Hemorrhagic Fever with Renal Syndrome
Hemorrhagic Fever with Renal Syndrome (HFRS) is a serious viral infection transmitted through rodents’ droppings, urine, or saliva. The disease is caused by viruses like Hantaan, Seoul, Dobrava, and Puumala. The symptoms include headache, back pain, abdominal pain, and low blood pressure. Treatment involves supportive care and antiviral medications. Complications may require dialysis. Prevention strategies focus on rodent control and potential vaccines.
Introduction
Hemorrhagic Fever with Renal Syndrome (HFRS) is a severe acute febrile illness caused by different types of Hantaviruses. These viruses are mainly carried by rodents, such as mice and rats, and can be transmitted to humans through contact with rodent excreta (droppings, urine, and saliva). The four main types of Hantaviruses that cause HFRS in different regions are Hantaan virus (mainly in Asia), Seoul virus (Asia), Dobrava virus (Balkans), and Puumala virus (Europe). These viruses can lead to a range of symptoms, including fever, headache, back pain, abdominal pain, and renal dysfunction; In severe cases, it can progress to hemorrhagic manifestations, shock, and acute kidney injury.
While the mortality rate varies depending on the virus strain and the region, HFRS can be a life-threatening condition if not diagnosed and managed promptly. The first recognized outbreak of HFRS occurred during the Korean War in the 1950s, associated with the Hantaan virus, highlighting the potential for these viruses to cause significant outbreaks.
Due to the diverse range of Hantaviruses and their rodent reservoirs, the geographic distribution of HFRS varies worldwide. In endemic regions, individuals living in rural areas or engaging in outdoor activities are at a higher risk of exposure to the virus through contact with infected rodents or their excreta. Understanding the transmission and symptoms of HFRS is crucial for early detection and appropriate management of this potentially fatal disease.
Overview of HFRS
Hemorrhagic Fever with Renal Syndrome (HFRS) is a group of clinically similar illnesses caused by several types of Hantaviruses. These viruses belong to the Bunyaviridae family and are predominantly associated with rodents, serving as their natural hosts. Humans typically become infected through inhalation of aerosolized virus particles from rodent excreta or direct contact with contaminated materials.
The clinical presentation of HFRS can vary depending on the specific Hantavirus involved, but common symptoms include fever, headache, back pain, abdominal pain, and renal impairment. The disease progresses in phases, with an initial febrile phase followed by hypotension, hemorrhagic manifestations, and renal failure. Severe cases can lead to shock and multi-organ dysfunction.
Diagnosis of HFRS is based on a combination of clinical presentation, history of rodent exposure, laboratory tests such as serology and polymerase chain reaction (PCR), and imaging studies. Early detection is crucial for initiating appropriate treatment and preventing complications. Treatment primarily consists of supportive care to manage symptoms and complications, including fluid resuscitation, pain relief, and hemodynamic support.
Antiviral medications may be considered in certain cases to reduce viral replication and improve outcomes. However, the effectiveness of antivirals in HFRS remains under investigation. In severe cases of HFRS with renal failure, dialysis may be necessary to support kidney function until recovery occurs.
Complications of HFRS can be severe and may include acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), and neurological dysfunction. Patients with these complications require intensive care management to improve survival rates and reduce long-term sequelae.
Prevention of HFRS primarily focuses on rodent control measures to reduce the risk of human exposure to infected animals and their excreta. This includes proper sanitation practices, avoiding contact with rodents, and sealing potential entry points in buildings to prevent rodent entry. In some endemic regions, vaccination strategies may be employed to protect at-risk populations from Hantavirus infection.
Transmission of HFRS
Hemorrhagic Fever with Renal Syndrome (HFRS) is primarily transmitted through contact with rodents carrying Hantaviruses, the causative agents of the disease. The main modes of transmission involve exposure to rodent excreta, including droppings, urine, and saliva, which can contain infectious viral particles. Humans can become infected by inhaling aerosolized particles when cleaning or disturbing areas contaminated with rodent excreta.
Additionally, direct contact with infected rodents or their fluids can also lead to transmission of Hantaviruses. The viruses can enter the human body through mucous membranes, broken skin, or by inhalation. It is important to note that person-to-person transmission of HFRS is rare and typically occurs in specific circumstances, such as through organ transplantation from an infected donor.
