Article Plan⁚ Disease ⸺ Primary Biliary Cirrhosis

Overview of Primary Biliary Cirrhosis
Primary biliary cholangitis (PBC), previously known as primary biliary cirrhosis, is an autoimmune disease that leads to the slow destruction of intrahepatic bile ducts. This condition causes inflammation and cholestasis, eventually progressing to cirrhosis and portal hypertension. PBC is more common in middle-aged women and is characterized by the immune system targeting the bile ducts, resulting in liver damage.
In PBC, the small bile ducts of the liver are slowly damaged, leading to the accumulation of bile and toxins within the liver, a process known as cholestasis. Over time, this damage can escalate, causing scarring, fibrosis, and ultimately cirrhosis. The condition affects the liver’s ability to function properly and can lead to complications like liver failure.
Understanding the progression of PBC to cirrhosis is crucial for early detection and intervention. It is essential for individuals, especially middle-aged women, to be aware of the symptoms, risk factors, and diagnostic methods associated with this disease. Seeking medical advice for timely diagnosis and treatment is vital in managing PBC and preventing its progression to advanced stages.
By staying informed about PBC and its implications on liver health, individuals can actively engage in preventive measures and adopt healthy lifestyle choices to support liver function. Regular monitoring, following medical recommendations, and adhering to treatment plans can significantly impact the progression of primary biliary cholangitis and improve overall quality of life.
Causes and Risk Factors
Primary biliary cholangitis (PBC), formerly known as primary biliary cirrhosis, is primarily characterized by the autoimmune destruction of bile ducts in the liver. The exact cause of this condition remains unknown, but various factors may contribute to its development. Genetics may play a role as PBC tends to run in families, suggesting a genetic predisposition.
Environmental factors like infections or exposure to certain toxins may trigger the autoimmune response that leads to PBC. Additionally, hormonal factors could potentially influence the higher prevalence of this condition in middle-aged women. Hormonal changes during menopause or pregnancy may impact the immune system’s response, increasing the risk of developing PBC.
Individuals with other autoimmune diseases, such as rheumatoid arthritis or Sjögren’s syndrome, have a higher risk of developing PBC. This suggests a potential link between different autoimmune conditions. Moreover, age and gender are significant risk factors, with middle-aged women being more commonly affected by PBC.
Understanding the potential causes and risk factors associated with PBC is crucial for early detection and intervention. While the exact mechanisms triggering the autoimmune response in PBC are still being researched, recognizing these risk factors can aid in proactive management of the condition and fostering better liver health.
Symptoms and Diagnosis
Primary biliary cholangitis (PBC) presents with various symptoms that may indicate liver dysfunction. Common early symptoms include fatigue, itching, and dry eyes or mouth. As the disease progresses, individuals may experience abdominal discomfort, jaundice, and fluid retention.
Diagnosing PBC involves a combination of medical history review, physical examination, and specific blood tests to assess liver function and autoantibodies associated with the disease. Liver biopsy may also be performed to confirm the diagnosis and evaluate the extent of liver damage caused by PBC.
Early detection of PBC is crucial for timely intervention and management to prevent further liver damage and progression to cirrhosis. Individuals experiencing persistent symptoms should consult a healthcare provider for a comprehensive evaluation and appropriate diagnostic tests.
Monitoring liver function through regular check-ups is essential for individuals at risk of PBC, especially middle-aged women, to detect the disease in its early stages. By understanding the symptoms and diagnostic procedures related to PBC, individuals can proactively address their liver health and seek necessary medical care for optimal management of the condition.
