Article Plan⁚ Disease ౼ Pneumonia‚ Eosinophilic
The definition of eosinophilic pneumonia depends on the clinical context. In pathology‚ eosinophilic pneumonia refers to a histologic pattern of diffuse pulmonary infiltrates containing prominent numbers of eosinophils.
*Important Note⁚ Always consult a medical professional for accurate diagnosis and treatment.*
Definition and Clinical Context
The definition of eosinophilic pneumonia regards a histologic pattern of lung infiltrates with prominent eosinophils. This condition is characterized by peripheral blood eosinophilia and eosinophilic infiltration in lung tissue.
It is essential to distinguish eosinophilic pneumonia from other clinical syndromes presenting similar histologic patterns. The disorders are categorized as Primary or Secondary based on their etiology.
Chronic eosinophilic pneumonia (CEP) is a condition where eosinophils accumulate in the lung without a known cause‚ leading to abnormal chronic eosinophil build-up. On the other hand‚ idiopathic acute eosinophilic pneumonia (AEP) is a rare cause of acute respiratory failure with a sudden onset.
Histologic Pattern
Eosinophilic pneumonia is identified by a histologic pattern of lung infiltrates rich in eosinophils. The distinctive feature is the accumulation of eosinophils in lung tissue‚ either alongside peripheral blood eosinophilia or without it. The pattern helps differentiate eosinophilic pneumonia from other lung conditions with similar presentations.
The histologic pattern of eosinophilic pneumonia is further classified into various etiological categories‚ aiding in the diagnosis and management of the condition. Understanding the specific histologic pattern can provide valuable insights into the underlying causes and appropriate treatment strategies.
Chronic eosinophilic pneumonia (CEP) and idiopathic acute eosinophilic pneumonia (AEP) are two main classifications within the spectrum of eosinophilic pneumonia‚ each characterized by distinct histologic patterns that guide clinicians in addressing the condition effectively.
Classification of Eosinophilic Pneumonia
Eosinophilic pneumonia encompasses various lung disorders where white blood cells‚ eosinophils‚ accumulate in the lungs and blood‚ leading to inflammation and damage. These disorders are classified based on the presence of eosinophils in lung tissue or blood‚ helping differentiate between primary and secondary causes.
Understanding the classification of eosinophilic pneumonia is crucial for accurate diagnosis and treatment. Primary eosinophilic pneumonia has identifiable causes‚ while idiopathic eosinophilic pneumonia lacks clear triggers. By categorizing these conditions‚ healthcare professionals can tailor interventions to address the specific underlying factors contributing to eosinophilic pneumonia.
If you suspect eosinophilic pneumonia‚ consult a healthcare provider for proper evaluation and management based on the classification of the condition to ensure the most effective care.
Etiologic Categories
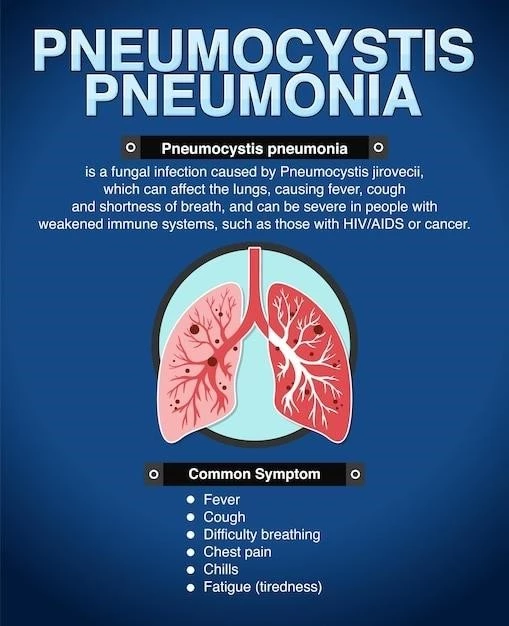
The etiology of eosinophilic pneumonia can be diverse‚ encompassing both infectious and non-infectious causes. Infections by pathogens such as fungi or parasites‚ as well as allergic reactions to medications‚ can lead to eosinophilic pneumonia. Understanding these distinct etiologic categories is essential for accurate diagnosis and appropriate treatment planning.
Common infectious etiologies include fungal infections like Pneumocystis jirovecii‚ while non-infectious causes range from allergic reactions to exposure-related triggers. It is crucial for healthcare providers to carefully evaluate patients and consider a wide range of potential causes when diagnosing eosinophilic pneumonia.
