised nodules or papules on the skin’s surface. Dermatofibromas may have a variable appearance, ranging from pink to brown or even black, with a central dimple upon compression known as the ‘dimple sign.’ While most dermatofibromas are harmless, it is important to have any new or changing skin lesions evaluated by a dermatologist to ensure an accurate diagnosis and appropriate management. Understanding the characteristics of dermatofibromas can empower individuals to monitor their skin health effectively and seek timely medical intervention when necessary.
Histopathology of Dermatofibroma
Examining the histopathology of dermatofibroma provides valuable insights into its composition and structure. Under microscopic analysis, dermatofibromas typically exhibit a dermal proliferation of spindle-shaped fibroblasts and collagen bundles, often arranged in a storiform pattern. Characteristic features may include a surrounding pseudocapsule, a central zone of fibroblasts, and a peripheral zone rich in collagen. Additionally, histopathological examination may reveal hemosiderin deposits, contributing to the lesion’s characteristic pigmentation. Understanding the histopathology of dermatofibroma can aid in confirming the diagnosis and distinguishing it from other skin conditions with similar presentations. Consultation with a dermatopathologist for accurate histological assessment is recommended for individuals with suspected or atypical dermatofibromas to guide appropriate management decisions.
Types of Dermatofibroma
While dermatofibromas commonly exhibit similar characteristics, variations in their appearance and features may lead to different types. These variations can include dermatofibromas with unusual clinical presentations, such as multiple or eruptive lesions, atypical colors, or rapid growth. Additionally, molecular studies have identified specific subtypes of dermatofibromas with distinct genetic mutations, contributing to their diverse nature. Understanding the various types of dermatofibroma can aid healthcare providers in making accurate diagnoses and developing individualized management plans for patients. Regular skin examinations and prompt evaluation of any new or changing lesions are essential to identifying and addressing different types of dermatofibromas effectively.
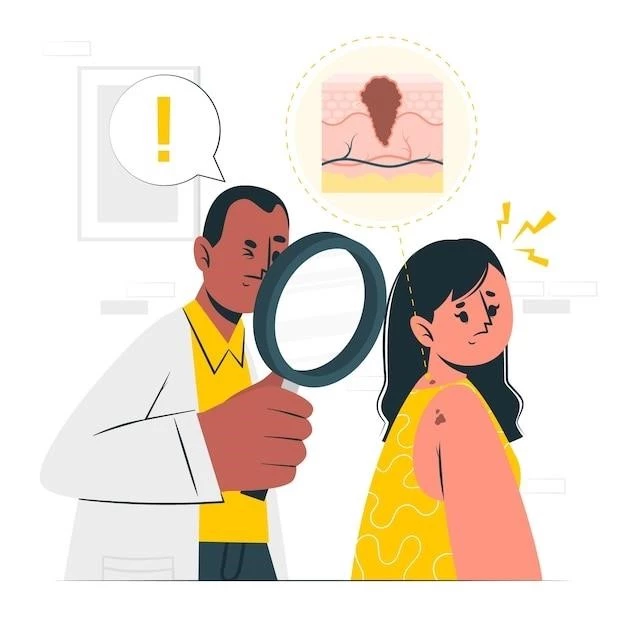
Diagnosis of Dermatofibroma
Diagnosing dermatofibroma involves a comprehensive approach that may include clinical evaluation, dermoscopy, biopsy, and histological examination. Dermatologists typically assess the lesion’s appearance, texture, and tenderness during a physical examination to differentiate dermatofibromas from other skin growths. Dermoscopy, a non-invasive technique that magnifies the skin’s surface, can provide additional details about the lesion’s structure and vascular patterns. A skin biopsy, where a sample of tissue is obtained and examined under a microscope, is often performed to confirm the diagnosis histologically. Healthcare providers may recommend excisional biopsy for suspicious or atypical lesions to rule out other skin conditions and ensure appropriate management. Seeking timely medical evaluation and utilizing diagnostic tools can facilitate accurate diagnosis and guide the most suitable treatment strategy for dermatofibromas.
Symptoms and Complications
Typically, dermatofibromas do not cause significant symptoms or complications. These benign fibrous growths often appear as small, firm nodules on the skin, which may be slightly raised and pigmented. While most dermatofibromas are harmless and painless, individuals may experience tenderness or itching in some cases. Complications such as ulceration, bleeding, or rapid growth are rare but should be promptly evaluated by a healthcare provider. It is important to monitor any changes in the size, color, or texture of dermatofibromas and seek medical attention if concerning symptoms or complications arise. Regular skin self-checks and dermatological assessments can help detect any unusual developments and ensure appropriate management to maintain skin health.
Treatment Options
When it comes to managing dermatofibromas, treatment options may vary based on individual factors such as the lesion’s size, location, and symptoms. In many cases, dermatofibromas do not require treatment unless they cause discomfort, aesthetic concerns, or complications. However, if desired or clinically indicated, treatment options include surgical excision, cryotherapy, laser therapy, or corticosteroid injections. Surgical excision, the most common approach, involves removing the dermatofibroma under local anesthesia to prevent recurrence and address any associated symptoms. Cryotherapy and laser therapy can be used to target and remove superficial lesions, while corticosteroid injections may help reduce inflammation and discomfort. Consulting with a dermatologist is crucial to determine the most appropriate treatment option based on your unique situation and preferences.