Progression to Cirrhosis
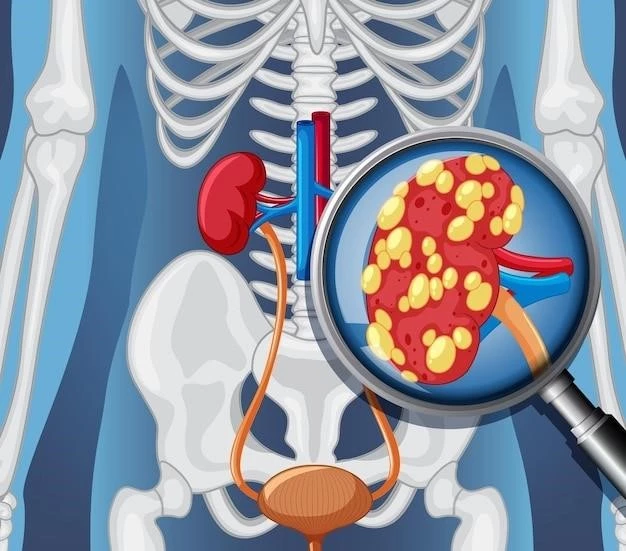
Primary biliary cholangitis (PBC) is a chronic liver disease that can progress to cirrhosis if left untreated. The gradual destruction of intrahepatic bile ducts in PBC leads to inflammation, cholestasis, and scarring of the liver tissue over time, ultimately resulting in cirrhosis and portal hypertension.
It is essential for individuals with PBC to undergo regular monitoring and adhere to treatment plans to prevent the progression to cirrhosis. Early intervention, such as lifestyle modifications and medications, can help slow down the disease’s advancement and reduce the risk of complications associated with cirrhosis.
Monitoring liver function tests and seeking medical advice for any concerning symptoms are crucial steps in managing PBC and preventing the development of cirrhosis. By staying informed about the progression from PBC to cirrhosis and actively engaging in recommended treatments, individuals can better safeguard their liver health and overall well-being.
Treatment Options
Treatment options for primary biliary cholangitis (PBC) aim to manage symptoms, slow disease progression, and prevent complications like cirrhosis and liver failure. The primary treatment for PBC is ursodeoxycholic acid, which can help improve liver function and decrease bile accumulation. Ursodeoxycholic acid is often prescribed to individuals diagnosed with PBC to support liver health and slow the autoimmune response.
In cases where ursodeoxycholic acid is ineffective or if PBC progresses to advanced stages, other medications such as obeticholic acid may be considered. Obeticholic acid can be used in combination with ursodeoxycholic acid to further alleviate symptoms and protect liver function. It is essential for individuals with PBC to work closely with healthcare providers to determine the most suitable treatment plan based on their condition’s severity and response to medications.
Regular monitoring of liver function tests is crucial to assess treatment efficacy and disease progression. Individuals with PBC should also prioritize lifestyle modifications such as maintaining a healthy diet, avoiding alcohol consumption, and staying physically active to promote overall liver health. In some cases, liver transplantation may be necessary for individuals with advanced cirrhosis due to PBC.
By actively engaging in treatment plans, making lifestyle changes, and following medical recommendations, individuals with PBC can better manage their condition, improve liver function, and enhance their quality of life. Seeking ongoing care and staying informed about the latest advancements in PBC treatment can significantly impact the disease’s prognosis and long-term outcomes.
Complications of Primary Biliary Cirrhosis
Primary biliary cholangitis (PBC) can lead to various complications, with one of the most concerning outcomes being the development of cirrhosis. Cirrhosis is a late-stage liver disease characterized by irreversible scarring of the liver tissue. As PBC progresses, the accumulation of bile and inflammation in the liver can lead to fibrosis and cirrhosis over time.
In addition to cirrhosis, individuals with PBC may experience complications such as portal hypertension, which occurs when there is increased pressure in the portal vein that carries blood from the digestive organs to the liver. This can lead to serious issues like variceal bleeding and ascites, the accumulation of fluid in the abdomen;
Furthermore, PBC can increase the risk of hepatocellular carcinoma, a type of liver cancer. Regular monitoring and early intervention are key to managing PBC and preventing these complications. Healthcare providers may recommend specific treatments or interventions to address cirrhosis, portal hypertension, and other associated health issues resulting from advanced PBC.
