Introduction
Hereditary fibrinogen Aα-Chain amyloidosis is a rare genetic disorder characterized by abnormal protein buildup leading to organ dysfunction.
Overview of Hereditary Fibrinogen Aα-Chain Amyloidosis
Hereditary fibrinogen Aα-Chain amyloidosis, a rare disorder, is caused by a genetic mutation leading to abnormal fibril formation. The Aα-chain of fibrinogen contributes to the buildup of amyloid fibrils, affecting various organs. This disorder is characterized by protein clumping in tissues and organs, impacting their normal functioning.
The symptoms of hereditary fibrinogen Aα-Chain amyloidosis vary depending on the affected organ, commonly involving the liver, kidneys, and nervous system. Diagnosis involves genetic testing to identify the specific mutation responsible for the disorder. Treatment options aim to manage symptoms and slow disease progression, focusing on supportive care and experimental therapies.
Understanding the Disease
Hereditary fibrinogen Aα-Chain amyloidosis involves abnormal fibril formation due to genetic mutation, leading to organ dysfunction.
Hereditary Aspect of the Disorder
Hereditary fibrinogen Aα-Chain amyloidosis is a genetic disorder stemming from mutations in the fibrinogen Aα-chain gene. This mutation results in the production of abnormal fibrinogen variants, leading to the formation of amyloid fibrils in various organs. The hereditary nature of the disorder means that it can be passed down from generation to generation within families, causing the manifestation of symptoms associated with organ dysfunction.
The transmission of the mutated gene follows an autosomal dominant pattern, where a single copy of the altered gene from either parent is adequate to cause the disorder. Understanding the hereditary aspect of this disease is crucial in both diagnosing affected individuals and studying the inheritance patterns for future therapeutic interventions. Genetic counseling plays a vital role in assessing the risk of passing on the mutation to offspring and in providing support to families affected by this rare disorder.
Role of Aα-Chain in Fibrinogen Amyloidosis
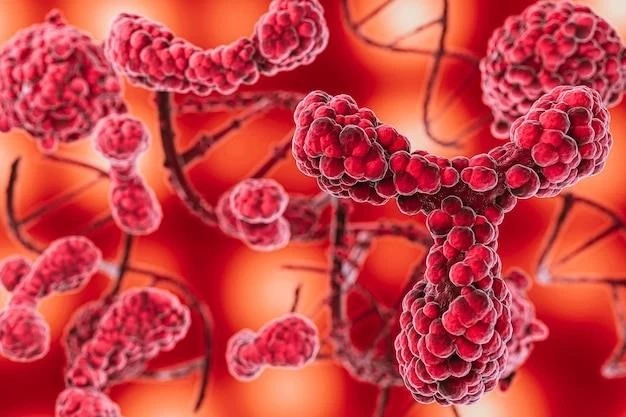
The Aα-chain is a critical component of fibrinogen that plays a central role in the pathogenesis of hereditary fibrinogen Aα-Chain amyloidosis. Mutations in the Aα-chain gene lead to the production of fibrinogen molecules with altered structures, prone to misfolding and aggregation.
These abnormal fibrinogen variants undergo a process where they transform into insoluble amyloid fibrils, accumulating in tissues and organs throughout the body. The deposition of amyloid fibrils disrupts normal organ function and contributes to the characteristic symptoms of the disorder.
Understanding the role of the Aα-chain in fibrinogen amyloidosis is essential for unraveling the molecular mechanisms underlying the disease and developing targeted therapeutic strategies to prevent or mitigate the harmful effects of amyloid buildup on vital organs.
Protein Buildup and Formation of Abnormal Fibrils
Hereditary fibrinogen Aα-Chain amyloidosis is characterized by the buildup of abnormal fibrinogen protein molecules due to genetic mutations. These mutated proteins have a propensity to misfold and aggregate, leading to the formation of amyloid fibrils.
The abnormal fibrils generated from the Aα-chain of fibrinogen accumulate in various tissues and organs, disrupting their normal structure and function. The presence of these amyloid deposits contributes to the development of organ dysfunction and the manifestation of symptoms associated with the disorder.
Understanding the process of protein buildup and aberrant fibril formation is crucial in elucidating the disease mechanisms and exploring potential therapeutic interventions aimed at reducing amyloid deposition and preserving organ integrity in individuals affected by hereditary fibrinogen Aα-Chain amyloidosis.
Symptoms and Diagnosis
Identifying symptoms and diagnostic methods are crucial in managing hereditary fibrinogen Aα-Chain amyloidosis effectively.
Identification of Symptoms in Patients
Recognizing the symptoms of hereditary fibrinogen Aα-Chain amyloidosis is essential for timely intervention. Patients may present with a range of manifestations depending on the affected organs, such as liver dysfunction, kidney involvement, or neurological symptoms.
