Malignant Mixed Müllerian Tumor
Overview of Malignant Mixed Müllerian Tumor
Malignant Mixed Müllerian Tumor (MMMT), also known as carcinosarcoma, is a rare and aggressive form of uterine cancer. It is characterized by the presence of both carcinoma and sarcoma components within the tumor. MMMT arises from the endometrial lining of the uterus and exhibits a high propensity for metastasis.
Histopathology plays a crucial role in diagnosing MMMT, with the identification of malignant epithelial and mesenchymal components being key. Genetic mutations and immunohistochemistry markers also aid in confirming the diagnosis.
Clinically, patients with MMMT may present with symptoms such as pelvic pain and abnormal vaginal bleeding. Early detection is challenging due to the nonspecific nature of these symptoms.
Treatment of MMMT typically involves a multidisciplinary approach, including surgery, chemotherapy, and radiotherapy. In some cases, neoadjuvant therapy may be considered to reduce tumor size prior to surgery.
Despite advancements in treatment, the prognosis for MMMT remains guarded, with a high risk of recurrence and metastasis. Close monitoring of tumor markers and regular follow-up with an oncologist are essential for managing MMMT effectively.
Etiology and Pathogenesis
The exact etiology of Malignant Mixed Müllerian Tumor (MMMT) remains unclear; however, it is believed to originate from the malignant transformation of Müllerian duct remnants in the uterus. Genetic mutations, including alterations in TP53 and PTEN genes, have been associated with the development of MMMT.
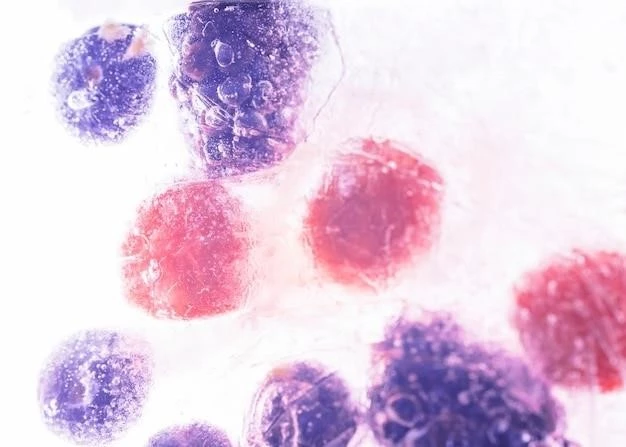
Pathologically, MMMT is characterized by the presence of both epithelial (carcinomatous) and mesenchymal (sarcomatous) components, which suggest a biphasic differentiation. The tumor likely arises through metaplastic changes in the endometrial epithelium, leading to the development of both carcinomatous and sarcomatous elements.
Immunohistochemistry studies have shown that MMMT shares some characteristics with both endometrial carcinomas and sarcomas, supporting the theory of a common origin from Müllerian duct structures. The complex interplay between genetic mutations and histological features contributes to the aggressive behavior of MMMT.
Further research is needed to elucidate the specific molecular pathways involved in the pathogenesis of MMMT. Understanding the etiology and pathogenesis of this rare uterine cancer is essential for developing targeted treatment strategies that can improve outcomes and overall survival for patients diagnosed with MMMT.
Clinical Presentation and Diagnosis
Patient with Malignant Mixed Müllerian Tumor (MMMT) may present with symptoms such as pelvic pain, abnormal vaginal bleeding, and postmenopausal bleeding. However, these clinical manifestations are nonspecific and can be attributed to various gynecological conditions, making early diagnosis challenging.
Diagnostic evaluation of MMMT involves a combination of imaging studies, such as transvaginal ultrasound and magnetic resonance imaging (MRI), to assess the extent of the tumor and detect any metastasis. Definitive diagnosis is achieved through histopathological examination of tissue samples obtained via biopsy or surgical resection.
Histopathology plays a crucial role in identifying the dual carcinomatous and sarcomatous components of MMMT. Immunohistochemistry studies, including markers for epithelial and mesenchymal differentiation, aid in confirming the diagnosis.
In addition to imaging and histopathology, evaluation of tumor markers, such as CA-125 and carcinoembryonic antigen (CEA), may be useful in monitoring disease progression and response to treatment. A multidisciplinary approach involving gynecological oncologists, radiologists, pathologists, and other specialists is essential for accurate diagnosis and treatment planning in patients with MMMT;
Treatment Strategies
The management of Malignant Mixed Müllerian Tumor (MMMT) often requires a multidisciplinary approach to address its aggressive nature. The primary treatment modalities for MMMT include surgery, chemotherapy, and radiotherapy, with the goal of achieving optimal disease control and improving outcomes.
Surgical intervention plays a crucial role in the treatment of MMMT, aiming to remove the tumor and potentially involved surrounding structures. Depending on the extent of disease and patient factors, procedures such as hysterectomy with bilateral salpingo-oophorectomy and lymph node dissection may be performed.
Chemotherapy is an essential component of adjuvant treatment for MMMT, particularly in cases where there is a high risk of recurrence or metastasis. Regimens combining platinum-based agents with other cytotoxic drugs have shown effectiveness in reducing tumor burden and improving survival rates.
Radiotherapy may be employed as adjuvant therapy following surgery to target residual disease or as palliative treatment to alleviate symptoms in cases of advanced or metastatic MMMT. The use of advanced techniques, such as intensity-modulated radiotherapy, can help minimize toxicity to surrounding healthy tissues.
