Disease ⸺ Dysplasia
Dysplasia refers to the abnormal development or growth of cells within a tissue. It involves atypical cellular formation, often caused by mutations. This article aims to provide a comprehensive overview of dysplasia, including its causes, progression, detection, pre-cancerous nature, treatment options, prognosis, risk factors, and ongoing research in the field.
Introduction to Dysplasia
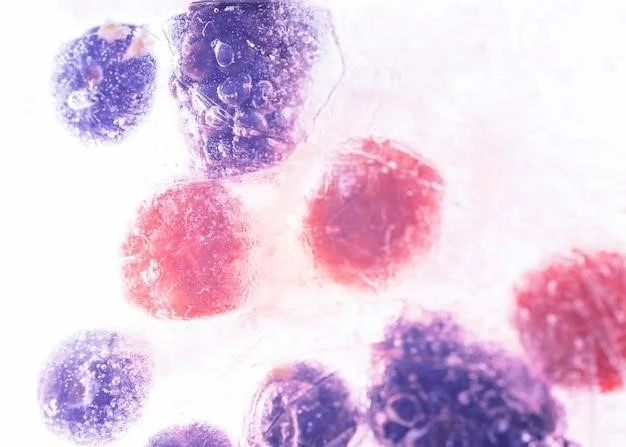
Dysplasia is a condition characterized by the presence of abnormal cells within a tissue. These cells often display distorted growth patterns and development, differing from the typical architecture of the tissue. Dysplasia can occur in various organs and is linked to genetic mutations or other factors leading to cellular malfunction. Understanding dysplasia is crucial as it can progress to pre-cancerous stages if left untreated.
When dysplastic cells are examined under a microscope, they are notably irregular and show signs of disordered growth. This anomaly in cellular structure can impede normal tissue function and pose a risk for further progression into cancer if not addressed promptly. Dysplasia is a warning sign of potential issues within the body and should be carefully monitored and managed by healthcare professionals.
It is important to distinguish dysplasia from healthy tissue to prevent the potential spread of abnormal cells. The identification of dysplastic changes enables healthcare providers to intervene early, potentially preventing the formation of cancerous lesions. By understanding the fundamentals of dysplasia, healthcare professionals can implement appropriate diagnostic and treatment strategies to manage this abnormal cellular growth effectively.
Understanding Cells and Tissue
In the context of dysplasia, a fundamental understanding of normal cellular and tissue structure is crucial. Cells are the basic building blocks of living organisms, each with specific functions that contribute to the overall function of tissues and organs. Tissues, on the other hand, are groups of cells that work together to perform specialized functions.
Healthy cells undergo a regulated process of growth, division, and eventual death, known as apoptosis. This controlled cycle ensures that tissues maintain their integrity and function properly. However, in dysplasia, this process is disrupted, leading to the development of abnormal cells that exhibit irregular growth patterns.
Cells in dysplasia often manifest mutations in their genetic material, causing them to proliferate uncontrollably and form atypical structures within the tissue. These distorted cells may lose their ability to function normally and can potentially progress to more severe stages if not addressed.
Understanding the characteristics of normal cells and tissues is essential for recognizing the subtle changes that occur in dysplasia. By identifying these aberrant cellular developments early on, healthcare professionals can intervene effectively to prevent further complications and the potential advancement to cancerous stages. Through continued research and observation, the intricate relationship between cellular dynamics and dysplasia can be further elucidated, ultimately improving diagnostic and therapeutic approaches for this condition.
Causes of Dysplasia
The development of dysplasia can be attributed to various factors, with genetic mutations playing a significant role in initiating abnormal cellular growth. Mutations in specific genes responsible for cell cycle regulation, DNA repair, and cell differentiation can lead to the malfunction of normal cellular processes.
Environmental factors such as exposure to carcinogens, chronic inflammation, or infections may also contribute to the onset of dysplasia; These external influences can disrupt the usual cellular environment and promote the formation of atypical cells within tissues.
Additionally, certain lifestyle habits like smoking, poor nutrition, and sedentary behavior can predispose individuals to dysplasia by compromising the body’s ability to maintain cellular homeostasis. These factors create an environment conducive to the development of abnormal cellular growth and impaired tissue function.
Furthermore, age-related changes and cumulative damage to cells over time can increase the likelihood of dysplasia. As individuals grow older, the body’s mechanisms for regulating cell growth and repair may become less efficient, leading to a higher susceptibility to cellular abnormalities.
