Introduction to Microscopic Polyangiitis
Microscopic polyangiitis is a small vessel necrotizing vasculitis, part of a spectrum of disorders termed ANCA-associated vasculitides․
Microscopic polyangiitis is a subset of small vessel vasculitis conditions collectively known as ANCA-associated vasculitides, along with granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis․
Symptoms and Manifestations of Microscopic Polyangiitis
Microscopic polyangiitis causes inflammation of small blood vessels affecting various organs, leading to diverse symptoms․
Microscopic polyangiitis typically impacts vital organs such as the kidneys, lungs, nerves, skin, and joints due to inflammation of the small blood vessels running through them․
Definition and Classification
Microscopic polyangiitis is classified as an ANCA-associated vasculitis, affecting small blood vessels and commonly involving organs like kidneys, lungs, skin, and joints․
Commonly Affected Organs
Microscopic polyangiitis commonly affects vital organs such as the kidneys, lungs, nerves, skin, and joints due to inflammation of the small blood vessels supplying these tissues․
Causes and Risk Factors
No information available on the causes and risk factors of Microscopic Polyangiitis could be retrieved․
Key Diagnostic Procedures
Diagnosing microscopic polyangiitis involves a combination of clinical assessment, imaging studies, laboratory tests such as ANCA testing, renal and lung function tests, as well as tissue biopsies to confirm the presence of vasculitis and determine the extent of organ involvement․
Differential Diagnosis
When evaluating a patient for microscopic polyangiitis, it is crucial to differentiate it from other forms of small vessel vasculitis such as granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis, as well as ruling out alternative diagnoses like systemic lupus erythematosus, rheumatoid arthritis, and other autoimmune conditions that may present with similar symptoms․
Treatment Options for Microscopic Polyangiitis
Medication plays a crucial role in managing microscopic polyangiitis, including immunosuppressants, corticosteroids, and biologics targeting specific pathways involved in the disease process․
In treating microscopic polyangiitis, medical interventions include immunosuppressive medications to control inflammation, manage organ involvement, and prevent disease progression․ Corticosteroids are often used in combination with other immunosuppressants to achieve disease remission and improve the patient’s overall condition․
Medical Management
The medical management of microscopic polyangiitis involves the use of immunosuppressive medications to control inflammation, such as corticosteroids and other immunosuppressants, to help achieve and maintain disease remission․
Surgical Interventions
Surgical interventions are not typically used in the treatment of microscopic polyangiitis as the disease primarily involves small vessel inflammation and is managed with medical therapy․
Potential Long-Term Effects
Microscopic polyangiitis can lead to long-term complications such as chronic kidney disease, lung damage, nerve problems, skin ulcers, arthritis, and an increased risk of infections due to immune suppression required for treatment․
Impact on Quality of Life
Microscopic polyangiitis can significantly impact the quality of life due to chronic kidney disease, lung damage, nerve issues, and other complications, affecting daily activities and requiring ongoing management․
Epidemiology and Demographics
Microscopic polyangiitis is a rare condition affecting the kidneys, lungs, nerves, skin, and joints, commonly seen across various age groups and genders․
Prevalence of Microscopic Polyangiitis
The prevalence of microscopic polyangiitis is relatively rare, affecting a small percentage of the population globally, with sporadic cases reported across different regions․
Age and Gender Distribution
Microscopic polyangiitis can impact individuals of various ages and genders, with manifestations commonly affecting both men and women across different age groups․
Pathophysiology of Microscopic Polyangiitis
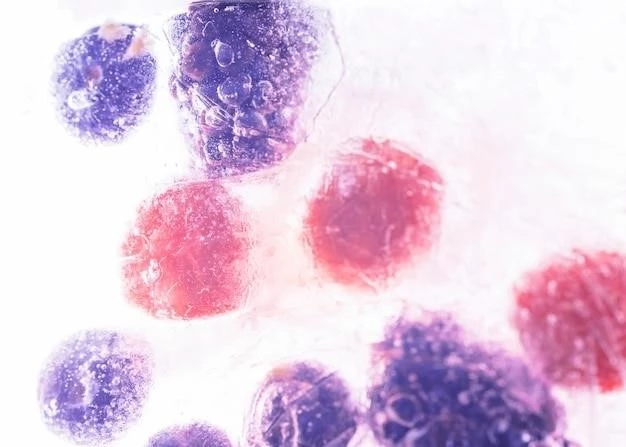
