Article Plan⁚ Disease, Peripheral Blood Vessel Disorder
Understanding Peripheral Vascular Disease (PVD)
Peripheral vascular disease (PVD) refers to a systemic disorder characterized by the narrowing of blood vessels located away from the heart or brain․ This condition typically stems from atherosclerosis, where fatty deposits build up within the arteries, leading to reduced blood flow․ PVD can affect arterial or venous vessels and often results in symptoms such as leg pain, numbness, or skin discoloration․
In PVD, decreased circulation to peripheral body parts occurs due to blocked or constricted blood vessels․ A primary cause is atherosclerosis, marked by the accumulation of plaque that narrows the arteries․ The condition progresses slowly over time, impacting various blood vessels like arteries, veins, or lymphatic vessels outside the heart․
Understanding the underlying mechanisms of PVD sheds light on its management and treatment options․ Individuals experiencing symptoms of PVD should seek medical attention promptly to prevent complications and improve their quality of life․
Causes of Peripheral Blood Vessel Disorders
Peripheral blood vessel disorders, including peripheral vascular disease (PVD), are often attributed to underlying conditions such as atherosclerosis․ This condition arises due to the build-up of plaque within the blood vessels, leading to narrowing and reduced blood flow․ Other potential causes of peripheral vascular disorders may include inflammatory diseases, blood vessel spasms, or trauma affecting the vessels․
It’s essential to recognize the risk factors that contribute to the development of these disorders․ Factors like smoking, diabetes, high blood pressure, and high cholesterol levels significantly increase the likelihood of developing peripheral blood vessel disorders․ Moreover, age, family history, and a sedentary lifestyle can also play a role in the onset of PVD․
Understanding the root causes of peripheral blood vessel disorders can prompt individuals to adopt healthier lifestyle choices and seek medical intervention when necessary․ By addressing these underlying causes and risk factors, the progression of the condition can potentially be slowed or even prevented․

Symptoms of Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD), arising from the narrowing of peripheral blood vessels, commonly manifests with symptoms indicative of reduced blood flow to the affected regions․ Individuals with PAD may experience leg pain or cramping during physical activity, known as intermittent claudication․ Other symptoms include numbness, weakness, or a feeling of coldness in one limb compared to the other․ Skin changes, slow wound healing, and hair loss on the legs may also signify PAD․
Recognizing these symptoms is crucial for early detection and management of PAD․ Individuals exhibiting these signs should consult a healthcare professional for a comprehensive evaluation and personalized treatment plan․ Timely intervention can help alleviate discomfort, improve mobility, and reduce the risks associated with peripheral artery disease․
Diagnosis of Peripheral Vascular Disease
Diagnosing peripheral vascular disease (PVD) often involves a combination of medical history review, physical examination, and specialized tests․ Healthcare providers may assess symptoms like leg pain, skin changes, or slow wound healing to suspect PVD․ Non-invasive tests such as ankle-brachial index (ABI) measurement, Doppler ultrasound, or magnetic resonance angiography can help evaluate blood flow and detect blockages․ In some cases, angiography or computed tomography (CT) scans may be utilized for a more detailed assessment of the blood vessels․
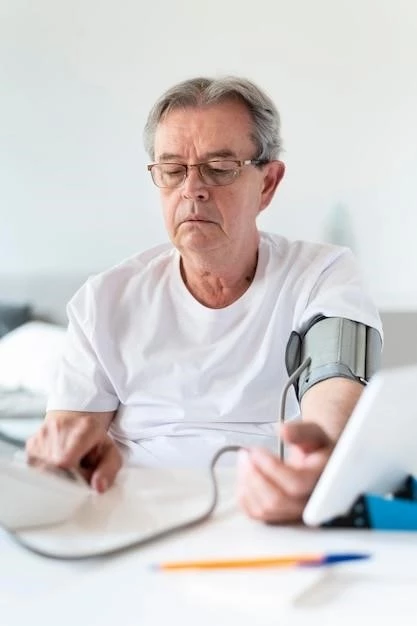
An early and accurate diagnosis of peripheral vascular disease is crucial for initiating timely treatment and preventing complications․ Individuals experiencing symptoms associated with PVD should promptly seek medical attention to undergo appropriate diagnostic evaluations tailored to their specific condition․ Effective diagnosis lays the foundation for personalized management strategies to improve quality of life and reduce the risks associated with peripheral artery disease․
Treatment Options for Peripheral Blood Vessel Disorders
When managing peripheral blood vessel disorders like peripheral vascular disease (PVD), treatment approaches aim to improve symptoms, enhance blood flow, and reduce complications․ Lifestyle modifications, including smoking cessation, a heart-healthy diet rich in fruits and vegetables, and regular exercise, play a crucial role in PVD management․ Medications such as antiplatelet agents, cholesterol-lowering drugs, and medications to address symptoms like leg pain may be prescribed․
In more severe cases, interventional procedures like angioplasty or stent placement may be recommended to restore blood flow in narrowed vessels․ Surgical interventions like bypass grafting can bypass blocked sections of arteries to improve circulation․ It is important for individuals with peripheral blood vessel disorders to adhere to their treatment plans, attend regular follow-ups, and communicate any changes in symptoms to their healthcare providers․
Lifestyle Changes to Manage Peripheral Artery Disease
Managing peripheral artery disease (PAD) involves incorporating healthy lifestyle changes to minimize symptoms and improve overall well-being․ Regular exercise, such as walking or cycling, can enhance circulation and reduce leg pain associated with PAD․ Following a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can aid in controlling cholesterol levels and promoting cardiovascular health․
Quitting smoking is paramount for individuals with PAD, as smoking exacerbates narrowing of blood vessels and increases the risk of complications․ Maintaining a healthy weight and managing conditions like diabetes and high blood pressure through proper medication adherence are essential components of PAD management․ By embracing these lifestyle modifications, individuals can better control their condition and enhance their quality of life․
Importance of Regular Exercise in Peripheral Vascular Disease