Surgical Excision Procedure
During a surgical excision procedure for dermatofibroma, the dermatologist or surgeon will first numb the area with local anesthesia to ensure your comfort. Using specialized tools, the dermatofibroma is carefully removed from the skin, including a margin of healthy tissue to reduce the risk of recurrence. The wound is then meticulously closed with sutures to promote proper healing and minimize scarring. Following the procedure, your healthcare provider will provide post-operative instructions on wound care, activity restrictions, and monitoring for any signs of infection. It is essential to follow these guidelines diligently to support optimal healing and achieve the best possible outcome. Regular follow-up appointments will allow your healthcare team to assess the surgical site’s progress, address any concerns, and ensure a smooth recovery process.
Follow-up Care
After undergoing treatment for dermatofibroma, consistent follow-up care is crucial to monitor healing progress, detect any signs of recurrence, and address potential complications. Your healthcare provider may schedule follow-up appointments to assess the surgical site, evaluate tissue healing, and ensure that any post-operative symptoms are resolving appropriately. It is essential to adhere to any recommended wound care instructions, such as keeping the area clean and dry, changing dressings as instructed, and avoiding activities that may disrupt the healing process. If you notice any changes in the surgical site, such as increasing redness, swelling, pain, or discharge, promptly contact your healthcare provider for further evaluation. By actively participating in follow-up care, you can contribute to a successful recovery and maintain optimal skin health.
Prevention Strategies
While dermatofibromas may not be entirely preventable, adopting certain strategies can help promote overall skin health and potentially reduce the risk of developing these benign growths. Protecting your skin from excessive sun exposure by using sunscreen, wearing protective clothing, and seeking shade during peak hours can aid in preventing various skin issues, including dermatofibromas. Regular skin self-checks to monitor for any new or changing lesions and promptly consulting a dermatologist for evaluation can facilitate early detection and timely management of dermatofibromas. Maintaining a healthy lifestyle, including a balanced diet, adequate hydration, and proper skincare practices, can also contribute to skin wellness. By incorporating preventive measures into your daily routine and staying vigilant about changes in your skin, you can optimize skin health and minimize potential risks associated with dermatofibromas.
Living with Dermatofibroma
Living with dermatofibroma involves understanding the benign nature of these fibrous growths and managing any associated symptoms with guidance from healthcare professionals. While most dermatofibromas are harmless and do not require treatment, individuals may choose to address aesthetic concerns or discomfort through various treatment options. Embracing a proactive approach to skin health by practicing sun safety, conducting regular skin self-examinations, and seeking medical advice for any concerning changes can empower individuals to take charge of their skin well-being. By staying informed about dermatofibromas, following recommended strategies for skin care and monitoring, and maintaining open communication with healthcare providers, individuals can effectively navigate life with dermatofibroma and prioritize their overall health and wellness.
Seeking Medical Advice
Seeking timely medical advice is essential when it comes to addressing dermatofibromas. If you notice any new or changing skin lesions, particularly those with unusual colors, textures, or rapid growth, it is important to consult a dermatologist for a thorough evaluation. Dermatologists have the expertise to accurately diagnose dermatofibromas through physical examinations, dermoscopy, and skin biopsies. Early intervention can help confirm the diagnosis, rule out other skin conditions, and determine the most appropriate treatment plan tailored to your specific needs. By prioritizing regular skin checks, prompt evaluation of concerning skin changes, and proactive communication with healthcare providers, you can ensure timely detection and management of dermatofibromas, promoting skin health and overall well-being.
Research and Advancements
Ongoing research and advancements in the field of dermatology continue to enhance our understanding of dermatofibroma and refine diagnostic and treatment approaches. Studies focusing on the genetic underpinnings of dermatofibromas, novel imaging techniques, and targeted therapies are paving the way for more personalized and effective management strategies. By staying informed about the latest developments in dermatofibroma research, individuals can benefit from emerging technologies and innovative treatments that offer improved outcomes and quality of care. Participating in clinical trials and supporting research efforts can contribute to the advancement of knowledge surrounding dermatofibromas and potentially shape future standards of care. Collaborating with healthcare professionals and remaining engaged in the latest scientific discoveries can empower individuals to make informed decisions about their skin health and well-being.
Conclusion
In conclusion, understanding dermatofibroma is key to navigating this benign fibrous growth effectively. From recognizing its characteristics and histopathology to exploring diagnostic methods and treatment options, informed decision-making plays a vital role in managing dermatofibromas. By prioritizing skin health practices, seeking medical advice promptly, and staying abreast of research advancements, individuals can empower themselves to address dermatofibromas proactively. Remember, early detection, regular skin monitoring, and collaborative care with healthcare providers are fundamental to maintaining optimal skin wellness. With a proactive approach and a focus on skin health, individuals can confidently navigate life with dermatofibroma and prioritize overall well-being.