If you suspect eosinophilic pneumonia‚ seek medical advice promptly to identify the specific etiology and determine the most suitable treatment approach based on the underlying cause. Consulting a healthcare professional is vital for proper management and optimal outcomes in eosinophilic pneumonia cases.
Chronic Eosinophilic Pneumonia (CEP)
Chronic Eosinophilic Pneumonia (CEP) is a unique lung disorder characterized by the abnormal accumulation of eosinophils in the lung tissue. The etiology of CEP remains unknown‚ distinguishing it from other types of pneumonia. Despite its name‚ CEP does not always present as a chronic condition; it may manifest as an acute or subacute illness that recurs.
Individuals with CEP experience symptoms such as cough‚ shortness of breath‚ and fatigue‚ which may overlap with other respiratory conditions‚ making diagnosis challenging. To confirm CEP‚ healthcare providers often rely on a combination of clinical assessments‚ blood tests showing eosinophilia‚ imaging studies‚ and sometimes lung biopsy.
If you suspect you may have CEP or are experiencing persistent respiratory symptoms‚ seek medical attention for a thorough evaluation. Proper diagnosis and management of Chronic Eosinophilic Pneumonia are crucial to alleviate symptoms and prevent complications associated with this condition.
Idiopathic Acute Eosinophilic Pneumonia (AEP)
Idiopathic Acute Eosinophilic Pneumonia (AEP) is a rare but critical condition characterized by the rapid accumulation of eosinophils in the lungs‚ resulting in severe respiratory symptoms. Typically‚ AEP presents with acute respiratory failure and may progress rapidly if not promptly recognized and treated.
Patients with AEP often experience symptoms such as sudden onset dyspnea‚ cough‚ and fever. While the exact cause remains unclear‚ potential triggers may include inhalational exposures or certain medications. Prompt identification of AEP is crucial to initiating appropriate management‚ often involving corticosteroid therapy to address the eosinophilic infiltration in the lungs.
If you suspect you or a loved one may be suffering from AEP‚ seeking immediate medical attention is vital. Early diagnosis and intervention can greatly improve outcomes and prevent the progression of this serious respiratory condition.
Age and Gender Factors
Acute Eosinophilic Pneumonia most commonly affects individuals between the ages of 20 and 40‚ with a higher incidence in males compared to females‚ noted at a ratio of 2⁚1. Additionally‚ this condition predominantly emerges in individuals with no prior history of asthma‚ and smoking history may be implicated in causation.
Elderly patients with Chronic Eosinophilic Pneumonia are at risk as well‚ although the exact age range for its onset can vary. Being vigilant about symptoms and risk factors‚ especially in the specified age groups‚ can aid in the early detection and management of Eosinophilic Pneumonia‚ thereby improving treatment outcomes.
If you or someone you know falls within the susceptible age range and is experiencing respiratory symptoms‚ seeking medical attention promptly is crucial. Timely diagnosis and appropriate treatment can significantly impact the prognosis of Eosinophilic Pneumonia.
Diagnosis of Chronic Eosinophilic Pneumonia (CEP)
Diagnosing Chronic Eosinophilic Pneumonia (CEP) involves a comprehensive approach to confirm the condition accurately. Healthcare providers typically initiate the diagnostic process by conducting a thorough medical history review and physical examination‚ paying close attention to respiratory symptoms and possible risk factors.
Diagnostic tests for CEP often include blood tests to assess eosinophil levels‚ imaging studies such as chest X-rays or CT scans to visualize lung abnormalities‚ and pulmonary function tests to evaluate lung capacity and function. In some cases‚ a lung biopsy may be necessary to confirm the presence of eosinophils in the lung tissue.
Given the overlap of symptoms with other respiratory conditions‚ obtaining a correct diagnosis of CEP is crucial for initiating appropriate treatment strategies and managing the disease effectively. If you suspect CEP based on persistent respiratory symptoms‚ consult a healthcare professional for a comprehensive evaluation and diagnostic workup.
Symptoms of Acute Eosinophilic Pneumonia (AEP)
Acute Eosinophilic Pneumonia (AEP) typically presents with a sudden onset of severe respiratory symptoms. Patients with AEP may experience acute respiratory distress‚ shortness of breath‚ and cough. Other common symptoms include fever‚ chest pain exacerbated by deep breathing‚ and a general feeling of illness.
Recognizing the symptoms of AEP is crucial for prompt medical intervention as the condition can progress rapidly‚ leading to respiratory failure if left untreated. If you or someone you know is experiencing these symptoms‚ seeking immediate medical attention is essential for accurate diagnosis and effective management of Acute Eosinophilic Pneumonia.
