Abdominal Pain
Abdominal Pain is a common symptom of colonic malakoplakia, characterized by discomfort or cramping in the abdominal region․
Change in Bowel Habits
Colonic malakoplakia may lead to alterations in bowel habits, such as constipation, diarrhea, or changes in stool consistency․
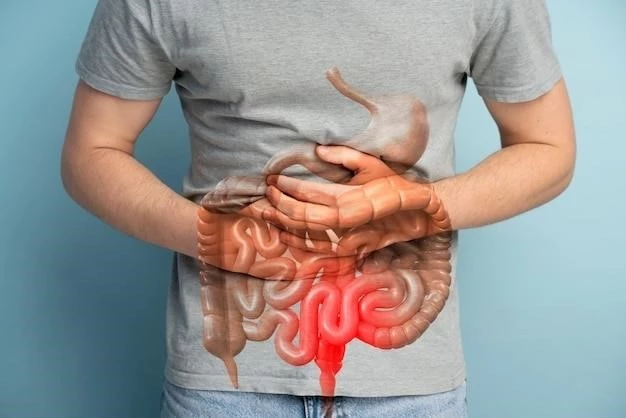
Blood in Stool
Blood in stool is a potential symptom of colonic malakoplakia, indicating possible inflammation or damage in the colon requiring medical attention․
Immunodeficiency
Immunodeficiency can increase the risk of colonic malakoplakia by impairing the body’s immune response against bacterial infections in the colon․
Bacterial Infection
Bacterial infections, particularly those caused by certain bacteria like Escherichia coli, have been linked to the development of colonic malakoplakia․
Genetic Factors
Genetic factors can play a role in the susceptibility to colonic malakoplakia, influencing how the immune system responds to bacterial triggers in the colon․
Colonoscopy
Colonoscopy is a key diagnostic procedure for colonic malakoplakia, allowing direct visualization of the colon’s internal structures and abnormalities․
Biopsy
A biopsy of abnormal colon tissue is crucial for diagnosing colonic malakoplakia, providing detailed information on cellular changes and confirming the condition․
Imaging Tests
Imaging tests like CT scans or MRIs are used in diagnosing colonic malakoplakia to visualize the colon and detect any abnormalities or lesions present․
Antibiotics
Antibiotics are commonly prescribed to treat colonic malakoplakia by targeting the underlying bacterial infection contributing to the condition․
Surgical Intervention
Surgical intervention may be necessary for colonic malakoplakia cases with severe complications or when conservative treatments are ineffective in resolving the condition․
Immunomodulatory Therapy
Immunomodulatory therapy is employed in some cases of colonic malakoplakia to regulate the immune response and help control inflammation in the colon․
Unique Symptoms in Children
Children with colonic malakoplakia may exhibit distinct symptoms such as growth delays, recurrent fevers, and failure to thrive, requiring specialized pediatric care․
Treatment Approaches for Pediatric Patients
Treatment of colonic malakoplakia in children may involve a combination of antibiotics, surgical intervention, and immunomodulatory therapy tailored to the child’s age and health needs․
Obstruction
Colonic malakoplakia can lead to bowel obstruction, a serious complication where the normal flow of stool is blocked within the colon, necessitating prompt medical intervention․
Fistula Formation
Colonic malakoplakia can result in fistula formation, where abnormal connections develop between the colon and nearby structures, leading to complications like infections or abscesses․
Maintaining a Healthy Immune System
Strengthening the immune system through a balanced diet, regular exercise, and adequate rest can support the prevention of colonic malakoplakia and other infections․
Proper Hygiene Practices
Adhering to good hygiene practices like washing hands regularly, maintaining cleanliness, and avoiding exposure to harmful bacteria can help prevent colonic malakoplakia and related complications․
Current Studies
Current studies on colonic malakoplakia focus on understanding its pathogenesis, exploring novel treatment approaches, and evaluating the long-term outcomes of different interventions․
Future Directions
Future research on colonic malakoplakia aims to develop targeted therapies, improve diagnostic methods, and enhance our understanding of the condition’s underlying mechanisms for better management and outcomes․