Understanding the multifactorial nature of dysplasia is essential in identifying at-risk populations and implementing preventative measures to reduce the incidence of this condition. By addressing both genetic and environmental contributors to dysplasia, healthcare professionals can work towards mitigating the factors that drive abnormal cellular growth and tissue dysfunction.
Types of Dysplasia
Dysplasia can manifest in various forms depending on the affected tissue or organ. Epithelial dysplasia, for example, involves abnormal cellular changes in the epithelial tissue lining organs like the skin, lungs, or digestive tract. This type of dysplasia is commonly associated with pre-cancerous conditions and requires careful monitoring.
Skeletal dysplasia pertains to abnormalities in bone development, leading to skeletal deformities and growth irregularities. Conditions such as dwarfism and osteogenesis imperfecta fall under this category of dysplasia, impacting the structural integrity of the skeletal system;
Renal dysplasia affects the development of the kidneys, resulting in malformations in the renal tissue that can impair kidney function and lead to complications such as hypertension or renal failure. Early detection and intervention are essential in managing renal dysplasia to prevent further damage to the kidneys.
Furthermore, fibrous dysplasia involves the abnormal growth of fibrous tissue within bones, causing pain, deformity, and increased fracture risk. This type of dysplasia can affect multiple bones in the body and may require surgical intervention to alleviate symptoms and restore bone function.
Understanding the distinct types of dysplasia is essential for accurate diagnosis and tailored treatment strategies. Healthcare professionals must be familiar with the presentations and implications of different dysplasia types to provide appropriate care and management for individuals affected by these conditions.
Progression of Dysplasia
The progression of dysplasia involves a continuum of cellular changes that can evolve from mild abnormalities to more severe, pre-cancerous states if left unchecked. Initially, dysplastic cells exhibit subtle structural alterations and irregular growth patterns within the tissue.
As dysplasia advances, the cellular atypia becomes more pronounced, with cells displaying increased distortion and potential loss of normal function. This progression may be accompanied by a higher proliferation rate of abnormal cells, further compromising the integrity of the tissue.
If dysplasia continues to progress unchecked, it can transition into a pre-cancerous stage where the risk of developing cancerous lesions significantly rises. At this critical juncture, early detection and intervention are paramount in preventing the further advancement of abnormal cellular growth into malignancy.
The progression of dysplasia is influenced by various factors, including the underlying cause of the condition, the affected tissue or organ, genetic predispositions, and environmental influences. Monitoring the progression of dysplasia through regular screenings and diagnostic tests is essential in managing the condition effectively and minimizing the risk of malignant transformation.
Understanding the progressive nature of dysplasia underscores the importance of timely intervention and vigilance in detecting and addressing abnormal cellular changes. By closely monitoring the evolution of dysplasia, healthcare professionals can implement targeted treatment strategies to halt its progression and reduce the likelihood of malignant development.
Detection and Diagnosis
The detection and diagnosis of dysplasia involve a comprehensive approach that combines various screening methods and diagnostic techniques. Healthcare providers may utilize imaging studies such as X-rays, CT scans, or MRIs to visualize abnormal tissue growth in affected organs. These imaging modalities help identify structural changes indicative of dysplasia.
Biopsies are essential in confirming the presence of dysplastic cells within a tissue. During a biopsy, a small sample of the affected tissue is obtained and examined under a microscope to assess cellular morphology and identify any abnormalities. This microscopic analysis provides valuable insights into the nature and extent of dysplasia present.
In addition to imaging studies and biopsies, genetic testing may be employed to detect specific mutations or genetic markers associated with dysplasia. Understanding the genetic underpinnings of dysplasia can aid in risk assessment, personalized treatment planning, and monitoring disease progression.
Clinical assessments and screenings play a vital role in the early detection of dysplasia. Regular check-ups with healthcare providers allow for the monitoring of symptoms and the identification of any subtle changes that may indicate the presence of abnormal cellular growth. Healthcare professionals rely on a combination of patient history, physical examinations, and diagnostic tests to accurately diagnose dysplasia and initiate appropriate management strategies.
Timely and accurate detection of dysplasia is crucial in facilitating prompt intervention and preventing the progression of abnormal cellular changes. By employing a multidisciplinary approach to detection and diagnosis, healthcare teams can effectively identify dysplasia and tailor treatment plans to address the specific needs of individual patients.
Pre-Cancerous Nature of Dysplasia
Dysplasia’s pre-cancerous nature signifies its potential to progress into malignancy if left untreated. The presence of abnormal cellular growth and atypical tissue formation in dysplasia can serve as a precursor to the development of cancerous lesions.
Pre-cancerous dysplastic changes indicate an increased risk of further malignant transformation within the affected tissue or organ. Cells exhibiting dysplastic features have a higher likelihood of acquiring additional genetic mutations that drive the progression towards cancer.