Individuals with PBC should prioritize regular medical assessments and follow-ups to monitor their liver health and address any emerging complications promptly. By actively participating in their care and adhering to treatment plans, individuals can better manage PBC-related complications, enhance their quality of life, and improve long-term outcomes.
Preventive Measures
Preventing primary biliary cholangitis (PBC) involves adopting healthy lifestyle habits and regular medical follow-ups to support liver health and reduce the risk of disease progression. Individuals at risk for PBC, especially middle-aged women, should prioritize the following preventive measures⁚
- Healthy Diet⁚ Maintain a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to promote liver function and overall well-being.
- Regular Exercise⁚ Engage in physical activity regularly to support metabolism, weight management, and liver health.
- Avoid Alcohol⁚ Limit alcohol consumption or abstain from it entirely to prevent additional stress on the liver.
- Quit Smoking⁚ Tobacco use can exacerbate liver damage, so quitting smoking is essential for liver health.
- Monitoring⁚ Individuals with a family history of PBC or autoimmune diseases should undergo regular check-ups and screenings to detect any signs of the condition early.
- Early Intervention⁚ Seek medical advice promptly if experiencing symptoms related to liver dysfunction to facilitate early diagnosis and treatment.
By proactively engaging in these preventive measures, individuals can reduce the likelihood of developing PBC or slow its progression if already diagnosed. Consulting with healthcare providers, following a tailored health plan, and staying informed about liver health are essential steps in mitigating the impact of PBC and maintaining overall wellness.
Impact on Middle-Aged Women
Primary biliary cholangitis (PBC), also known as primary biliary cirrhosis, predominantly affects middle-aged women, with a higher prevalence in this demographic group. The exact reasons for the increased susceptibility of middle-aged women to PBC remain under study, but hormonal factors, genetic predisposition, and immune system differences may play a role.
Research indicates that women are more commonly diagnosed with PBC than men, with approximately 65 out of every 100,000 women in the United States affected by the disease. Due to the chronic nature of PBC and its potential progression to cirrhosis, it is vital for middle-aged women to be aware of the symptoms, risk factors, and diagnostic procedures associated with the condition.
Early detection and proactive management of PBC are crucial in mitigating the impact of the disease and preventing complications such as advanced liver damage and liver failure. Middle-aged women should prioritize regular health check-ups, follow a healthy lifestyle, and seek medical advice if experiencing any symptoms related to liver dysfunction to ensure timely diagnosis and treatment.
Research and Development Updates
Research and development in the field of primary biliary cirrhosis (PBC) focus on understanding the underlying mechanisms of the disease, identifying new treatment approaches, and improving patient outcomes. Recent studies have highlighted various advancements in the management of PBC⁚
- Elafibranor⁚ Clinical trials have shown that elafibranor, under development by pharmaceutical companies, could significantly improve serum markers of cholestasis in PBC patients, offering potential benefits in disease management.
- Fibrates⁚ For individuals with PBC who do not respond adequately to standard therapy with ursodeoxycholic acid, fibrates have demonstrated promise as adjunctive treatment options to mitigate disease progression.
- RhuDex⁚ MediGene is advancing the clinical development of RhuDex, a drug in Phase II trials for PBC, indicating ongoing research efforts to expand treatment options and enhance therapeutic outcomes for patients.
- Sarcopenia Study⁚ Research studies have explored the prevalence of sarcopenia and its impact on prognoses in PBC patients, shedding light on the importance of addressing comorbidities to optimize disease management.
These developments underscore the commitment of the scientific community to enhance the understanding and treatment of PBC, offering hope for improved care strategies and better outcomes for individuals affected by this chronic liver disease. Continued research into novel therapeutic agents and personalized approaches is essential for advancing the field and ultimately benefiting patients with PBC.