Chromomycosis⁚ Understanding the Fungal Infection
Chromomycosis, caused by certain fungi, presents challenges due to its slow progression and varied symptoms. Understanding the causes, such as traumatic implantation of fungi, is crucial for early diagnosis and effective treatment.
Causes of Chromomycosis
Chromomycosis is primarily caused by fungi belonging to the order Chaetothyriales, often found in soil and decaying vegetation. The infection occurs when these fungi enter the skin through wounds or cuts. Additionally, exposure to contaminated environments can increase the risk of contracting the disease.
Specifically, the following factors contribute to the development of chromomycosis⁚
- Fungal Entry⁚ Traumatic implantation of fungi through skin injuries.
- Environmental Exposure⁚ Working or living in areas with high fungal concentrations.
- Weakened Immune System⁚ Individuals with compromised immunity are more susceptible.
- Occupational Hazards⁚ Certain occupations like farming or forestry may involve frequent exposure to fungi.
Understanding these causes is essential for implementing preventive measures and educating individuals on risk factors associated with chromomycosis.
Symptoms and Diagnosis of Chromomycosis
Chromomycosis manifests with distinct symptoms, including skin lesions that may vary in appearance from nodules to ulcers. These lesions are often slow-growing and can be discolored, ranging from brown to black. Other common symptoms include itching, swelling, and scarring of the affected area.
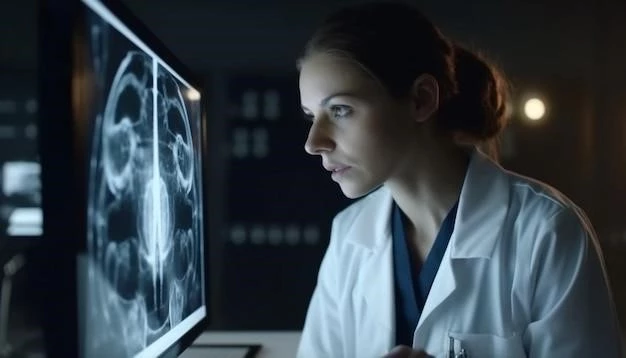
Diagnosing chromomycosis involves a physical examination and may require laboratory tests, such as skin scrapings or biopsies to identify the specific fungi causing the infection. Additionally, imaging studies like X-rays or MRIs can help assess the extent of tissue involvement.
Healthcare providers must differentiate chromomycosis from other skin conditions with similar symptoms to ensure accurate diagnosis. Early identification is crucial for initiating appropriate treatment and preventing potential complications associated with the infection.

Treatment Options for Chromomycosis
Treating chromomycosis involves a multidisciplinary approach that may include antifungal medications, surgical interventions, and wound care. The choice of treatment depends on the severity of the infection, the extent of tissue involvement, and the patient’s overall health.
Common treatment options for chromomycosis include⁚
- Antifungal Therapy⁚ Oral antifungal medications such as itraconazole or terbinafine are often prescribed to combat the fungal infection.
- Surgical Excision⁚ In cases of extensive lesions, surgical removal of infected tissues may be necessary to prevent spread and promote healing.
- Cryosurgery⁚ Cryotherapy using extreme cold can be employed to destroy fungal tissue.
- Topical Treatments⁚ Antifungal creams or ointments may be used for localized infections.
It is essential for healthcare providers to closely monitor patients during treatment to ensure efficacy and manage any potential side effects. Combining different treatment modalities tailored to each individual case can improve outcomes and reduce the risk of disease recurrence.
Prevention Strategies for Chromomycosis
Preventing chromomycosis involves implementing various strategies to reduce the risk of fungal infections, particularly in individuals who are frequently exposed to outdoor environments or working with soil and decaying vegetation. Educati0ng individuals on preventive measures is crucial in minimizing the incidence of this infection.
Key prevention strategies for chromomycosis include⁚
- Protective Clothing⁚ Wearing appropriate clothing, including gloves and boots, when working in areas where fungal exposure is likely.
- Skin Hygiene⁚ Maintaining good skin hygiene, promptly cleaning and covering any wounds or cuts to prevent fungal entry;
- Environmental Precautions⁚ Avoiding direct contact with soil or plant material known to harbor fungi.
- Occupational Safety⁚ Implementing workplace safety guidelines to minimize exposure to fungi for individuals in high-risk occupations.
