Understanding Hydrocephaly Corpus Callosum Agenesis Diaphragmatic Hernia
Hydrocephalus is a neurological condition characterized by an abnormal buildup of cerebrospinal fluid in the brain’s ventricles. Corpus callosum agenesis is a congenital brain abnormality where the corpus callosum is partially or completely missing. Diaphragmatic hernia is a developmental anomaly affecting the diaphragm. This article will delve into the diagnosis, treatment, complications, and surgical procedures associated with these conditions.
Introduction to Hydrocephaly, Corpus Callosum Agenesis, and Diaphragmatic Hernia
Hydrocephalus is a condition that results from an imbalance between the production and absorption of cerebrospinal fluid in the brain, leading to an enlargement of the brain’s ventricles. This abnormal accumulation of fluid can exert pressure on the brain, causing damage to the delicate brain tissue. It can be congenital or acquired, with varying underlying causes.
Corpus callosum agenesis is a rare congenital condition where the corpus callosum, the structure that connects the brain’s two hemispheres, fails to develop fully or at all. This can lead to a range of neurological abnormalities depending on the extent of the agenesis. Individuals with this condition may experience developmental delays, intellectual disabilities, and seizures.
Diaphragmatic hernia is a developmental anomaly where there is an opening in the diaphragm, the muscle that separates the chest cavity from the abdomen. This opening allows abdominal organs to move into the chest cavity, potentially affecting lung development and function. It can occur on one side (asymmetric) or both sides (congenital diaphragmatic hernia), leading to respiratory distress and other complications.
These conditions, though distinct in nature, can impact individuals in profound ways, affecting their neurological development, respiratory function, and overall quality of life. Understanding the underlying causes, diagnostic approaches, treatment options, and potential complications associated with hydrocephalus, corpus callosum agenesis, and diaphragmatic hernia is crucial for healthcare professionals, patients, and their families.
Understanding Hydrocephalus
Hydrocephalus is a neurological condition characterized by the abnormal accumulation of cerebrospinal fluid within the brain’s ventricles. This buildup of fluid can increase pressure inside the skull, leading to potential damage to the brain tissue. The condition can be congenital, meaning present at birth, or acquired later in life due to factors like tumors, infections, or bleeding in the brain.
The cerebrospinal fluid, a clear liquid that surrounds and cushions the brain and spinal cord, is typically produced within the brain’s ventricles; In a healthy individual, this fluid circulates and is reabsorbed, maintaining a balanced flow. However, in hydrocephalus, there is an imbalance between the production and absorption of this fluid, resulting in its accumulation.
Common causes of hydrocephalus include blockages that prevent the normal flow of cerebrospinal fluid, overproduction of the fluid, or issues with its absorption. Congenital hydrocephalus can be associated with birth defects impacting the development of the brain’s ventricular system. Acquired hydrocephalus may result from conditions such as meningitis, traumatic brain injury, or brain tumors.
Symptoms of hydrocephalus can vary depending on age and the progression of the condition. Infants may present with a rapid increase in head size, vomiting, irritability, and downward deviation of the eyes (‘sunsetting’). In older children and adults, symptoms can include headaches, nausea, blurred vision, difficulty walking, cognitive impairment, and incontinence.
Diagnosis of hydrocephalus typically involves imaging studies such as ultrasound, MRI, or CT scans to visualize the ventricles and assess the flow of cerebrospinal fluid. Treatment often involves surgical interventions, with the placement of a shunt being a common approach. A shunt is a thin tube that helps drain the excess fluid from the brain to another part of the body where it can be reabsorbed, relieving pressure on the brain.
Corpus Callosum Agenesis⁚ Congenital Brain Abnormality
Corpus callosum agenesis is a rare congenital condition characterized by the partial or complete absence of the corpus callosum, the structure that allows communication between the brain’s two hemispheres. This crucial brain region plays a vital role in integrating motor, sensory, and cognitive functions.
The absence of the corpus callosum can lead to a spectrum of neurological abnormalities and developmental disabilities. Individuals with complete agenesis may exhibit more severe symptoms compared to those with partial agenesis. Some common manifestations of corpus callosum agenesis include delayed developmental milestones, intellectual disabilities, challenges with coordination and motor skills, and behavioral issues.
Diagnosing corpus callosum agenesis often involves neuroimaging studies such as MRI or CT scans to visualize the brain structures. Additional assessments may include developmental evaluations and genetic testing to identify any underlying causes or associated syndromes. Early detection of this condition is vital for initiating appropriate interventions and support services.
Management of corpus callosum agenesis focuses on addressing the specific needs and challenges faced by each individual. This may involve early intervention programs to support developmental delays, speech and occupational therapy to improve communication and motor skills, and educational accommodations to optimize learning opportunities.
While there is no cure for corpus callosum agenesis, a multidisciplinary approach involving healthcare providers, educators, therapists, and families can help individuals with this condition lead fulfilling lives. Research into the underlying genetic and neurological factors contributing to corpus callosum agenesis continues to advance our understanding of this complex brain abnormality.
