Understanding Filariasis ⏤ A Debilitating Parasitic Disease
Filariasis is a parasitic disease affecting the lymphatic system, commonly transmitted through mosquitoes in tropical regions․ It leads to conditions like elephantiasis and lymphedema due to the accumulation of lymph fluid․ Antiparasitic drugs are used to treat microfilariae, reducing fever, swelling, and damage to lymph nodes caused by this vector-borne disease․
Introduction to Filariasis
Filariasis is a parasitic disease caused by thread-like nematode worms belonging to the Filarioidea family․ These worms infect the lymphatic system, leading to various serious health issues․ The most common types of filariasis are lymphatic filariasis, which causes elephantiasis, and subcutaneous filariasis․
This disease is prevalent in tropical regions worldwide, particularly in areas with poor sanitation and standing water, creating breeding grounds for the mosquitoes that act as vectors for transmitting the infection․ Filariasis can have a significant impact on individuals’ quality of life and can lead to long-term disabilities if left untreated․
Understanding the transmission, symptoms, diagnosis, treatment, and prevention of filariasis is crucial in combating its spread and reducing its burden on affected populations․ Through awareness, effective control measures, and access to antiparasitic drugs, the global health community can work towards eliminating this debilitating parasitic disease․
Types of Filariasis
There are several types of filariasis caused by different species of parasitic worms․ The most common forms include lymphatic filariasis, which leads to a condition known as elephantiasis, characterized by severe swelling and thickening of the skin․ Another type is subcutaneous filariasis, where the worms reside in the subcutaneous tissues․
Onchocerciasis, or river blindness, is another form of filariasis caused by Onchocerca volvulus․ This disease primarily affects the skin and eyes, leading to visual impairment and severe skin issues․ Loiasis, caused by Loa loa worms, presents with symptoms like fever and swelling in the subcutaneous tissues․
Mansonella perstans and Mansonella ozzardi are other types of filariasis affecting humans, with symptoms such as skin nodules and eye lesions․ Each type of filariasis has distinct characteristics and effects on the human body, often leading to chronic health issues if untreated․ Understanding the different types of filariasis is essential for accurate diagnosis and effective treatment strategies․
Transmission and Vector
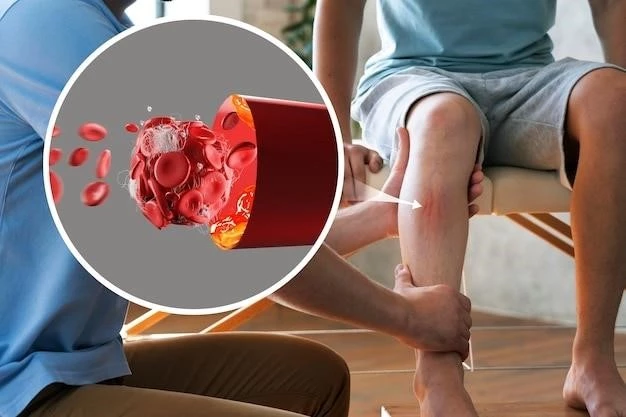
Filariasis is primarily transmitted through the bite of infected mosquitoes․ Mosquito species such as Aedes, Anopheles, and Culex serve as vectors for carrying the parasitic worms responsible for the disease․ When an infected mosquito bites a human host, it introduces the microscopic larvae, known as microfilariae, into the bloodstream․
Once inside the human body, the microfilariae migrate to the lymphatic system, where they mature into adult worms․ These adult worms then reproduce, releasing more microfilariae into the bloodstream, perpetuating the cycle of infection․ Mosquitoes become infected with the parasite when they feed on blood from an infected individual, completing the transmission cycle․
The presence of standing water, poor sanitation, and inadequate waste management contribute to increased mosquito populations, enhancing the risk of filariasis transmission․ Prevention measures such as mosquito control, bed nets, and insect repellents play a crucial role in reducing the transmission of this parasitic disease in endemic regions․
Symptoms and Effects
The symptoms of filariasis can vary depending on the type of infection and the stage of the disease․ In lymphatic filariasis, individuals may experience fever, lymphedema (swelling of limbs), and enlarged lymph nodes․ Elephantiasis, a severe form of lymphedema, can cause disfigurement and disability, particularly in the legs and genitals․