By following these preventive strategies and remaining vigilant about potential sources of fungal contamination, individuals can significantly reduce their chances of developing chromomycosis. Early prevention is key in avoiding the onset of this challenging fungal infection.
Complications of Chromomycosis
Chromomycosis can lead to various complications, especially if left untreated or if the infection spreads to deeper tissues. These complications may result in prolonged morbidity and may require more aggressive treatment approaches to manage effectively.
Common complications associated with chromomycosis include⁚
- Secondary Infections⁚ The presence of open skin lesions can increase the risk of secondary bacterial infections.
- Scarring and Disfigurement⁚ Severe cases of chromomycosis may result in significant scarring and permanent changes to the affected skin.
- Localized Spread⁚ Fungal infection can spread to nearby tissues, leading to deeper involvement and more complex treatment requirements.
- Chronic Inflammation⁚ Prolonged inflammation in the affected area can cause discomfort and delayed healing.
Addressing these complications requires a comprehensive approach that may involve a combination of antifungal therapy, surgical interventions, and wound care to prevent further progression of the infection and mitigate potential long-term effects on the patient’s health and well-being;
Epidemiology of Chromomycosis
Chromomycosis is a rare fungal infection that predominantly affects individuals living in tropical and subtropical regions, particularly in rural areas with high humidity and warm climates. The epidemiology of chromomycosis reflects the environmental conditions conducive to fungal growth and human exposure.
Key points regarding the epidemiology of chromomycosis include⁚
- Geographical Distribution⁚ The highest incidence of chromomycosis is reported in regions of Africa, Asia, and certain parts of the Americas.
- Occupational Risk⁚ Agricultural workers, farmers, and individuals with outdoor occupations are at higher risk due to frequent contact with soil and decaying vegetation.
- Age and Gender⁚ Chromomycosis can affect individuals of all ages and genders, although certain age groups may be more vulnerable.
- Seasonal Variation⁚ The infection may exhibit seasonal patterns corresponding to environmental factors influencing fungal presence.
Understanding the epidemiology of chromomycosis is essential for developing targeted prevention strategies, raising awareness among high-risk populations, and improving diagnostic and treatment protocols to better address the challenges associated with this fungal infection.
Research and Developments in Chromomycosis
Ongoing research and developments in the field of chromomycosis focus on enhancing diagnostic methods, exploring novel treatment modalities, and investigating the genetic and environmental factors that contribute to the disease’s progression. Collaborative efforts among clinicians, researchers, and public health professionals play a crucial role in advancing our understanding and management of this challenging fungal infection.
Some key areas of research and developments in chromomycosis include⁚
- Genetic Studies⁚ Investigating genetic susceptibility to chromomycosis to identify individuals at higher risk of developing the infection.
- Antifungal Therapies⁚ Evaluating the efficacy of new antifungal agents and combination therapies for improved treatment outcomes.
- Vaccine Development⁚ Exploring the potential for vaccine development to prevent chromomycosis in high-risk populations.
- Environmental Investigations⁚ Studying the ecology of fungal species causing chromomycosis to better understand transmission patterns.
By fostering innovation and continuous research efforts, the scientific community aims to advance our knowledge of chromomycosis, enhance patient care, and ultimately reduce the burden of this fungal infection on global health.
Case Studies of Chromomycosis
Examining case studies of chromomycosis provides valuable insights into the diverse presentations of the fungal infection, treatment outcomes, and challenges encountered in clinical practice. These real-life scenarios offer clinicians and researchers an opportunity to learn from individual patient experiences and tailor management strategies accordingly.
Some notable case studies of chromomycosis include⁚
- Case 1⁚ A 45-year-old farmer presenting with multiple nodular skin lesions on the lower extremities, successfully treated with a combination of oral antifungal therapy and surgical excision.
- Case 2⁚ A 60-year-old outdoor worker with chronic ulcers infected with black fungi, demonstrating the importance of early diagnosis and wound care in preventing complications.
- Case 3⁚ A pediatric patient with a rare disseminated form of chromomycosis, highlighting the need for specialized pediatric care and long-term follow-up.
- Case 4⁚ A case of chromomycosis recurrence post-surgical excision٫ underscoring the challenges of managing persistent infections and the importance of long-term monitoring.
By analyzing these case studies, healthcare professionals can enhance their understanding of chromomycosis, refine diagnostic and treatment approaches, and contribute to the collective knowledge aimed at improving patient outcomes and quality of care for individuals affected by this fungal infection.