Diaphragmatic Hernia⁚ Developmental Anomaly
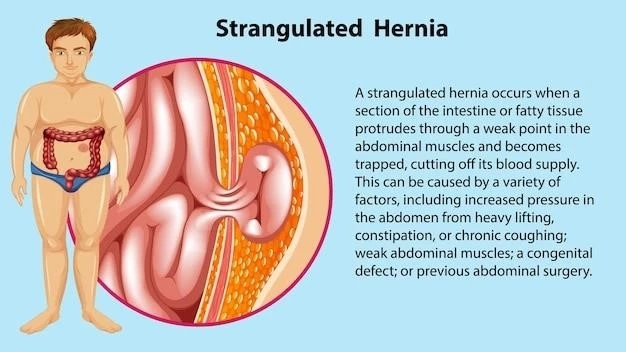
Diaphragmatic hernia is a developmental anomaly characterized by a defect in the diaphragm, the muscle that separates the chest cavity from the abdomen. This opening in the diaphragm allows abdominal organs, such as the stomach, intestines, or liver, to migrate into the chest cavity, putting pressure on the lungs and potentially hindering their proper development.
There are two main types of diaphragmatic hernia⁚ congenital diaphragmatic hernia (CDH) and hiatal hernia. CDH occurs during fetal development when the diaphragm fails to fully close, leading to the displacement of abdominal organs. Hiatal hernia, on the other hand, typically occurs later in life when the stomach protrudes through the diaphragm into the chest cavity.
Infants born with CDH may experience respiratory distress shortly after birth due to the compression of the lungs by displaced abdominal organs. This can lead to breathing difficulties, cyanosis (bluish discoloration of the skin), and other life-threatening complications. Diagnosis is usually confirmed through imaging studies such as ultrasound or MRI.
Treatment for diaphragmatic hernia often involves surgical repair to close the hole in the diaphragm and reposition the misplaced organs back into the abdominal cavity. In cases of severe CDH where lung development is compromised, neonatal intensive care and respiratory support may be necessary to stabilize the infant’s condition.
Long-term outcomes for individuals with diaphragmatic hernia can vary depending on the severity of the condition and associated complications. Some individuals may experience respiratory issues, gastrointestinal problems, or developmental delays. Regular monitoring by healthcare providers is essential to address any ongoing concerns and provide appropriate interventions.
Research into the genetic and environmental factors contributing to diaphragmatic hernia is ongoing, aiming to improve diagnostic techniques, surgical outcomes, and long-term management strategies for individuals affected by this developmental anomaly.
Diagnosis of Hydrocephaly Corpus Callosum Agenesis Diaphragmatic Hernia
Diagnosing hydrocephalus typically involves a combination of imaging studies, physical examinations, and neurological assessments. Imaging techniques such as ultrasound, MRI, or CT scans are used to visualize the brain’s ventricles and assess the flow of cerebrospinal fluid. Neurological examinations help evaluate symptoms such as headaches, cognitive issues, and difficulty walking.
Corpus callosum agenesis is often diagnosed through neuroimaging studies, which can reveal the absence or underdevelopment of the corpus callosum. Additional evaluations such as genetic testing may be recommended to identify any associated syndromes or underlying genetic causes. Developmental assessments play a crucial role in understanding the impact of agenesis on cognitive and motor functions.
Diaphragmatic hernia diagnosis involves a combination of imaging tests like ultrasound, X-rays, or CT scans to visualize the diaphragm and identify any abdominal organs that have moved into the chest cavity. Respiratory distress in infants may prompt further investigations to confirm the presence of a hernia and assess its severity.
Serial monitoring of fetal development through ultrasound examinations can aid in the early detection of congenital anomalies such as hydrocephalus, corpus callosum agenesis, or diaphragmatic hernia. Timely and accurate diagnosis of these conditions is crucial for initiating appropriate medical interventions and supportive care to optimize outcomes for affected individuals.
Treatment Approaches for the Conditions
The treatment of hydrocephalus often involves surgical intervention to alleviate the buildup of cerebrospinal fluid in the brain. One common approach is the placement of a shunt system, which consists of a thin tube that helps drain excess fluid from the brain’s ventricles to another part of the body where it can be reabsorbed. Shunt systems play a crucial role in managing hydrocephalus and reducing intracranial pressure.
Corpus callosum agenesis does not have a specific cure, so treatment focuses on addressing the symptoms and complications associated with the condition. Early intervention programs, educational support, speech therapy, and occupational therapy can help individuals with agenesis develop essential skills and improve their quality of life.
Diaphragmatic hernia treatment often involves surgical repair to close the opening in the diaphragm and reposition any displaced organs. In cases of congenital diaphragmatic hernia, neonatal intensive care and respiratory support may be necessary to stabilize the infant’s condition and address any breathing difficulties resulting from lung compression.
Each of these conditions requires a tailored treatment approach to address the diverse needs of affected individuals. Multidisciplinary teams consisting of neurosurgeons, pediatricians, geneticists, therapists, and other healthcare professionals collaborate to create comprehensive treatment plans that consider the unique challenges posed by hydrocephalus, corpus callosum agenesis, and diaphragmatic hernia.
