Understanding Erosive Pustular Dermatosis of the Scalp
Erosive Pustular Dermatosis of the Scalp is a rare skin disorder characterized by inflammatory lesions, crusting, itching, flaking, and ulceration. Diagnosis involves dermatological assessment. Treatment often includes topical medication for chronic management.
I. Introduction
Erosive Pustular Dermatosis of the Scalp, also known as Erosive Pustulosis of the Scalp, is a challenging dermatological condition that primarily affects the scalp. This rare disorder is characterized by the formation of pustules, erosions, crusted lesions, and ulcers on the scalp, leading to hair loss. Individuals with Erosive Pustular Dermatosis of the Scalp often experience intense itching, flaking, and discomfort.
While the exact cause of this condition remains uncertain, it is believed to be associated with chronic inflammatory processes. Erosive Pustular Dermatosis of the Scalp typically affects older individuals, especially women, and those with a history of scalp trauma or previous skin damage.
Understanding the symptoms, causes, and risk factors associated with Erosive Pustular Dermatosis of the Scalp is essential for timely diagnosis and effective management of this dermatological condition. Through proper diagnosis and targeted treatment, individuals with this condition can experience symptom relief and improved scalp health.
II. Symptoms and Characteristics
Erosive Pustular Dermatosis of the Scalp presents with a range of distressing symptoms and distinct characteristics that impact the scalp’s health and appearance. The key symptoms and characteristics include⁚
- Pustules⁚ The formation of pustules on the scalp, which are small, pus-filled bumps that may rupture and crust over.
- Erosions⁚ Shallow ulcerations or erosions on the scalp surface, often surrounded by areas of inflammation.
- Crusted Lesions⁚ Thick crusts that form over the affected areas, resulting from the healing process of the erosions.
- Ulcers⁚ Open sores or ulcers that may be painful and non-healing, leading to scarring in severe cases.
- Itching⁚ Intense itching of the scalp, which can be a distressing symptom for individuals with Erosive Pustular Dermatosis.
- Hair Loss⁚ Progressive hair loss in the areas affected by the condition due to inflammation and damage to the hair follicles.
- Flaking⁚ Excessive flaking or scaling of the scalp skin, often accompanied by redness and irritation.
These symptoms and characteristics of Erosive Pustular Dermatosis of the Scalp can significantly impact an individual’s quality of life, causing discomfort, self-esteem issues, and emotional distress. Recognizing these signs is crucial for early intervention and appropriate management of the condition.
III. Causes and Risk Factors
The precise causes of Erosive Pustular Dermatosis of the Scalp remain unclear; however, several factors may contribute to the development of this dermatological condition. Some potential causes and risk factors include⁚
- Chronic Inflammatory Processes⁚ Erosive Pustular Dermatosis of the Scalp is believed to be associated with chronic inflammation of the scalp skin, leading to the formation of pustules, erosions, and ulcers.
- Previous Scalp Trauma⁚ Individuals with a history of scalp trauma, such as burns, surgeries, or radiation therapy, may be at a higher risk of developing this condition.
- Autoimmune Factors⁚ Autoimmune processes within the body could play a role in triggering the inflammatory response seen in Erosive Pustular Dermatosis of the Scalp.
- Advanced Age⁚ This condition predominantly affects older individuals, especially those over the age of 60, although it can occur in younger age groups as well.
- Female Gender⁚ Women are more commonly affected by Erosive Pustular Dermatosis of the Scalp than men, though the reasons for this gender discrepancy are not well understood.
- Existing Skin Conditions⁚ Individuals with pre-existing skin conditions, such as psoriasis or eczema, may have an increased susceptibility to developing Erosive Pustular Dermatosis of the Scalp.
Understanding the potential causes and risk factors associated with this condition is vital for healthcare providers to assess and manage individuals presenting with symptoms of Erosive Pustular Dermatosis of the Scalp effectively. Further research is needed to elucidate the underlying mechanisms driving the development of this rare scalp disorder.
