Hyperimmunoglobulinemia E
Hyperimmunoglobulinemia E is a rare condition characterized by elevated IgE levels, leading to hyperreactivity to antigens. Understanding the role of immunoglobulins in the body is crucial in managing this disorder. Stay tuned to learn more about its relationship with atopic dermatitis, allergies, asthma, eczema, pruritus, mast cells, basophils, anaphylaxis, and immunodeficiency.
Introduction to Hyperimmunoglobulinemia E
Hyperimmunoglobulinemia E, also known as Job syndrome, is a rare immune disorder characterized by elevated levels of Immunoglobulin E (IgE) in the blood. IgE is a type of antibody produced by the immune system in response to allergens. In individuals with hyperimmunoglobulinemia E, the increased IgE levels lead to hyperreactivity to various antigens, triggering allergic responses.
People with this condition often present with symptoms such as atopic dermatitis, allergies, asthma, eczema, pruritus (itching), and dermatitis. Understanding the underlying mechanisms of hyperimmunoglobulinemia E is essential for proper diagnosis and management. Stay informed about the role of mast cells, basophils, anaphylaxis, and potential links to immunodeficiency disorders.
Managing hyperimmunoglobulinemia E involves a multidisciplinary approach that may include allergists, immunologists, and dermatologists. Treatment options aim to reduce IgE levels, control symptoms, and prevent complications. By learning more about this condition, individuals can better navigate their healthcare journey and improve their quality of life.
Understanding Immunoglobulins
Immunoglobulins, also known as antibodies, play a crucial role in the immune system’s defense against harmful substances. There are five main classes of immunoglobulins, with IgE being one of them. IgE is primarily involved in allergic reactions and hypersensitivity responses.
Individuals with hyperimmunoglobulinemia E have elevated levels of IgE, which can lead to an exaggerated immune response to harmless substances, such as pollen or certain foods. Understanding how IgE interacts with antigens and triggers the release of histamine from mast cells and basophils is key in comprehending the pathophysiology of allergic conditions.
By gaining insight into the functions of immunoglobulins, particularly IgE, individuals can better grasp the underlying mechanisms of hyperimmunoglobulinemia E and its associated symptoms. This knowledge empowers both patients and healthcare providers to make informed decisions regarding diagnosis, treatment, and long-term management strategies.
Relationship with Atopic Dermatitis
Atopic dermatitis, also known as eczema, is a common skin condition characterized by red, itchy, and inflamed skin patches. In individuals with hyperimmunoglobulinemia E, there is a strong relationship with atopic dermatitis due to the elevated levels of IgE, which contribute to the inflammatory response in the skin.
Understanding the link between hyperimmunoglobulinemia E and atopic dermatitis is essential for healthcare providers to effectively diagnose and manage both conditions. Treatment approaches may involve addressing the underlying IgE-mediated hypersensitivity reactions, controlling skin inflammation, and relieving itching to improve the quality of life for individuals affected by these conditions.
By recognizing the connection between hyperimmunoglobulinemia E and atopic dermatitis, patients can work collaboratively with their healthcare team to develop personalized treatment plans that target the root cause of their symptoms. Education on proper skincare routines, allergen avoidance, and medication management can help individuals better manage their atopic dermatitis and associated allergic manifestations.
Connection to Allergies and Asthma
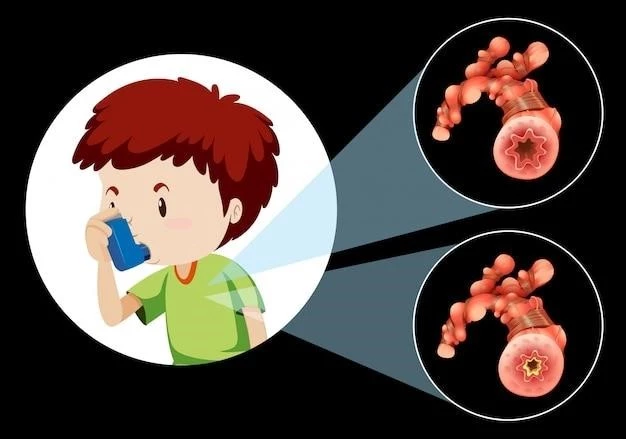
Hyperimmunoglobulinemia E is closely linked to allergies and asthma, as elevated IgE levels play a significant role in the development and exacerbation of these conditions. Allergies, such as hay fever or food allergies, can trigger an immune response mediated by IgE, leading to symptoms like sneezing, wheezing, or hives.