The risk of Hantavirus exposure is higher in areas where rodents are prevalent, such as rural or agricultural settings. Factors that contribute to increased transmission risk include inadequate sanitation, poor waste management, and close proximity to rodent habitats. Individuals involved in activities that bring them into contact with rodents, such as farming, forestry, or cleaning barns and outbuildings, are at greater risk of HFRS infection.
Occupational exposure to rodents, particularly in industries that involve working with livestock or crops, poses a significant risk of Hantavirus transmission. Health care workers caring for HFRS patients are also at risk of infection if proper infection control measures are not followed. Understanding the routes of transmission and implementing preventive strategies are essential in reducing the burden of HFRS in at-risk populations.
Preventive measures aimed at reducing the risk of HFRS transmission include practicing proper hygiene, using personal protective equipment when handling rodents or cleaning contaminated areas, and implementing rodent control measures. Effective rodent control strategies may involve sealing entry points to buildings, removing potential food sources for rodents, and maintaining a clean environment to deter rodent infestations.
Public health initiatives focused on raising awareness about the risks of HFRS and educating the public on preventive practices can play a crucial role in reducing the incidence of Hantavirus infections. By addressing the transmission pathways and implementing targeted prevention measures, the spread of HFRS can be mitigated, ultimately protecting individuals from this potentially serious viral illness.
Symptoms of HFRS
Hemorrhagic Fever with Renal Syndrome (HFRS) presents with a range of symptoms that can vary in severity depending on the specific Hantavirus strain causing the infection. The most common initial symptoms of HFRS include fever, headache, and muscle aches, which can progress to more severe manifestations as the disease advances.
One of the hallmark symptoms of HFRS is back pain, which is often severe and localized in the lower back region. Patients may also experience abdominal pain, typically in the upper abdomen, which can be accompanied by gastrointestinal symptoms such as nausea, vomiting, and diarrhea. As the disease worsens, individuals may develop petechiae (small red or purple spots under the skin) due to abnormal blood clotting.
HFRS can also lead to renal complications, with affected individuals experiencing decreased urine output, fluid retention, and electrolyte imbalances. The renal involvement in HFRS can progress to acute kidney injury (AKI), necessitating medical intervention such as dialysis in severe cases; Additionally, changes in blood pressure, ranging from hypotension to hypertension, may occur as a result of the viral infection.
In more severe cases of HFRS, patients may develop hemorrhagic manifestations, including bleeding from mucous membranes, gastrointestinal bleeding, and hemoptysis (coughing up blood). The presence of these hemorrhagic symptoms signifies a more critical stage of the disease and warrants immediate medical attention.
As the disease progresses, individuals with HFRS may develop complications related to multi-organ dysfunction, including respiratory distress, liver failure, and shock. Neurological symptoms such as confusion, seizures, and coma can also occur in severe cases of HFRS, indicating widespread viral involvement and systemic inflammation.
Early recognition of the symptoms of HFRS is crucial for timely diagnosis and management of the disease. Medical evaluation should be sought if any of the aforementioned symptoms are present, especially in individuals with a history of rodent exposure or living in endemic regions where Hantaviruses circulate. Prompt medical intervention can help improve outcomes and reduce the risk of complications associated with HFRS.
Diagnosis and Treatment
Diagnosing Hemorrhagic Fever with Renal Syndrome (HFRS) involves a combination of clinical assessment, laboratory tests, and imaging studies to confirm the presence of the viral infection and assess the severity of the disease. Patients presenting with symptoms suggestive of HFRS, such as fever, headache, back pain, and renal dysfunction, should undergo diagnostic evaluation promptly.
Laboratory tests play a vital role in the diagnosis of HFRS, with serological assays detecting specific antibodies against Hantaviruses and polymerase chain reaction (PCR) tests identifying viral genetic material in blood or tissue samples. These tests help differentiate HFRS from other febrile illnesses and confirm the presence of Hantavirus infection.