Healthcare professionals consider dysplasia a critical warning sign of impending cancer and prioritize early intervention to prevent the advancement to malignancy. Through regular monitoring and timely treatment, the transition from pre-cancerous dysplasia to invasive cancer can be potentially averted.
Screening protocols and surveillance strategies are crucial in identifying pre-cancerous dysplastic changes in high-risk individuals or populations. Early detection of dysplasia allows for the implementation of preventive measures and tailored treatment approaches to mitigate the risk of cancer development.
Recognizing the pre-cancerous nature of dysplasia underscores the importance of proactive healthcare management and ongoing monitoring to intervene at the earliest stages of abnormal cellular growth. By addressing dysplasia in its pre-cancerous state, healthcare providers can significantly impact patient outcomes and reduce the burden of cancer incidence.
Symptoms of Dysplasia
Dysplasia typically does not present with specific symptoms that are easily recognizable by individuals. In many cases, dysplasia is asymptomatic and is often incidentally discovered during routine screenings or evaluations for other health concerns. The absence of overt symptoms makes it challenging to detect dysplasia based on clinical presentation alone.
However, in some instances, depending on the affected organ or tissue, individuals may experience subtle signs that could indicate the presence of dysplasia. These symptoms can vary and are usually nonspecific, such as localized pain, changes in bowel habits, abnormal bleeding, or unexplained weight loss.
In skeletal dysplasia, individuals may exhibit abnormal skeletal growth, disproportionate limb lengths, or bone deformities that can be visually apparent. Renal dysplasia, on the other hand, may manifest as kidney-related symptoms like high blood pressure, urinary changes, or swelling in the extremities.
It is important to note that the symptoms of dysplasia are often mild or mimic other benign conditions, making accurate diagnosis challenging without further evaluation. Due to the lack of specific symptoms associated with dysplasia, healthcare providers rely on diagnostic tests and screenings to identify abnormal cellular changes within tissues.
Recognizing the subtle or nonspecific symptoms of dysplasia underscores the importance of regular health check-ups and screening evaluations to detect potential abnormalities early. Early detection allows for prompt intervention and management of dysplasia before it progresses to more severe stages or complications.
Treatment Options
The management of dysplasia involves a multifaceted approach aimed at addressing the underlying causes of abnormal cellular growth and preventing the progression to more severe stages, including cancer. Treatment options for dysplasia may vary depending on the location and extent of the dysplastic changes within the body.
One common treatment modality for dysplasia is the removal of dysplastic tissues through surgical procedures such as excision or resection; Surgical intervention aims to eliminate affected cells and tissues to prevent further development of dysplasia or mitigate the risk of cancerous transformation.
In cases where dysplasia is widespread or affects internal organs, minimally invasive procedures such as endoscopic interventions or laser therapy may be utilized to target and remove abnormal tissue while preserving healthy surrounding structures. These minimally invasive approaches often result in quicker recovery times and reduced risk of complications.
Medical interventions, including pharmacological treatments, may be prescribed to target specific pathways or cellular processes contributing to dysplasia. Medications aimed at controlling cell proliferation, promoting apoptosis, or modulating immune responses can be employed to manage dysplasia and inhibit further abnormal growth.
Furthermore, close monitoring and surveillance through regular screenings and follow-up appointments are essential components of dysplasia management. Monitoring allows healthcare providers to track the progression of dysplasia, assess treatment efficacy, and intervene promptly if there are signs of disease advancement.
The selection of treatment options for dysplasia is individualized based on the patient’s overall health status, the severity of dysplastic changes, and the potential risk of progression to cancer. By combining surgical, medical, and monitoring strategies, healthcare teams can effectively manage dysplasia and improve patient outcomes.
Prognosis and Outcomes
The prognosis for individuals with dysplasia depends on various factors, including the type, location, and extent of the abnormal cellular changes, as well as the effectiveness of treatment interventions. In many cases, if dysplasia is detected early and managed promptly, the prognosis is generally favorable with a low risk of progression to cancer.
Individuals with mild dysplasia or those who undergo successful surgical removal of dysplastic tissues often have excellent outcomes, with a reduced likelihood of recurrence or complications. Regular monitoring and screenings are essential for tracking the progression of dysplasia and ensuring timely intervention if needed.
However, in instances where dysplasia is more extensive, involves critical organs, or has progressed to pre-cancerous stages, the prognosis may be less favorable. Close collaboration between healthcare providers and patients is crucial in developing tailored treatment plans and monitoring strategies to optimize outcomes and minimize the risk of disease advancement.