Microscopic polyangiitis involves small vessel inflammation and is associated with antineutrophil cytoplasmic autoantibodies (ANCA) targeting myeloperoxidase․
Autoimmune Mechanisms Involved
Microscopic polyangiitis is characterized by systemic vasculitis predominantly affecting small-caliber blood vessels and often associated with antineutrophil cytoplasmic autoantibodies (ANCAs) targeting specific proteins, contributing to the inflammatory process in the disease․
Role of Antineutrophil Cytoplasmic Antibodies (ANCAs)
Microscopic polyangiitis is closely associated with the presence of antineutrophil cytoplasmic autoantibodies (ANCAs), particularly those targeting myeloperoxidase (MPO), indicating an autoimmune component in the pathogenesis of the disease․ These antibodies contribute to the inflammation seen in small blood vessels and play a significant role in the pathophysiology of microscopic polyangiitis․
Recent Research and Advancements
Recent studies focus on further understanding the autoimmune mechanisms involved in microscopic polyangiitis, exploring potential targeted therapies to improve patient outcomes․
Innovations in Treatment Approaches
Ongoing research in the treatment of microscopic polyangiitis focuses on developing targeted therapies that aim to modulate the immune response more effectively, potentially leading to improved outcomes and reduced disease activity․
Emerging Therapies
Advancements in the treatment of microscopic polyangiitis include the exploration of novel targeted therapies and immunomodulators with the potential to enhance disease management and mitigate autoimmune responses associated with the condition․
Management Strategies for Patients with Microscopic Polyangiitis
Managing microscopic polyangiitis entails a comprehensive approach involving immunosuppressive therapy, monitoring, and supportive care to address organ damage and improve long-term outcomes․
Interdisciplinary Care Approach
Managing microscopic polyangiitis requires a multidisciplinary approach involving healthcare professionals from various fields collaborating to tailor treatment plans and provide holistic care to patients, addressing both medical and supportive needs․
Patient Education and Support
Providing patient education on microscopic polyangiitis is crucial to help individuals understand their condition, treatment options, and self-management strategies․ Support groups and resources can offer emotional support and a sense of community for those living with this rare disease․
Lifestyle Modifications and Self-Care Tips
Adopting a healthy lifestyle can complement medical treatment for microscopic polyangiitis․ Eating a balanced diet, regular exercise, stress management, and avoiding tobacco and excessive alcohol consumption can contribute to overall well-being and help manage the symptoms of the condition․

Coping with Microscopic Polyangiitis⁚ Psychological and Emotional Aspects
Living with microscopic polyangiitis can be emotionally challenging․ Supportive therapy and counseling can help manage psychological aspects and enhance coping strategies for individuals dealing with the impacts of the disease․
Mental Health Support
Individuals with microscopic polyangiitis may benefit from mental health support to address the emotional and psychological impact of living with a chronic autoimmune disease․ Counseling, therapy, and support groups can help manage anxiety, stress, and depression that may arise during the course of the illness․
Counseling and Therapy Options
Individuals with microscopic polyangiitis may benefit from counseling services and therapy options to address the emotional and psychological challenges that accompany managing a chronic autoimmune disease․ These interventions offer support in coping with the impact of the condition on mental well-being and overall quality of life․
Conclusion and Future Perspectives
In conclusion, microscopic polyangiitis is a complex autoimmune disease that requires a multi-faceted approach for management․ As research advances and new therapies emerge, the future holds promise for improved outcomes and quality of life for individuals living with this rare condition․