Long-term management may include regular monitoring, rehabilitative therapy, educational support, and interventions to address any complications or developmental delays associated with these conditions. By providing personalized care and support, healthcare providers strive to enhance the quality of life and well-being of individuals living with these complex medical conditions.
Complications Associated with Hydrocephaly Corpus Callosum Agenesis Diaphragmatic Hernia
Hydrocephalus can lead to various complications if left untreated or inadequately managed. Increased intracranial pressure due to the accumulation of cerebrospinal fluid can result in symptoms such as severe headaches, nausea, vomiting, cognitive impairments, vision problems, and gait disturbances. In infants, untreated hydrocephalus can lead to developmental delays and permanent brain damage.
Complications of corpus callosum agenesis may include intellectual disabilities, challenges with communication and social interactions, motor coordination issues, and behavioral difficulties. The absence or malformation of the corpus callosum can impact the integration of sensory information between the brain hemispheres, leading to a range of neurological symptoms.
Diaphragmatic hernia complications can vary depending on the severity of the condition and associated factors. Respiratory distress is a common complication in infants with diaphragmatic hernia, as lung compression by abdominal organs can impair breathing function. Long-term respiratory issues, gastroesophageal reflux, and developmental delays may also arise in affected individuals.
Early detection, timely intervention, and ongoing monitoring are essential to mitigate the risk of complications associated with hydrocephalus, corpus callosum agenesis, and diaphragmatic hernia. Healthcare professionals work closely with patients and their families to provide comprehensive care, address potential challenges, and minimize the impact of these complex medical conditions on overall health and well-being.
Surgical Procedures for Hydrocephaly and Diaphragmatic Hernia
Surgical intervention plays a key role in the management of hydrocephalus and diaphragmatic hernia, addressing the underlying causes and reducing associated complications. In the case of hydrocephalus, one common surgical procedure is the placement of a ventriculoperitoneal shunt. This shunt system diverts excess cerebrospinal fluid from the brain’s ventricles to the abdominal cavity, where it can be reabsorbed.
Shunt revisions may be necessary in individuals with hydrocephalus to ensure proper drainage and prevent complications such as shunt malfunction, infection, or blockage. Regular follow-up appointments with a neurosurgeon are essential to monitor shunt function and adjust treatment as needed based on the individual’s symptoms and imaging studies.
For diaphragmatic hernia, surgical repair is often performed in neonates or infants to close the opening in the diaphragm and position any displaced organs back into the abdominal cavity. This procedure aims to restore proper organ placement, relieve lung compression, and improve respiratory function in individuals with congenital diaphragmatic hernia.
In cases where diaphragmatic hernia results in long-term respiratory issues or complications, additional surgical interventions or respiratory support may be required to manage breathing difficulties effectively. Multidisciplinary teams consisting of pediatric surgeons, neonatologists, respiratory therapists, and other specialists collaborate to provide comprehensive care and ensure optimal outcomes for affected individuals.
Surgical procedures for hydrocephalus and diaphragmatic hernia are tailored to the individual’s specific needs, medical history, and the severity of the condition. By addressing the underlying anatomical abnormalities and alleviating associated complications through surgery, healthcare providers aim to improve the quality of life and long-term prognosis for patients with these complex medical conditions.
Understanding the Role of the Brainstem, Cerebellum, and Ventricles
The brainstem, located at the base of the brain, plays a critical role in regulating essential functions such as breathing, heart rate, and consciousness. It serves as a bridge connecting the cerebrum to the spinal cord and controls basic autonomic functions necessary for survival. Damage to the brainstem can have profound implications on vital processes and may result in severe neurological deficits.
The cerebellum, situated underneath the cerebrum, is responsible for coordinating movement, balance, and muscle tone. It plays a crucial role in fine motor control and ensuring smooth, coordinated movements. Individuals with abnormalities in the cerebellum, such as those with corpus callosum agenesis, may experience challenges with balance, coordination, and motor skills.
The ventricles of the brain are interconnected cavities filled with cerebrospinal fluid that provide cushioning and support for the brain. These fluid-filled spaces help maintain intracranial pressure, remove waste products, and regulate the chemical environment of the brain. Changes in ventricular size, as seen in hydrocephalus, can impact brain function and lead to neurological symptoms.
Understanding the complex interplay between the brainstem, cerebellum, and ventricles is essential in managing conditions like hydrocephalus, corpus callosum agenesis, and diaphragmatic hernia. Healthcare providers rely on neuroimaging studies, neurological assessments, and multidisciplinary approaches to diagnose and address abnormalities affecting these vital brain structures.
By elucidating the roles of the brainstem in regulating autonomic functions, the cerebellum in coordinating motor activities, and the ventricles in maintaining cerebrospinal fluid balance, researchers and clinicians can develop targeted interventions to optimize patient outcomes and enhance the quality of life for individuals affected by these complex neurological and developmental conditions.