Regular exercise plays a crucial role in managing peripheral vascular disease (PVD) by promoting better blood flow and overall cardiovascular health․ Engaging in physical activity helps improve circulation, reduce leg pain, and increase stamina․ Walking, cycling, or swimming are excellent low-impact exercises that can benefit individuals with PVD․
Exercise helps strengthen muscles and may lower blood pressure and cholesterol levels, reducing the progression of PVD․ Moreover, physical activity can enhance overall well-being and quality of life for individuals living with peripheral vascular disease․ It is essential to consult healthcare providers to develop a safe and effective exercise regimen tailored to individual needs and abilities․
Dietary Recommendations for Individuals with Peripheral Blood Vessel Disorders
For individuals with peripheral blood vessel disorders, adopting a heart-healthy diet is essential to manage symptoms and promote vascular health․ Emphasize a diet rich in fruits, vegetables, whole grains, and lean proteins to maintain proper nutrition and support cardiovascular function․ Limit saturated fats, trans fats, and cholesterol to reduce plaque build-up in the arteries․
Focus on incorporating foods high in omega-3 fatty acids, such as fish, nuts, and seeds, to help lower inflammation and improve blood flow․ Additionally, consuming foods high in fiber can aid in controlling cholesterol levels and promoting digestive health․ Hydration is also key; aim to drink an adequate amount of water daily to support optimal circulation․
By prioritizing a well-rounded, nutrient-dense diet tailored to peripheral blood vessel disorders, individuals can positively impact their vascular health and overall well-being․
Medication Management for Peripheral Artery Disease
When it comes to peripheral artery disease (PAD), medication management is a key component of treatment․ Physicians may prescribe medications to address different aspects of the condition․ Antiplatelet drugs like aspirin or clopidogrel can reduce the risk of blood clots and improve blood flow․ Cholesterol-lowering medications such as statins help manage lipid levels, slowing the progression of atherosclerosis․
In some cases, medications to control blood pressure or blood sugar may be recommended to prevent complications and support overall cardiovascular health․ It is important for individuals with PAD to adhere to their prescribed medication regimen, report any side effects to their healthcare provider, and attend regular follow-up appointments for monitoring and adjustments as needed․
Surgical Interventions for Severe Cases of Peripheral Vascular Disease
For severe cases of peripheral vascular disease (PVD), surgical interventions may be necessary to restore proper blood flow and alleviate symptoms․ Procedures such as angioplasty with or without stenting can help widen narrowed arteries and improve circulation․ In more complex situations, bypass surgery may be recommended to reroute blood flow around blocked vessels․
These surgical interventions aim to address critical blockages and promote better blood flow to affected tissues․ It is essential for individuals undergoing these procedures to follow post-operative care instructions diligently, attend regular follow-ups, and maintain a healthy lifestyle to support optimal recovery and long-term vascular health․
Complications Associated with Untreated Peripheral Blood Vessel Disorders
Untreated peripheral blood vessel disorders can lead to significant complications due to reduced blood flow to vital organs and tissues․ In cases of advanced peripheral artery disease (PAD), individuals may face an increased risk of developing critical conditions such as limb ischemia, where insufficient blood supply causes tissue damage and can lead to gangrene․ Left untreated, PAD can also elevate the risk of cardiovascular events like heart attacks and strokes․
Moreover, untreated peripheral blood vessel disorders are associated with chronic pain, reduced mobility, and impaired quality of life․ It is crucial for individuals experiencing symptoms of peripheral artery disease or other vascular disorders to seek prompt medical attention to prevent the progression of the condition and avoid serious complications․
Research and Advancements in the Treatment of Peripheral Artery Disease
Ongoing research and advancements in the treatment of peripheral artery disease (PAD) focus on improving diagnostic techniques, enhancing treatment options, and exploring innovative therapies․ Studies are investigating the effectiveness of new medications, minimally invasive procedures, and advanced surgical techniques to address PAD․
Researchers are also exploring the role of personalized medicine in managing PAD, tailoring treatments to individual patient profiles for better outcomes․ Additionally, advancements in vascular imaging technologies and biomarker research are aiding in early detection and monitoring of PAD progression․
Staying informed about the latest research developments in PAD treatment can empower both healthcare providers and individuals with PAD to make informed decisions about care and explore cutting-edge therapies that may enhance quality of life and long-term vascular health․
Prevention Strategies for Peripheral Vascular Disease
Prevention is key when it comes to peripheral vascular disease (PVD)․ Adopting a healthy lifestyle can significantly reduce the risk of developing vascular disorders․ Maintaining a balanced diet low in saturated fats and cholesterol, rich in fruits, vegetables, whole grains, and lean proteins, can support heart health and prevent atherosclerosis, a common cause of PVD․
Regular physical activity is crucial for improving circulation and overall cardiovascular function, reducing the likelihood of vascular issues․ Avoiding tobacco products and managing conditions like high blood pressure and diabetes through proper medication and lifestyle adjustments are essential preventive measures․
By prioritizing a heart-healthy lifestyle, individuals can proactively protect their vascular health and reduce the chances of developing peripheral blood vessel disorders․ Regular check-ups with healthcare providers for screenings and early detection are also vital for preemptive intervention․