Asthma, a chronic respiratory condition characterized by airway inflammation and narrowing, can also be influenced by hyperimmunoglobulinemia E. The inflammatory response triggered by IgE can contribute to asthma symptoms, including coughing, shortness of breath, and chest tightness.
Recognizing the connection between hyperimmunoglobulinemia E, allergies, and asthma is crucial for healthcare providers to develop comprehensive treatment plans that address the underlying immune dysregulation. Managing IgE levels, identifying and avoiding triggers, and using medications to control symptoms are vital components of managing these interconnected conditions effectively.
Symptoms like Eczema and Pruritus
Eczema, also known as atopic dermatitis, is a common symptom associated with hyperimmunoglobulinemia E. It presents as red, itchy, and inflamed patches on the skin, often exacerbated by elevated levels of IgE. Proper management of eczema involves moisturizing the skin, avoiding irritants, and using prescribed medications to reduce inflammation.
Pruritus, or itching, is another prevalent symptom linked to hyperimmunoglobulinemia E. The persistent urge to scratch the skin can cause discomfort and skin damage. Understanding the triggers of pruritus, such as allergens or dry skin, is essential in developing strategies to alleviate itching and improve the skin’s condition.
Individuals experiencing eczema and pruritus should consult healthcare professionals for a comprehensive evaluation and personalized treatment plan. Addressing the underlying immune dysregulation associated with hyperimmunoglobulinemia E can help manage these distressing symptoms effectively and enhance the overall quality of life for those affected.
Role of Mast Cells and Basophils
Mast cells and basophils are key players in the immune response associated with hyperimmunoglobulinemia E. When allergens trigger the immune system in individuals with elevated IgE levels, mast cells and basophils release histamine, leading to allergic reactions.
Understanding the role of mast cells and basophils is essential in managing allergic symptoms like asthma, eczema, and pruritus in the context of hyperimmunoglobulinemia E. Medications that target histamine receptors, such as antihistamines, can help alleviate symptoms by blocking the effects of histamine released by these cells.
Healthcare providers may recommend strategies to reduce the activation of mast cells and basophils, including allergen avoidance, proper medication use, and lifestyle modifications. By addressing the underlying mechanisms involving these immune cells, individuals can better control their allergic manifestations and improve their overall well-being.
Severe Complications⁚ Anaphylaxis
Anaphylaxis is a severe, potentially life-threatening allergic reaction that can occur in individuals with hyperimmunoglobulinemia E. This heightened allergic response can lead to systemic symptoms, including difficulty breathing, swelling, low blood pressure, and even shock.
Recognizing the signs of anaphylaxis and seeking immediate medical attention is crucial in individuals with hyperimmunoglobulinemia E. Healthcare providers may recommend carrying an epinephrine auto-injector for prompt treatment in case of an emergency. Education on triggers, early symptoms, and emergency protocols is essential for preventing and managing anaphylactic reactions effectively.

By understanding the risk of anaphylaxis in the context of hyperimmunoglobulinemia E, individuals can take proactive measures to minimize exposure to allergens, adhere to treatment plans, and communicate their condition to healthcare providers, family members, and peers. Prompt action in the event of anaphylaxis can help save lives and ensure better outcomes for those at risk.
Immunodeficiency and Treatment Options
Hyperimmunoglobulinemia E can be associated with immunodeficiency, where the immune system may not function optimally despite elevated IgE levels. This can predispose individuals to recurrent infections and other complications.
Treatment options for hyperimmunoglobulinemia E focus on managing symptoms, reducing IgE levels, and addressing any underlying immunodeficiency. This may include medications to control inflammation, boost immune function, and prevent allergic reactions.
It is essential for individuals with hyperimmunoglobulinemia E and potential immunodeficiency to work closely with healthcare professionals to develop a tailored treatment plan. Regular monitoring, adherence to prescribed medications, and lifestyle modifications can help optimize immune function and improve overall health outcomes.