Clinical Manifestations of Chronic Eosinophilic Pneumonia (CEP)
Chronic Eosinophilic Pneumonia (CEP) presents with a range of clinical manifestations that can vary in severity. Patients with CEP often experience persistent respiratory symptoms such as cough‚ dyspnea (shortness of breath)‚ and chest discomfort. Fatigue‚ weight loss‚ and night sweats may also accompany these respiratory complaints.
It is essential for individuals with suspected CEP to undergo a comprehensive evaluation by healthcare professionals to confirm the diagnosis. The chronic nature of CEP‚ characterized by recurrent acute episodes‚ necessitates close monitoring and appropriate management to alleviate symptoms and prevent long-term complications.
If you are experiencing respiratory symptoms consistent with CEP‚ seek medical attention for a thorough assessment and personalized treatment plan. Early diagnosis and intervention play a critical role in managing Chronic Eosinophilic Pneumonia effectively.
Diagnostic Criteria for Eosinophilic Pneumonia
Diagnosing Eosinophilic Pneumonia involves assessing histopathologic features‚ clinical symptoms‚ and ancillary tests. The diagnosis is established based on a combination of peripheral eosinophilia (elevated eosinophil count)‚ eosinophilic infiltration in lung tissues‚ and characteristic radiographic findings‚ such as pulmonary infiltrates.
Clinical manifestations‚ including cough‚ dyspnea‚ and chest pain‚ in combination with eosinophilia‚ guide clinicians towards suspecting Eosinophilic Pneumonia. Additionally‚ exclusion of other pulmonary diseases and potential triggers‚ such as infections or allergens‚ is essential in confirming the diagnosis.
If you experience respiratory symptoms suggestive of Eosinophilic Pneumonia‚ consult a healthcare professional for a comprehensive evaluation. Diagnosing this condition accurately is crucial for initiating appropriate treatment and managing the disease effectively.
Infectious and Non-Infectious Etiologies
Eosinophilic pneumonia can stem from various infectious and non-infectious causes. Infections by fungi like Pneumocystis jirovecii can trigger pneumonia‚ particularly in individuals with weakened immune systems. On the other hand‚ non-infectious triggers include allergic reactions to medications‚ exposure-related factors‚ and idiopathic etiologies.
Understanding the diverse etiologies of eosinophilic pneumonia is crucial for accurate diagnosis and targeted treatment. Healthcare professionals consider both infectious and non-infectious factors when evaluating patients with respiratory symptoms suggestive of eosinophilic pneumonia‚ emphasizing the importance of a comprehensive assessment to determine the underlying cause.
If you suspect eosinophilic pneumonia‚ seek medical advice promptly to identify the potential triggers and receive appropriate care tailored to the specific etiology contributing to the condition.
Treatment Options for Eosinophilic Pneumonia
The treatment of eosinophilic pneumonia depends on various factors‚ including the specific type and severity of the condition. In cases of idiopathic acute eosinophilic pneumonia (AEP)‚ prompt recognition and early corticosteroid therapy are essential to manage the rapid onset of respiratory distress and prevent further complications.
For chronic eosinophilic pneumonia (CEP)‚ treatment often involves corticosteroids to reduce eosinophilic inflammation in the lungs. Additionally‚ identifying and addressing potential triggers‚ such as allergens or environmental factors‚ plays a crucial role in managing eosinophilic pneumonia effectively.
Consulting with a healthcare provider is vital to determine the most appropriate treatment plan tailored to your specific condition and medical history. Follow-up monitoring and adjustments to the treatment regimen may be necessary to ensure optimal outcomes in eosinophilic pneumonia cases.
Prognosis and Complications
The prognosis for eosinophilic pneumonia varies depending on the type and severity of the condition‚ as well as the appropriateness of treatment. Idiopathic acute eosinophilic pneumonia (AEP) can lead to respiratory failure if left untreated‚ emphasizing the importance of early intervention for improved outcomes.
Complications of eosinophilic pneumonia may include respiratory distress‚ lung damage‚ and in severe cases‚ respiratory failure. Chronic eosinophilic pneumonia (CEP) might recur or become persistent‚ requiring ongoing management to prevent exacerbations and long-term complications.
Regular follow-ups and adherence to treatment plans are essential to monitor the condition‚ address any potential complications promptly‚ and optimize the prognosis for individuals with eosinophilic pneumonia. Seeking medical advice for any concerning symptoms or changes in the disease course is crucial for effective management and overall health.