IV. Diagnosis
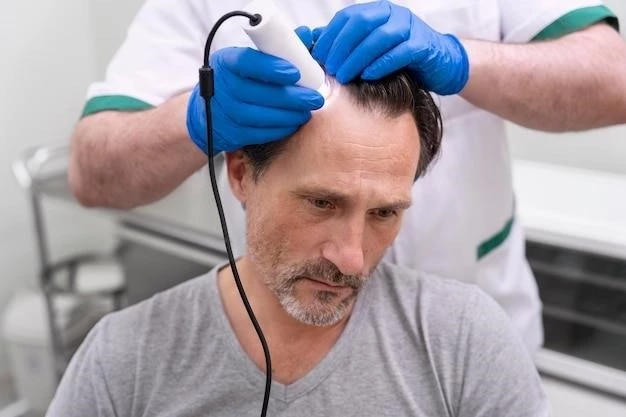
Diagnosing Erosive Pustular Dermatosis of the Scalp involves a comprehensive dermatological evaluation to determine the presence of characteristic symptoms and confirm the condition. The diagnostic process may include the following steps⁚
- Medical History⁚ Healthcare providers will review the patient’s medical history, including any previous skin conditions, scalp traumas, or autoimmune disorders.
- Physical Examination⁚ A thorough examination of the scalp will be conducted to assess the presence of pustules, erosions, crusting, ulcers, and other associated symptoms.
- Biopsy⁚ A skin biopsy may be performed to obtain a tissue sample from the affected area for microscopic analysis, helping to confirm the diagnosis.
- Culture and Tests⁚ In some cases, cultures or other laboratory tests may be recommended to rule out infectious causes or underlying conditions.
- Dermatological Imaging⁚ Imaging studies like dermoscopy or reflectance confocal microscopy may aid in visualizing the skin layers and assessing the extent of tissue damage.
Since Erosive Pustular Dermatosis of the Scalp is a rare condition with overlapping features of other dermatological disorders, an accurate diagnosis is crucial for initiating appropriate treatment. Healthcare providers with expertise in dermatology play a pivotal role in correctly identifying and differentiating this scalp disorder from other similar conditions.
V. Treatment Options
Managing Erosive Pustular Dermatosis of the Scalp involves a multi-faceted approach aimed at alleviating symptoms, promoting healing, and preventing disease progression. Several treatment options can be considered for individuals diagnosed with this challenging scalp disorder⁚
- Topical Medication⁚ Topical corticosteroids or calcineurin inhibitors may be prescribed to reduce inflammation, itching, and promote healing of the affected scalp areas.
- Antibiotics⁚ In cases where secondary infection is present, oral or topical antibiotics may be recommended to combat bacterial overgrowth and prevent further complications.
- Emollients⁚ Moisturizing agents or emollients can help hydrate the scalp skin, reduce flaking, and improve the overall condition of the scalp.
- Cryotherapy⁚ Cryosurgery or cryotherapy techniques may be utilized to freeze and remove damaged tissue, promoting skin regeneration.
- Systemic Therapy⁚ In severe or refractory cases, systemic immunosuppressive drugs or biologic agents may be considered to target the underlying inflammatory processes.
- Dermatological Procedures⁚ Surgical interventions such as skin grafting or laser therapy could be options for individuals with extensive ulceration or scarring.
Individualized treatment plans tailored to the specific needs and severity of Erosive Pustular Dermatosis of the Scalp are essential in achieving optimal outcomes and improving quality of life for affected individuals. Close monitoring by dermatological specialists is recommended to track progress, adjust treatment strategies, and address any treatment-related side effects.
VI. Management and Care
Effective management and care strategies play a crucial role in supporting individuals living with Erosive Pustular Dermatosis of the Scalp to enhance their quality of life and promote scalp health. Here are key considerations for managing this challenging dermatological condition⁚
- Regular Dermatological Monitoring⁚ Routine follow-up visits with a dermatologist are essential to assess disease progression, monitor treatment efficacy, and address any emerging concerns.
- Scalp Hygiene⁚ Gentle scalp care practices, such as using mild shampoos, avoiding harsh chemical treatments, and keeping the scalp clean, can help minimize irritation and support healing.
- Sun Protection⁚ Sun exposure can exacerbate scalp symptoms; therefore, wearing hats or using sunscreen on the scalp when outdoors is recommended to protect the skin.
- Emotional Support⁚ Living with a chronic skin condition like Erosive Pustular Dermatosis of the Scalp can impact emotional well-being. Seeking support from mental health professionals or support groups can be beneficial.
- Diet and Lifestyle⁚ Maintaining a healthy diet rich in nutrients and staying hydrated can contribute to overall skin health. Avoiding triggers like stress or certain foods that worsen symptoms is also important.
- Patient Education⁚ Educating individuals about their condition, treatment options, and self-care practices empowers them to actively participate in managing their scalp health.
