Essential Thrombocytosis
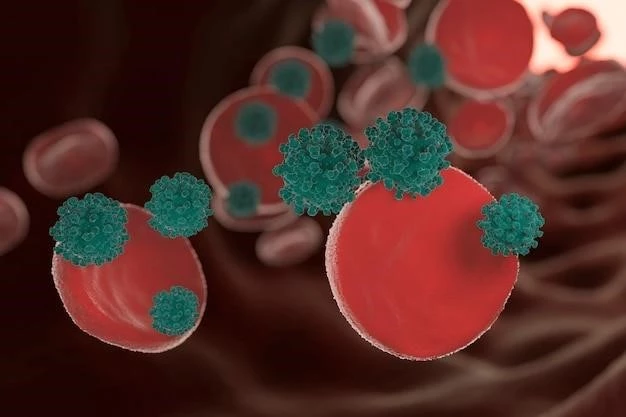
Essential Thrombocytosis, also known as primary thrombocythemia, is a rare blood disorder characterized by the overproduction of platelets in the bone marrow. This condition can lead to blood clots (thrombosis) or bleeding due to abnormal blood cell counts. Common complications include hemorrhage, iron deficiency, and splenomegaly.
Introduction
Essential Thrombocytosis is a rare chronic myeloproliferative neoplasm (MPN) characterized by the excessive production of platelets in the bone marrow. This leads to an elevated platelet count in the bloodstream, increasing the risk of blood clots (thrombosis) or bleeding complications. While the exact cause is often unknown, it is linked to mutations in the JAK2, MPL, or CALR genes.
Individuals with Essential Thrombocytosis may remain asymptomatic and the condition is often detected incidentally during routine blood tests. However, symptoms may include headaches, dizziness, chest pain, weakness, and numbness in the extremities. Diagnosis is made through blood tests, bone marrow biopsy, and genetic testing to confirm the presence of the JAK2 mutation.
Managing Essential Thrombocytosis involves monitoring the blood cell counts regularly to assess the risk of complications. Treatment strategies aim to reduce the risk of blood clots and control platelet counts. Prognosis varies depending on individual factors and response to treatment. Essential Thrombocytosis is closely related to other myeloproliferative neoplasms (MPNs) such as polycythemia vera and primary myelofibrosis.
Potential complications of Essential Thrombocytosis include an increased risk of thrombosis, particularly in the arteries and veins, which can lead to serious conditions such as stroke or heart attack. On the other hand, bleeding or hemorrhage may occur due to abnormal platelet function. In some cases, the spleen may become enlarged (splenomegaly) as a result of increased platelet production.
Causes and Risk Factors
Essential Thrombocytosis is primarily caused by mutations in the bone marrow stem cells that produce blood cells. The most common mutations associated with this condition are in the JAK2, MPL, or CALR genes, which play a crucial role in regulating blood cell production.
While the exact cause of these mutations is often unknown, certain risk factors may contribute to the development of Essential Thrombocytosis. These risk factors include age, as the condition is more common in middle-aged to older adults, and a history of other myeloproliferative neoplasms (MPNs) such as polycythemia vera or primary myelofibrosis.
Gender may also play a role, as Essential Thrombocytosis is slightly more common in females. Additionally, a family history of MPNs or inherited genetic mutations may increase the likelihood of developing the disorder. Exposure to certain chemicals or radiation may also be a risk factor for the development of Essential Thrombocytosis, although more research is needed to understand the precise relationship.
Overall, while the exact causes and risk factors for Essential Thrombocytosis may vary, understanding these genetic and environmental influences is essential for early detection, management, and treatment of the condition.
Symptoms and Diagnosis
Essential Thrombocytosis can present with a range of symptoms, although some individuals may remain asymptomatic and the condition is often detected incidentally through routine blood tests. Common symptoms may include headaches, dizziness, chest pain, weakness, numbness or tingling in the extremities, and visual disturbances.
Diagnosing Essential Thrombocytosis involves a thorough medical history review, physical examination, and various tests to confirm the presence of elevated platelet levels. Blood tests, including a complete blood count (CBC) and peripheral blood smear, can help assess platelet counts and morphology. Additionally, bone marrow biopsy and genetic testing for JAK2, MPL, or CALR mutations may be conducted to confirm the diagnosis.