It is important for individuals diagnosed with dysplasia to follow their healthcare team’s recommendations regarding treatment, surveillance, and lifestyle modifications to improve prognosis and overall well-being. Compliance with follow-up appointments and screenings plays a significant role in identifying any recurrence or progression of dysplastic changes early.
By actively engaging in their healthcare management, individuals with dysplasia can positively impact their prognosis and outcomes. Through a comprehensive and proactive approach that integrates treatment, monitoring, and lifestyle adjustments, patients can work towards optimizing their health and reducing the long-term effects of dysplasia.
Risk Factors
Several risk factors contribute to the development and progression of dysplasia, increasing the likelihood of abnormal cellular growth and tissue changes. Genetic predisposition plays a significant role, with inherited mutations in specific genes predisposing individuals to dysplastic conditions.
Environmental factors such as exposure to carcinogens, toxins, or radiation can also heighten the risk of dysplasia by causing DNA damage and cellular dysfunction. Chronic inflammatory conditions, infections, and autoimmune disorders may create an inflammatory microenvironment conducive to dysplastic changes within tissues.
Lifestyle habits and behaviors, including smoking, excessive alcohol consumption, poor dietary choices, and sedentary lifestyles, are additional risk factors associated with dysplasia. These factors can impact cellular health and contribute to the initiation and progression of abnormal cellular growth.
Age-related changes and cumulative cellular damage over time are also risk factors for dysplasia, as the body’s natural mechanisms for maintaining cellular integrity may become less efficient with aging. Older individuals may be more susceptible to dysplasia due to a higher burden of genetic alterations and cellular stress.
Understanding the multifaceted nature of risk factors for dysplasia is crucial in identifying at-risk populations and implementing preventive measures to reduce the incidence of this condition. By addressing genetic, environmental, and lifestyle factors that contribute to dysplasia, healthcare providers can empower individuals to make informed choices that promote cellular health and reduce the risk of abnormal cellular growth.
Research and Advances
Ongoing research in the field of dysplasia is pushing the boundaries of knowledge and expanding the understanding of abnormal cellular growth and its implications. Advanced imaging technologies, such as high-resolution microscopy and molecular imaging, are shedding light on the intricate cellular changes associated with dysplasia.
Genomic studies are unraveling the genetic underpinnings of dysplasia, identifying key mutations and signaling pathways that drive abnormal cellular growth. By elucidating the molecular mechanisms underlying dysplasia, researchers are paving the way for targeted therapies and precision medicine approaches tailored to individual patients.
Novel biomarkers and diagnostic tools are being developed to improve the early detection of dysplasia and enhance precision in diagnosing this condition. Biomarker panels that reflect specific genetic alterations or cellular biomarkers associated with dysplasia hold promise for more accurate and timely diagnosis.
Advancements in treatment modalities, such as targeted therapies, immunotherapies, and gene-editing techniques, are revolutionizing the management of dysplasia. These innovative approaches aim to target dysplastic cells specifically while minimizing damage to healthy tissues, offering new avenues for personalized and effective treatment strategies;
Clinical trials and collaborative research efforts are instrumental in evaluating the safety and efficacy of emerging treatments for dysplasia. By participating in clinical studies, patients have the opportunity to access cutting-edge therapies and contribute to the advancement of dysplasia management.
In conclusion, dysplasia represents a complex condition characterized by atypical cellular growth and abnormal tissue formation. Understanding the causes, progression, detection, and treatment of dysplasia is paramount in addressing this disorder effectively.
The pre-cancerous nature of dysplasia underscores the importance of early detection and intervention to prevent the development of malignant lesions. By recognizing the subtle symptoms, implementing regular screenings, and utilizing advanced diagnostic techniques, healthcare providers can identify dysplastic changes early and initiate timely treatment.
Treatment options for dysplasia encompass a range of surgical, medical, and monitoring strategies tailored to the individual needs of patients. By combining these approaches and emphasizing proactive healthcare management, favorable outcomes and reduced risks of disease progression can be achieved.
Ongoing research and advances in the field of dysplasia offer promising opportunities for enhanced diagnostics, targeted therapies, and personalized medicine. By leveraging innovative technologies and collaborative efforts, the future of dysplasia management holds great potential for improving patient care and outcomes.
In closing, a comprehensive approach that integrates early detection, individualized treatment, and continuous monitoring is essential in effectively managing dysplasia. By prioritizing a proactive stance towards healthcare and staying informed about advances in the field, individuals and healthcare providers can work together to address dysplasia and promote overall well-being.