In subcutaneous filariasis, symptoms may include skin rashes, itching, and the presence of nodules under the skin․ Onchocerciasis or river blindness can lead to visual impairment, skin depigmentation, and intense itching․ Loiasis may present with migratory swellings, joint pain, and itching․
Chronic filarial infections can also cause damage to the lymphatic system, leading to lymphatic dysfunction and recurrent infections․ In severe cases, filariasis can impact an individual’s mobility, productivity, and overall quality of life․ Early diagnosis and treatment are essential in preventing long-term complications and reducing the burden of this debilitating parasitic disease․
Diagnosis and Treatment
Diagnosing filariasis typically involves a combination of clinical assessment, imaging tests, and laboratory techniques․ Physical examination may reveal characteristic symptoms such as lymphedema, skin changes, or enlarged lymph nodes․ Blood tests can help detect the presence of microfilariae or specific antibodies against the parasitic worms․
Imaging studies like ultrasound and MRI may be used to visualize lymphatic damage or identify adult worms in affected tissues․ Once diagnosed, treatment aims to eliminate the parasitic infection and manage associated symptoms․ Antiparasitic drugs such as albendazole, ivermectin, and diethylcarbamazine (DEC) are commonly prescribed to kill the adult worms and microfilariae․
In cases of severe swelling or lymphedema, supportive treatments like compression therapy, physical rehabilitation, and wound care may be necessary to improve patient outcomes․ Surgical interventions may be considered for individuals with advanced stages of elephantiasis to alleviate symptoms and improve mobility․ Regular monitoring and follow-up are essential to assess treatment efficacy and prevent disease recurrence․
Prevention and Control
Preventing filariasis relies on comprehensive strategies to control mosquito populations and reduce human-mosquito contact․ Public health efforts focus on vector control measures such as insecticide-treated bed nets, indoor residual spraying, and environmental management to eliminate mosquito breeding sites․
Community education and awareness campaigns play a vital role in promoting personal protective measures like wearing long sleeves, using insect repellents, and sleeping under mosquito nets․ Mass drug administration programs, distributing antiparasitic drugs to at-risk populations, are also key in reducing the prevalence of filariasis in endemic areas․
Improving sanitation infrastructure, access to clean water, and proper waste disposal can help minimize mosquito breeding grounds and interrupt the transmission cycle of the parasite․ Integrated approaches that involve collaboration between healthcare providers, government agencies, and community leaders are essential in sustaining long-term control efforts and preventing disease resurgence․
Impact on Global Health
Filariasis poses a significant burden on global health, especially in tropical and subtropical regions where the disease is endemic․ The socio-economic impact of filariasis is profound, affecting individuals, families, and communities by causing disabilities, decreased productivity, and increased healthcare costs․
Chronic filarial infections can lead to long-term disability, stigmatization, and reduced quality of life for those affected․ The physical disfigurement and functional limitations associated with conditions like elephantiasis can impact mobility, mental well-being, and social interactions․
Furthermore, filariasis contributes to the cycle of poverty, as affected individuals may face challenges in accessing education, employment opportunities, and healthcare services․ The economic burden of treating and managing filariasis adds pressure to already strained healthcare systems in endemic regions․
Efforts to control and eliminate filariasis not only improve the health outcomes of individuals but also have broader societal benefits, including increased productivity, reduced healthcare expenditures, and enhanced quality of life for affected populations․ Global initiatives focusing on filariasis eradication aim to alleviate the disease’s impact on communities and advance the overall well-being of individuals worldwide․