Imaging studies, such as renal ultrasound or abdominal computed tomography (CT) scans, may be performed to evaluate renal involvement and assess the extent of organ damage in patients with HFRS. These imaging modalities can provide valuable information to guide treatment decisions and monitor disease progression.
The treatment of HFRS primarily focuses on supportive care to manage symptoms, prevent complications, and promote recovery. Supportive measures include fluid resuscitation to maintain adequate hydration, pain management to alleviate discomfort, and hemodynamic support to stabilize blood pressure and prevent shock.
Antiviral medications may be considered in certain cases of HFRS to reduce viral replication and improve clinical outcomes. However, the use of antivirals in HFRS remains a subject of ongoing research, and their efficacy in treating the disease is not yet fully established. Medical professionals will determine the appropriateness of antiviral therapy based on individual patient factors and disease severity.
In cases of severe HFRS with renal failure, dialysis may be required to support kidney function and manage electrolyte imbalances until renal function improves. Dialysis helps remove waste products from the blood and maintain fluid and electrolyte balance, promoting recovery in patients with acute kidney injury.
Monitoring for complications of HFRS, such as acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), and neurological dysfunction, is essential during treatment. Early detection and intervention for these complications can improve patient outcomes and reduce the risk of long-term sequelae associated with severe HFRS.
Overall, a multidisciplinary approach involving healthcare providers from various specialties, including infectious disease specialists, nephrologists, and critical care physicians, is crucial in the comprehensive management of HFRS. Close monitoring, timely intervention, and individualized treatment strategies can maximize the chances of recovery and minimize the impact of this potentially life-threatening viral infection.
Complications and Dialysis
Hemorrhagic Fever with Renal Syndrome (HFRS) can lead to a variety of complications, both during the acute phase of the illness and in the recovery period. These complications can range from renal dysfunction and hemorrhagic manifestations to more severe conditions affecting multiple organ systems.
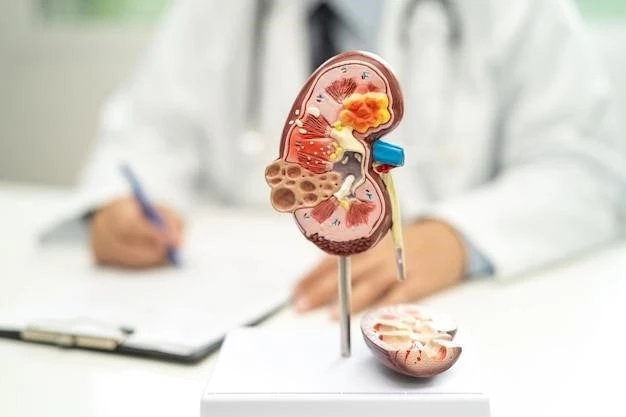
One of the most common complications of HFRS is acute kidney injury (AKI), which can result from the direct viral effects on the kidneys or as a consequence of the body’s immune response to the infection. AKI in HFRS can lead to decreased urine output, electrolyte imbalances, and the accumulation of waste products in the blood, necessitating medical intervention such as dialysis.
Dialysis is a crucial therapeutic modality in the management of severe cases of HFRS with renal failure. It involves the use of a machine to perform the functions of the kidneys, including filtering waste products and excess fluids from the blood. By undergoing dialysis, patients with HFRS-induced AKI can maintain electrolyte balance, control fluid accumulation, and support kidney function while the body recovers.
In addition to renal complications, HFRS can result in hemorrhagic manifestations such as petechiae, ecchymoses (bruises), and mucosal bleeding. These symptoms reflect abnormalities in the blood clotting process and can lead to more serious hemorrhagic conditions if left untreated. Patients with severe bleeding may require blood transfusions and close monitoring to prevent complications.
Complications of HFRS may extend beyond the renal and hematological systems to affect other organs, including the respiratory and central nervous systems. Acute respiratory distress syndrome (ARDS) can develop in patients with severe HFRS, leading to respiratory failure and necessitating advanced respiratory support measures in an intensive care setting.
Neurological complications, such as encephalitis, seizures, and coma, can also occur in some individuals with HFRS, particularly in cases of severe systemic involvement. Prompt recognition and management of these neurological manifestations are essential to prevent long-term neurological sequelae and improve patient outcomes.