By implementing comprehensive management strategies and adopting a holistic approach to care, individuals with Erosive Pustular Dermatosis of the Scalp can better cope with the challenges posed by this condition and improve their scalp’s well-being over time. Collaboration between healthcare providers, patients, and caregivers is vital in achieving successful management outcomes.
VII. Research and Advancements
Ongoing research and advancements in the field of dermatology are crucial for expanding our understanding of Erosive Pustular Dermatosis of the Scalp and developing innovative treatment approaches. Several areas of focus for research and potential advancements include⁚
- Pathogenesis Studies⁚ Investigating the underlying mechanisms that trigger the inflammatory response leading to Erosive Pustular Dermatosis of the Scalp to identify novel therapeutic targets.
- Biomarker Discovery⁚ Identifying specific biomarkers associated with the condition could aid in early diagnosis, prognosis prediction, and personalized treatment strategies.
- Genetic Research⁚ Exploring genetic factors that may predispose individuals to developing this scalp disorder can provide insights into genetic susceptibility and inheritance patterns.
- Immunomodulatory Therapies⁚ Developing immunomodulatory agents or biologic therapies targeted at regulating the immune response involved in Erosive Pustular Dermatosis of the Scalp.
- Telemedicine and Digital Health⁚ Utilizing telemedicine platforms for remote consultations, monitoring, and patient education can improve accessibility to specialized care for individuals with this rare condition.
- Clinical Trials⁚ Participating in clinical trials investigating new drug formulations, surgical techniques, or treatment modalities can offer promising options for individuals who are refractory to conventional therapies.
By investing in research initiatives and embracing technological advancements, healthcare professionals and researchers can advance the field of dermatology, enhance patient outcomes, and ultimately improve the care and management of individuals affected by Erosive Pustular Dermatosis of the Scalp. Collaboration across interdisciplinary teams is vital in driving progress and innovation in addressing this challenging scalp disorder.
VIII. Patient Education and Support
Empowering individuals with Erosive Pustular Dermatosis of the Scalp through education and fostering a supportive environment is essential in promoting self-management and overall well-being. Effective patient education and support initiatives may include⁚
- Disease Understanding⁚ Providing clear and comprehensive information about the nature of the condition, its symptoms, potential triggers, and treatment options to enhance patient knowledge and awareness.
- Self-Care Practices⁚ Educating individuals on scalp hygiene, skincare routines, sun protection, and lifestyle modifications that can help alleviate symptoms and maintain scalp health.
- Treatment Compliance⁚ Encouraging adherence to prescribed medications, follow-up appointments, and recommended lifestyle changes to optimize treatment outcomes and disease management.
- Mental Health Support⁚ Offering access to mental health resources, counseling services, or support groups to address the emotional impact of living with a chronic skin condition and promote psychological well-being.
- Community Engagement⁚ Facilitating connections with other individuals facing similar challenges, creating a sense of community, and fostering peer support networks for mutual encouragement and understanding.
- Resource Accessibility⁚ Providing resources, educational materials, and online platforms where patients can access reliable information, participate in discussions, and seek guidance from healthcare professionals.
By prioritizing patient education and support initiatives, healthcare providers can empower individuals with Erosive Pustular Dermatosis of the Scalp to actively participate in their care, make informed decisions, and navigate the complexities of managing this rare scalp disorder with confidence and resilience.
IX. Conclusion
In conclusion, Erosive Pustular Dermatosis of the Scalp is a rare and challenging dermatological condition characterized by inflammatory lesions, crusting, ulceration, and hair loss on the scalp. Timely diagnosis through dermatological assessment and appropriate treatment with topical medications are essential for managing this chronic disorder.
Understanding the symptoms, causes, and risk factors associated with Erosive Pustular Dermatosis of the Scalp is critical in providing targeted care and support to individuals affected by this condition. By integrating patient education, supportive resources, and advancements in research, healthcare professionals can enhance the quality of life for patients living with this scalp disorder.
Continued research efforts, technological innovations, and interdisciplinary collaboration are key to advancing the field of dermatology and improving outcomes for individuals with Erosive Pustular Dermatosis of the Scalp. By fostering a holistic approach to care, incorporating patient-centered strategies, and promoting a supportive environment, healthcare providers can empower patients to navigate the challenges of this rare skin condition with resilience and confidence.
Through ongoing education, advocacy, and patient-centered care, individuals with Erosive Pustular Dermatosis of the Scalp can effectively manage their symptoms, maintain scalp health, and lead fulfilling lives despite the complexities of this dermatological disorder.