It is crucial for healthcare providers to differentiate Essential Thrombocytosis from other conditions that may present with similar symptoms, such as reactive thrombocytosis, myelodysplastic syndromes, or other myeloproliferative neoplasms (MPNs). Early and accurate diagnosis is essential for initiating appropriate treatment and managing potential complications associated with the disorder.
Complications of Essential Thrombocytosis
Essential Thrombocytosis can lead to various complications due to the abnormal increase in platelet production. One of the main complications is an increased risk of blood clots (thrombosis) forming in the arteries or veins, which can result in serious conditions like stroke, heart attack, or deep vein thrombosis.
On the other hand, the excessive platelets in the blood may also impair their normal function, leading to bleeding or hemorrhage. This abnormal bleeding can manifest as easy bruising, nosebleeds, or prolonged bleeding from minor cuts or injuries. It is essential to monitor platelet counts regularly to prevent these complications.
Another potential complication of Essential Thrombocytosis is iron deficiency, which can occur due to gastrointestinal bleeding from ulcers or abnormal blood vessel formation. Anemia may develop as a result, causing symptoms like fatigue, weakness, and pale skin. Treating the underlying cause of bleeding is essential to manage iron deficiency.
Splenomegaly, or enlargement of the spleen, may also occur in some individuals with Essential Thrombocytosis. The spleen plays a role in filtering blood and removing old or damaged blood cells, but an enlarged spleen can cause discomfort or pain in the upper abdomen. Monitoring spleen size and function is important to prevent complications.
Treatment Options
The treatment approach for Essential Thrombocytosis aims to reduce the risk of blood clots and manage platelet counts to prevent complications. In many cases, treatment may not be necessary if the individual is asymptomatic and at low risk of thrombosis. However, regular monitoring is crucial.
For individuals at high risk of thrombosis, medications such as low-dose aspirin may be prescribed to prevent blood clots. Antiplatelet drugs like clopidogrel may also be recommended to reduce platelet aggregation and lower the risk of clot formation in the arteries.
In cases where platelet counts are significantly elevated and there is a high risk of complications, cytoreductive therapy may be necessary to lower platelet production. Medications like hydroxyurea or anagrelide can help suppress the bone marrow’s activity, reducing platelet counts and the risk of clotting events.
In rare instances where complications like severe bleeding or enlarged spleen occur, procedures such as platelet pheresis or splenectomy (spleen removal) may be considered. These interventions are typically reserved for specific situations where other treatments have not been effective in controlling symptoms or complications.
Overall, the choice of treatment for Essential Thrombocytosis depends on individual factors like age, overall health, and risk of complications. Close collaboration between healthcare providers, hematologists, and patients is essential to determine the most appropriate and effective treatment plan for managing the condition. Regular follow-up appointments and monitoring of blood cell counts are essential to assess treatment response and adjust therapies as needed.
Monitoring and Management
Regular monitoring of Essential Thrombocytosis is essential to assess disease progression, treatment response, and the risk of complications. Healthcare providers may recommend periodic blood tests to evaluate platelet counts, hemoglobin levels, and white blood cell counts.
Monitoring may also include imaging studies such as ultrasounds or CT scans to assess for the presence of blood clots or complications like splenomegaly. Bone marrow biopsies may be performed periodically to evaluate the status of the bone marrow and assess for disease progression or transformation into other myeloproliferative neoplasms.
Management of Essential Thrombocytosis focuses on controlling platelet levels, reducing the risk of thrombosis, and managing symptoms. Lifestyle modifications such as maintaining a healthy weight, staying physically active, and avoiding smoking can help reduce the risk of complications.
Patients may also be advised to stay hydrated, avoid activities that may increase the risk of bleeding or injury, and adhere to any prescribed medications. Regular follow-up appointments with healthcare providers and hematologists are essential to monitor the effectiveness of treatment, manage potential side effects of medications, and address any new symptoms or concerns.
Through proactive monitoring and management strategies, individuals with Essential Thrombocytosis can effectively reduce the risk of complications, improve quality of life, and optimize long-term outcomes. Collaborating closely with healthcare providers and following recommended monitoring schedules are key components of successful disease management.
Prognosis and Outlook
The prognosis for individuals with Essential Thrombocytosis varies depending on several factors, including age, overall health, response to treatment, and the presence of complications. Many patients with this condition have a relatively favorable prognosis with proper management and monitoring.