For select cases, neoadjuvant therapy may be considered to shrink the tumor size before surgery, potentially enabling more conservative surgical approaches. The integration of targeted therapies and immunotherapies into treatment regimens is an area of active research to enhance the efficacy of treatment for MMMT.
Prognosis and Metastasis
The prognosis for patients with Malignant Mixed Müllerian Tumor (MMMT) is generally guarded due to its aggressive nature and high propensity for metastasis. The most common sites of metastasis for MMMT include the lungs, liver, and peritoneum, with distant spread indicating advanced disease and poorer outcomes.
Despite advancements in treatment modalities such as surgery, chemotherapy, and radiotherapy, MMMT carries a significant risk of recurrence even after achieving initial remission. The likelihood of recurrence is influenced by factors such as tumor stage, grade, and the extent of surgical debulking.
Prognostic indicators such as age, performance status, and response to treatment also play a role in determining the overall outlook for patients with MMMT. Close monitoring of tumor markers, imaging studies, and clinical symptoms is crucial for assessing disease progression and tailoring treatment strategies accordingly.
A multidisciplinary approach involving gynecological oncologists, medical oncologists, radiation oncologists, and supportive care teams is essential in providing comprehensive care for patients with MMMT. Research efforts are ongoing to identify novel therapeutic targets and personalized treatment approaches that may improve outcomes and quality of life for individuals affected by this rare and aggressive uterine cancer.
Multidisciplinary Approach in Care
The management of patients with Malignant Mixed Müllerian Tumor (MMMT) necessitates a comprehensive multidisciplinary approach to address the complex nature of this aggressive uterine cancer. A team of gynecological oncologists, medical oncologists, radiation oncologists, pathologists, radiologists, and supportive care providers collaborates to ensure a holistic and personalized care plan for each patient.
Gynecological oncologists play a central role in coordinating the treatment of MMMT, overseeing surgical interventions, chemotherapy regimens, and long-term follow-up care. Medical oncologists contribute expertise in administering systemic therapies tailored to the individual patient’s disease characteristics and overall health status.
Radiation oncologists are vital in the delivery of radiotherapy, either as adjuvant therapy post-surgery or as palliative treatment to manage symptoms and improve quality of life in advanced cases of MMMT. Pathologists provide critical diagnostic insights through histopathological examination and immunohistochemistry studies, aiding in confirming the presence of MMMT and guiding treatment decisions.
Supportive care teams, including nurses, social workers, and psychologists, play an essential role in addressing the emotional, psychological, and practical needs of patients with MMMT. Palliative care specialists also contribute to managing symptoms, enhancing comfort, and providing end-of-life support when necessary.
By harnessing the expertise of a multidisciplinary team and individualizing care plans to each patient’s unique circumstances, healthcare providers can optimize outcomes, enhance quality of life, and ensure comprehensive support for individuals affected by this challenging disease.
Research and Advancements
Ongoing research efforts in the field of Malignant Mixed Müllerian Tumor (MMMT) are focused on elucidating the underlying molecular mechanisms, identifying novel therapeutic targets, and improving treatment outcomes for patients with this rare and aggressive uterine cancer. Advances in genomics, molecular profiling, and immunotherapy are shaping the landscape of MMMT research.
Studies exploring the genetic mutations associated with MMMT, such as alterations in TP53 and PTEN genes٫ aim to unravel the pathogenesis of the disease and identify potential targets for precision therapies. Molecular profiling techniques٫ including next-generation sequencing and gene expression analysis٫ offer insights into the heterogeneity of MMMT tumors and guide personalized treatment strategies.
Immunotherapy, particularly immune checkpoint inhibitors, is being investigated as a promising approach to enhancing the immune response against MMMT cells and improving treatment responses. Clinical trials evaluating the efficacy of immunotherapeutic agents alone or in combination with standard treatments are underway to assess their impact on patient outcomes.
Novel treatment modalities, such as targeted therapies directed at specific molecular pathways involved in MMMT tumorigenesis, hold promise for improving response rates and prolonging survival in patients with advanced disease. Advances in imaging technologies, radiation techniques, and supportive care measures also contribute to the evolution of MMMT management.
By fostering collaboration among researchers, clinicians, and patient advocates, the field of MMMT research continues to drive innovation, uncover new therapeutic avenues, and ultimately improve the prognosis and quality of life for individuals affected by this challenging uterine cancer.
Conclusion
In conclusion, Malignant Mixed Müllerian Tumor (MMMT) represents a rare and aggressive form of uterine cancer characterized by its biphasic nature and high metastatic potential; The complex interplay between carcinoma and sarcoma components within MMMT poses significant challenges in diagnosis and treatment.
A multidisciplinary approach involving gynecological oncologists, pathologists, radiologists, and supportive care teams is paramount in delivering comprehensive and personalized care for patients with MMMT. Advances in surgical techniques, chemotherapy regimens, and radiation protocols have improved treatment outcomes, yet the prognosis remains guarded due to the risk of recurrence and metastasis.
Ongoing research endeavors in genomics, molecular profiling, and immunotherapy offer promising avenues for enhancing the understanding of MMMT pathogenesis and developing targeted therapeutic strategies. Collaborative efforts across institutions and disciplines are essential in driving innovation, advancing treatment modalities, and ultimately improving patient survival and quality of life.
By fostering a holistic approach to care, integrating the latest research findings into clinical practice, and prioritizing patient-centered support, healthcare providers can strive to optimize outcomes and provide compassionate care for individuals impacted by this challenging disease. Continued vigilance in monitoring disease progression, exploring novel therapies, and enhancing supportive services are critical in the ongoing battle against MMMT.