Complications of HFRS highlight the importance of early diagnosis, prompt intervention, and comprehensive management to address the diverse array of clinical manifestations associated with the disease. Through close monitoring, targeted therapeutic interventions, and supportive care measures, healthcare providers can mitigate the impact of complications, improve patient outcomes, and enhance the prospects of recovery in individuals affected by HFRS.
Prevention of HFRS
Preventing Hemorrhagic Fever with Renal Syndrome (HFRS) focuses on strategies aimed at reducing human exposure to Hantaviruses carried by rodents and minimizing the risk of infection. Implementing effective preventive measures is essential in endemic regions or areas where rodents are prevalent to safeguard public health and prevent the transmission of HFRS.
One of the key strategies in preventing HFRS is rodent control. This involves minimizing the presence of rodents in and around living spaces, workplaces, and recreational areas by employing measures such as sealing entry points, eliminating food sources, and maintaining proper sanitation practices. By reducing the rodent population, the risk of human exposure to Hantaviruses is significantly decreased.
Education and raising awareness about HFRS and its transmission pathways are essential components of preventive efforts. Public health campaigns can provide information on the risks associated with rodent contact, proper hygiene practices, and the importance of promptly reporting rodent infestations. Targeted educational initiatives help empower individuals to take proactive steps in preventing HFRS.
Individuals living in or visiting endemic regions where Hantaviruses are known to circulate should take precautions to minimize their risk of exposure. This includes avoiding direct contact with rodents, their droppings, and nesting materials, especially in areas where rodents are likely to inhabit, such as barns, sheds, and fields. Wearing gloves and masks when cleaning potentially contaminated areas can further reduce the risk of infection.
Occupational groups at higher risk of HFRS, such as farmers, forestry workers, and cleaning personnel, should follow specific safety guidelines to prevent exposure to Hantaviruses. Employers can implement workplace policies that promote rodent control, provide personal protective equipment, and offer training on infection prevention measures to protect workers from occupational hazards.
In some endemic regions, vaccination strategies may be considered as part of public health interventions to reduce the incidence of HFRS. Vaccines against specific Hantavirus strains have been developed in certain countries and may be recommended for individuals at high risk of exposure, such as research personnel working with infected rodents or individuals residing in areas with a history of HFRS outbreaks.
Community-based initiatives, collaborations between healthcare providers and public health agencies, and integrated surveillance systems play a crucial role in the prevention of HFRS. By fostering multidisciplinary approaches to address the environmental, clinical, and public health aspects of HFRS, communities can effectively mitigate the risk of Hantavirus transmission and protect individuals from this potentially severe viral infection.
Conclusion
In conclusion, Hemorrhagic Fever with Renal Syndrome (HFRS) poses a significant public health concern worldwide, particularly in regions where Hantaviruses are endemic. This viral disease, transmitted through rodents and their excreta, can lead to a spectrum of clinical manifestations ranging from mild flu-like symptoms to severe hemorrhagic fever and renal failure.
Early recognition of the symptoms of HFRS, prompt diagnosis, and timely initiation of appropriate treatment are essential in managing the disease and preventing complications. Healthcare providers play a crucial role in caring for individuals affected by HFRS, delivering supportive care, monitoring for complications, and providing interventions such as dialysis when necessary.
Prevention strategies targeting rodent control, public education, and vaccination programs are fundamental in reducing the incidence of HFRS and limiting the spread of Hantaviruses. By employing a combination of preventive measures at the individual, community, and healthcare system levels, the burden of HFRS on public health can be mitigated.
As research continues to advance our understanding of HFRS and the associated Hantaviruses, ongoing efforts in surveillance, diagnostics, and treatment development are vital in addressing the challenges posed by this complex viral infection. By fostering collaborations between researchers, healthcare professionals, and public health authorities, we can work towards effectively preventing, diagnosing, and managing HFRS.
Ultimately, a comprehensive approach that integrates prevention, early detection, and multidisciplinary care is key to combating HFRS and safeguarding the well-being of individuals at risk of Hantavirus exposure. Through continued vigilance, education, and research, we can strive to reduce the impact of HFRS on communities and promote a healthier, resilient population in the face of emerging infectious diseases.