With regular monitoring of blood cell counts, appropriate treatment strategies, and lifestyle modifications, individuals can effectively reduce the risk of blood clots, bleeding episodes, and other complications associated with Essential Thrombocytosis. Early detection and intervention play a crucial role in improving outcomes and quality of life.
In some cases, Essential Thrombocytosis may remain stable for many years without causing significant symptoms or complications. However, close collaboration between patients and healthcare providers is essential to ensure ongoing evaluation, adjustment of treatment plans, and timely management of any emerging issues.
Overall, the outlook for individuals with Essential Thrombocytosis is generally positive with proper medical care and adherence to treatment recommendations. By staying informed about the condition, actively participating in their healthcare, and maintaining open communication with their healthcare team, individuals can navigate the complexities of Essential Thrombocytosis and optimize their long-term prognosis.
Connection to Myeloproliferative Neoplasms (MPNs)
Essential Thrombocytosis is closely related to other myeloproliferative neoplasms (MPNs), a group of disorders characterized by the overproduction of blood cells in the bone marrow. Along with Essential Thrombocytosis, MPNs include polycythemia vera, primary myelofibrosis, and chronic myeloid leukemia.
These conditions share common underlying mechanisms, such as mutations in genes like JAK2, MPL, or CALR, which drive abnormal cell growth and proliferation. While each MPN has distinct features and presentations, they are all characterized by the dysregulation of blood cell production, leading to a range of symptoms and complications.
Individuals diagnosed with Essential Thrombocytosis may have an increased risk of developing other MPNs over time, underscoring the importance of ongoing monitoring and evaluation. Understanding the interconnections between different MPNs is critical for accurate diagnosis, appropriate treatment selection, and long-term management.
Through advances in research and clinical practice, healthcare providers can better recognize the relationships between MPNs, tailor treatment plans to address the specific needs of each patient, and improve outcomes for individuals living with these complex blood disorders. Collaboration between hematologists, oncologists, and other specialists is essential in providing comprehensive care for individuals with MPNs.
Potential Complications
Essential Thrombocytosis can lead to various complications that impact the cardiovascular system, blood clotting mechanisms, and overall health of individuals with the condition. One significant complication is the increased risk of thrombosis, which can result in serious conditions such as stroke, heart attack, or pulmonary embolism.
Excessive platelet counts in Essential Thrombocytosis can also lead to abnormal bleeding or hemorrhage, affecting the body’s ability to form blood clots and control bleeding effectively. This may manifest as frequent nosebleeds, easy bruising, or prolonged bleeding from minor cuts or injuries.
Iron deficiency is another potential complication of Essential Thrombocytosis, particularly in cases where gastrointestinal bleeding occurs due to ulcers or abnormal blood vessel formation. Anemia resulting from iron deficiency can cause symptoms like fatigue, weakness, and pale skin, further impacting overall well-being.
Splenomegaly, or enlargement of the spleen, may develop in some individuals with Essential Thrombocytosis as a result of increased platelet production and activity. An enlarged spleen can lead to abdominal discomfort, early satiety, or an increased risk of spleen rupture in rare cases, necessitating close monitoring and potential interventions.
Conclusion
In conclusion, Essential Thrombocytosis is a rare blood disorder characterized by the overproduction of platelets in the bone marrow, leading to an increased risk of blood clots, bleeding complications, iron deficiency, and splenomegaly. This condition is closely linked to other myeloproliferative neoplasms (MPNs) and requires ongoing monitoring and management to mitigate potential complications.
Through early detection, accurate diagnosis, and personalized treatment approaches, individuals with Essential Thrombocytosis can effectively manage their condition and improve their prognosis. Collaboration between healthcare providers, hematologists, and patients is key to developing comprehensive care plans that address individual needs and optimize long-term outcomes.
By staying informed about the symptoms, causes, risk factors, and potential complications of Essential Thrombocytosis, individuals can take proactive steps to maintain their health, minimize the risk of thrombosis or bleeding episodes, and enhance their quality of life. Continued research and advancements in treatment options offer hope for better outcomes and improved management of this complex blood disorder.
Overall, raising awareness about Essential Thrombocytosis, advocating for regular screenings, and fostering open communication between healthcare teams and patients are essential components of managing this condition effectively. With a multidisciplinary approach and a focus on individualized care, individuals with Essential Thrombocytosis can navigate their journey toward better health and well-being.