Common signs include hepatomegaly, renal impairment, peripheral neuropathy, and cardiomyopathy. Additionally, patients may experience proteinuria, sensory deficits, and cardiac abnormalities. Timely recognition of these symptoms can prompt further evaluation and diagnosis, enabling early management strategies to alleviate the impact of the disorder on organ function.
Diagnostic Methods for Hereditary Fibrinogen Aα-Chain Amyloidosis
Diagnosing hereditary fibrinogen Aα-Chain amyloidosis involves a multimodal approach. Genetic testing plays a crucial role in identifying the specific mutation in the fibrinogen Aα-chain gene associated with the disorder.
Furthermore, imaging studies like MRI and CT scans can reveal amyloid deposits in affected organs. Biopsy of tissues showing suspected amyloid accumulation, such as the kidney or liver, is often performed to confirm the diagnosis definitively.
Laboratory tests assessing organ function, such as liver and kidney function tests, complement the diagnostic process. Combining these methods enables healthcare professionals to establish a comprehensive understanding of the disease presentation in individuals with hereditary fibrinogen Aα-Chain amyloidosis.
Genetic Mutation and Organ Dysfunction
The genetic mutation leads to protein abnormality causing organ dysfunction in hereditary fibrinogen Aα-Chain amyloidosis patients.
Impact of Genetic Mutation on Protein Production
The genetic mutation in hereditary fibrinogen Aα-Chain amyloidosis disrupts the normal production of fibrinogen proteins. This mutation results in the synthesis of abnormal fibrinogen variants with altered structures.
These mutated proteins have a higher propensity to misfold and aggregate, leading to the formation of amyloid fibrils. The increased production of these aberrant fibrils contributes to the pathological process underlying the disorder, causing organ dysfunction and associated symptoms.
Understanding the impact of genetic mutations on protein production is essential in elucidating the molecular basis of hereditary fibrinogen Aα-Chain amyloidosis and developing targeted interventions that aim to modulate protein synthesis and prevent the harmful consequences of amyloid accumulation on organ systems.
Organ Dysfunction Caused by Fibril Accumulation
In hereditary fibrinogen Aα-Chain amyloidosis, organ dysfunction arises from the accumulation of amyloid fibrils in various tissues. The deposition of these abnormal fibrils disrupts the normal architecture and function of affected organs.
Organ dysfunction can manifest differently based on the organs involved, such as liver impairment, renal insufficiency, or neurological deficits. The progressive buildup of amyloid fibrils contributes to tissue damage and ultimately leads to organ dysfunction, highlighting the debilitating nature of this rare disorder.
Understanding the mechanisms by which fibril accumulation causes organ dysfunction is crucial in developing targeted therapies aimed at preventing or reversing the detrimental effects of amyloid deposition on vital organ systems in individuals with hereditary fibrinogen Aα-Chain amyloidosis.
Treatment Options
Managing hereditary fibrinogen Aα-Chain amyloidosis involves current approaches to alleviate symptoms and ongoing research for future therapeutic advancements.
Current Approaches to Managing Hereditary Fibrinogen Aα-Chain Amyloidosis
Current treatment strategies for hereditary fibrinogen Aα-Chain amyloidosis focus on symptom management and supportive care. Therapeutic interventions aim to alleviate organ dysfunction and improve quality of life for affected individuals.
Common approaches may include medications to target specific symptoms, such as pain management for neuropathy or cardiac medications for cardiomyopathy. Additionally, supportive therapies like physical therapy or dietary modifications may complement the treatment plan.
Multidisciplinary care involving specialists in various fields, including genetics, nephrology, cardiology, and neurology, is crucial in providing comprehensive management for individuals with hereditary fibrinogen Aα-Chain amyloidosis. Ongoing research continues to explore novel treatment modalities to address the underlying mechanisms of the disorder and improve patient outcomes.
Research and Future Directions in Treating the Disorder
Ongoing research in hereditary fibrinogen Aα-Chain amyloidosis aims to explore novel therapeutic approaches and potential targeted interventions. Investigational studies focus on understanding the molecular pathways involved in fibril formation and organ damage, paving the way for precise treatment strategies.
Future directions include the development of gene-silencing techniques to modulate the expression of mutated fibrinogen genes, reducing amyloid production. Emerging therapies, such as gene editing or personalized medicine tailored to individual genetic profiles, hold promise in addressing the underlying cause of the disorder.
Clinical trials evaluating innovative treatments and disease-modifying therapies offer hope for improved outcomes and quality of life for patients with hereditary fibrinogen Aα-Chain amyloidosis. Collaborative efforts between researchers, healthcare professionals, and pharmaceutical companies are essential in advancing the field and translating scientific discoveries into effective clinical interventions.